FIGURE 73-1. Structural organization of the human TSH subunit genes and mRNAs. The two panels show the TSHβ (top) and α subunit (bottom) genes. Shown are the relative locations and sizes of the exons and introns. Untranslated regions are shown as open boxes, and protein coding regions are shown in black boxes. The TATA box important for positioning the RNA transcriptional start is located in the promoter close to exon 1. Following transcription, introns are spliced out, exons precisely joined, and a polyA tail added to the 3′ end of the mature mRNA.
DNA sequences close to the transcriptional start site in the promoter of the TSHβ gene contain elements responsible for initiating transcription and regulating expression. A consensus TATA box is located 28 bp upstream of the transcriptional start site and is important for positioning RNA synthesis. Progressive 5′ deletions of the mouse TSHβ promoter linked to a luciferase reporter following expression in thyrotrope cells defined the cis-acting sequences required for expression to the first 270 bp of the promoter.17,18 Although these sequences defined the minimal promoter, other studies have shown that enhancer sequences located more than 6 kb upstream are also required for the promoter to express in pituitary thyrotropes in transgenic mice.19
Promoter deletion studies have demonstrated that the mouse TSHβ promoter from −271 to −80 is sufficient to confer thyrotrope-specific activity,17 and thyrotrope transcription factors can bind to the proximal promoter.20 Within this broad area, four regions of protein interaction have been identified using nuclear extracts from thyrotrope cells.18 Two factors, Pit-1, a homeodomain factor, and Gata2, a zinc finger transcription factor, can bind to TSHβ promoter sequences from −135 to −8821 (Fig. 73-2). Both factors can bind independently to the promoter, form a heteromeric complex with DNA, physically interact with each other, and functionally synergize to activate TSHβ promoter activity. Recently, an additional transcription factor, TRAP220 (Med1, PBP), was shown to be recruited to the TSHβ proximal promoter, where it was shown to play a role in transcriptional activation.22
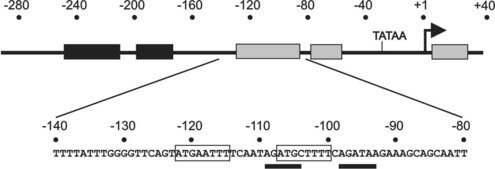
FIGURE 73-2. Functionally important regions of the TSHβ gene promoter. Top, Schematic showing regions (shaded boxes) of the TSHβ promoter that interact with transcription factors present in thyrotrope cells. Below, The DNA sequence of a key region that is critical for high level of TSHβ expression in thyrotropes. Within this region, Pit-1 sites are boxed, and sites interacting with Gata2 are underlined.
TRAP220 was originally defined as part of a transcriptional mediator complex that interacts with hormone-occupied thyroid/steroid hormone receptors.23 Mice with a single copy of this gene were hypothyroid with reduced levels of pituitary TSHβ transcripts.24 TRAP220 is recruited to the TSHβ gene by virtue of its physical interaction with both Pit-1 and Gata2, since the protein itself does not bind DNA. Co-transfections in nonpituitary cells showed that Pit-1, Gata2, or TRAP220 alone could not stimulate the TSHβ promoter. However, maximal activity resulted when all three factors were expressed. Interaction studies showed that all three factors interact with each other in vivo and in vitro. The regions of interaction were important for maximal function. Chromatin immunoprecipitation demonstrated in vivo occupancy on the proximal TSHβ promoter.22 Thus, the TSHβ gene is activated by a unique combination of transcription factors present in pituitary thyrotropes, including those that act via binding to the proximal promoter, as well as others that are recruited to the promoter via protein-protein interactions.
α Subunit Gene Structure
The human glycoprotein hormone α subunit gene is located on chromosome 6 at position 6q12-q21.25 It is present as a single copy gene that is 9635 kb in size and contains four exons and three introns and contains a consensus TATA box located 26 bp upstream of the transcriptional start site.26 The first exon (94 bp) contains 5′-untranslated sequences and is separated from the second exon by a 6.4 kilobase (kb) intron. The second exon contains 7 bp of 5′-untranslated sequence and 88 bp of the coding region. The coding sequence continues in the third (185 bp) and fourth (75 bp) exons, and the 3′-untranslated region (220 bp) is contained within the fourth exon (Fig. 73-1, bottom panel).
The α subunit gene is expressed in thyrotropes, gonadotropes, and placental cells but is differentially regulated. Cell-specific expression in each cell type is dependent on different regions of the promoter. Whereas the region downstream of −200 is sufficient for placental expression,27 gonadotropes require sequences between −225 and −200,28 and regions farther upstream appear to be critical for thyrotrope expression.29 Transgenic mouse studies have shown 480 bp of the mouse α subunit 5′-flanking DNA could target transgenic expression to both gonadotropes and thyrotropes.30 A region from −225 to −200 that binds steroidogenic factor 1 appears to be critical for gonadotrope expression,31 but not for thyrotrope expression.32 Another important sequence involves the pituitary glycoprotein hormone basal element, extending from −342 to −329, that is critical for both thyrotrope and gonadotrope expression.33 The element interacts with P-LIM, a pituitary-specific LIM-homeodomain transcription factor that is important for other pituitary cells.34 Several sequences within the region from −480 to −300 appear to be important for mouse α subunit expression in thyrotropes but not gonadotropes.29 Among these is the sequence from −434 to −421, which interacts with the developmental homeodomain transcription factor Msx1.35 Other sequences within the 480 bp promoter have been found to interact with the pituitary-specific homeodomain factor Ptx-1, and a synergism between Ptx-1 and P-LIM, mediated by the co-activator C-LIM, has been described.36 Recent studies with the mouse promoter in transgenic mice showed that an upstream DNA element located between −4.6 and −3.7 kb further enhanced expression in both thyrotropes and gonadotropes, and contained consensus binding sites for Gata, SF1, Sp1, ETS, and bHLH factors, which suggests cooperativity between factors binding both to proximal cis-acting elements and to the distal enhancer.37
BIOSYNTHESIS OF TSH
The intact TSH molecule is a heterodimeric glycoprotein with a molecular weight of 28 kDa that is composed of the noncovalently linked α and β subunits. The common α subunit contains 92 amino acids, and the specific TSHβ subunit has 118 amino acids. TSH biosynthesis and secretion by thyrotrope cells of the anterior pituitary are precisely regulated events. This section examines our understanding of the biosynthesis of TSH, including the processes of transcription, translation, glycosylation, folding, combination, and storage.
Transcription of TSH Subunit Genes
The DNA information contained in the TSHβ and α subunit genes is transcribed into a precursor RNA by a complex of enzymes, as directed by their respective promoters in the presence of both ubiquitous and specific transcription factors. The transcribed RNAs undergo a precise series of splicing events at the exon-intron junctions that lead to the production of the mature messenger RNA (mRNA) that then exits the nucleus and is translated to protein in the cytoplasm prior to posttranslational modification, subunit association, storage, and finally secretion. Transcription of the TSHβ and α subunit genes is coordinated under the influence of physiologic regulators, the most important of which are T3 and TRH.
Translation of TSH Subunits
The next steps in TSH biosynthesis are summarized in Fig. 73-3.38 The mRNAs for the TSHβ and α subunits are independently translated by ribosomes in the cytoplasm. The first peptide sequences consist of “signal” peptides of 20 amino acids for TSHβ and 24 amino acids for α.39 These signal peptides are hydrophobic, allowing insertion through the lipid bilayer of the membrane of the rough endoplasmic reticulum. Translation into TSHβ and α pre-subunits continues into the lumen of the rough endoplasmic reticulum, and cleavage of the signal peptide occurs before translation is completed. This results in the formation of a 118 amino acid TSHβ subunit40 and a 92 amino acid α subunit. Cleavage of TSHβ to a protein of 112 amino acids appears to be an artifact of purification. Synthesis of recombinant TSHβ subunit has resulted in two products of 112 and 118 amino acids, both of which are similarly active in vitro.41
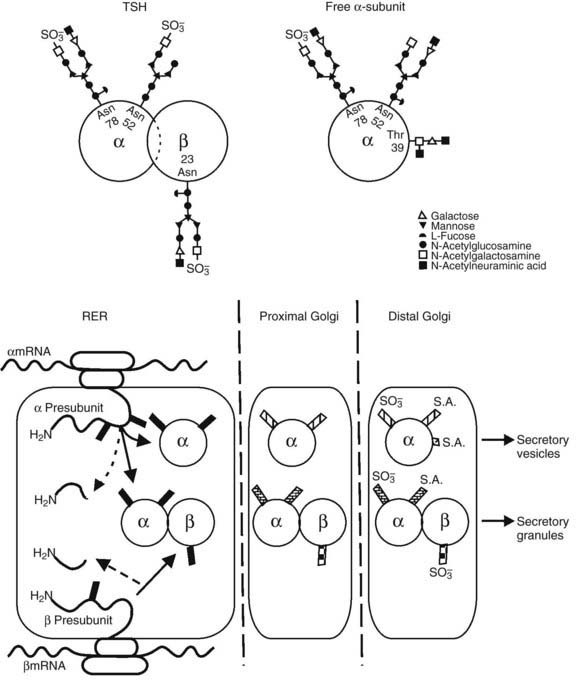
FIGURE 73-3. Top panel, Oligosaccharide chains of thyroid-stimulating hormone (TSH). Shown are typical oligosaccharide chains present on the TSH heterodimer and the free α subunit. Glycosylated asparagine (Asp) and threonine (Thr) residues are indicated. Symbols represent the oligosaccharide chain residues as indicated in the key. Bottom panel, Biosynthesis of thyroid-stimulating hormone (TSH). Schematic shown includes the processes of translation and glycosylation within the rough endoplasmic reticulum (RER) and Golgi apparatus, divided into proximal and distal. Cleavage of the aminoterminal (H2N) signal peptide and early addition of high mannose chains (black boxes), as well as the combination of α and β subunits, occur in the RER. In the proximal Golgi, oligosaccharide chains are modified (shaded boxes), and the final steps of sulfation and sialation occur in the distal Golgi apparatus.
(From Weintraub BD, Gesundheit N: Thyroid-stimulating hormone synthesis and glycosylation: clinical implications. Thyroid Today 10:1–11, 1987.)
Glycosylation of TSH
Glycosylation of TSH has a significant impact on its biological activity.42 The TSHβ subunit has a single glycosylation site, the asparagine residue at position 23, whereas the α subunit is glycosylated in two sites, the asparagine residues at positions 52 and 7843 (see Fig. 73-3). Excess free α subunit is glycosylated at an additional site, the threonine residue at position 39.44 This residue is located in a region believed to be important for combination with the TSHβ subunit. It is not known whether glycosylation at this residue is a regulated step that inhibits combination with the TSHβ subunit, or whether it occurs in excess free α subunits because this site is exposed.
Extensive studies on the processes of TSH subunit glycosylation have been carried out. Glycosylation of the TSHβ and α subunits begins before translation is completed (co-translational glycosylation), and addition of the second oligosaccharide in the α subunit occurs after translation is completed (posttranslational glycosylation). The first step in this process involves the assembly of a 14-residue oligosaccharide, (glucose)3-(mannose)9-(N-acetylglucosamine)2 on a dolichol-phosphate carrier. This oligosaccharide then is transferred to asparagine residues by the enzyme olygosaccharyl transferase, which recognizes the tripeptide sequence (asparagine)-(X)-(serine or threonine).45 This mannose-rich oligosaccharide is progressively cleaved in the rough endoplasmic reticulum and Golgi apparatus. An intermediate with only six residues is produced and then other residues are added, resulting in complex oligosaccharides.46 The residues added include N-acetylglucosamine, fucose, galactose, and N-acetylgalactosamine. Oligosaccharides before the six-residue intermediate are termed high mannose and are sensitive to endoglycosidase H, which releases the oligosaccharide from the protein, whereas the intermediate and complex oligosaccharides are endoglycosidase H resistant. Complex oligosaccharides usually consist of two branches (biantennary), but sometimes three or four branches are seen, as are hybrid oligosaccharides consisting of one complex and another high-mannose branch. Sulfation and sialation occur late in the pathway, within the distal Golgi apparatus. Sulfate is bound to N-acetylgalactosamine residues, and sialic acid, or its precursor N-acetylneuraminic acid, is bound to galactoside residues.47 Thus, activation of the enzymes sulfotransferase and N-acetylgalactosamine transferase may involve important regulatory steps that affect the ratio of sulfate to sialic acid. As demonstrated with LH, it appears that sulfation increases and sialylation decreases the bioactivity of TSH,47 because the exclusively sialylated recombinant glycoprotein produced in Chinese hamster ovary cells has been found to have attenuated activity in vitro.48
Processing of complex oligosaccharides appears to occur at a slower rate for secreted glycoproteins, such as TSH, when compared with that for nonsecreted glycoproteins. For example, after an 11 minute pulse labeling with [35S]methionine and a 30 minute chase, only a few α subunits were endoglycosidase H resistant, and only 76% reached this stage after an 18 hour chase.49 Secretion was observed after a 60 minute chase, and the secreted products—TSH, free α subunit but no free β subunit—had mostly complex oligosaccharides associated with them.43 It may be important to note that many of the studies described were carried out in thyrotropic tumor tissue obtained from hypothyroid mice, and glycosylation may differ in the euthyroid as compared with the hypothyroid state. In addition, differences between species have been noted, such as the human TSH may contain more sialic acid than the bovine TSH.40
Folding, Combination, and Storage of TSH
Elucidation of the crystal structure of human CG (hCG)50 allowed the construction of a model of human TSH, as supported by other evidence.51,52 This model has greatly facilitated the interpretation of structure-function studies of the protein backbone. However, crystallization was achieved only with partly deglycosylated hCG, so it is likely that the conformation of the glycosylated protein may differ to some extent, although nuclear magnetic resonance studies suggest that the α subunit carbohydrate moieties project outward and may be freely mobile.53 Nevertheless, this model predicts that the tertiary structure of each TSH subunit consists of two hairpin loops on one side of a central knot formed by three disulfide bonds and a long loop on the opposite side. In this tertiary structure, the glycoprotein hormones share features in common with transforming growth factor β, nerve growth factor, platelet-derived growth factor, vascular endothelial growth factor, inhibin, and activin, all of which are now grouped in the family of “cystine knot” growth factors.54
Folding of nascent peptides begins before translation is completed. It has been shown that proper folding is dependent on glycosylation, because the drug tunicamycin, which prevents the initial oligosaccharide transfer to the asparagine residue, results in a peptide that does not fold properly and is degraded intracellularly.55 Site-directed mutagenesis of a single glycosylation site also disrupted processing and decreased TSH secretion in transfected Chinese hamster ovary cells.56 Folding is a critical step that allows correct internal disulfide bonding, which stabilizes the tertiary structure of the protein, allowing subunit combination.
Combination of TSH β and α subunits begins soon after translation is completed in the rough endoplasmic reticulum and continues in the Golgi apparatus.43 Subunit combination then accelerates and modifies oligosaccharide processing of the α subunit.57 In fact, studies have suggested that the conformation of the α subunit differs after combination with each type of β subunit,58 and this may affect subsequent processing. The rate of combination of TSHβ and α subunits has been examined in mouse thyrotropic tumors. After a 20 minute pulse labeling with [35S]methionine, 19% of TSHβ subunits were combined with α subunits, and this percentage increased to 61% after a additional 60 minute chase incubation.43 Recent studies have shown that the combination of the TSHβ and α subunits, as is also the case with other glycoprotein hormones, occurs after “latching” of the disulfide “seatbelt” of the β subunit, with subsequent “threading” of loop 2 and the attached oligosaccharide of the α subunit beneath that “seatbelt.”59
The sequence of the TSHβ subunit from amino acid 27 to 31 (CAGYC) is highly conserved among species and is thought to be important for combination with the α subunit. In a case of congenital hypothyroidism, a point mutation in the CAGYC region (see Disorders of TSH Production) results in the synthesis of altered TSHβ subunits that are unable to associate with α subunits, with consequent lack of intact TSH production.60 A lack of free circulating TSHβ subunit was also observed, suggesting that combination with α subunit is necessary for TSHβ subunit secretion. This phenomenon was also demonstrated in studies where synthesis of wild-type recombinant TSHα subunit was carried out in the presence or absence of recombinant β subunit.61 Using site-directed mutagenesis, another study showed that a mutation at residue 25 in the glycosylation recognition site, which substitutes a serine for a threonine, does not alter glycosylation but decreases TSH production by 70%, possibly because of disruption of the nearby CAGYC region.62
After TSH and free α subunit are processed in the distal Golgi apparatus, they are transported into secretory granules or vesicles.63 The secretory granules constitute a regulated secretory pathway, mainly influenced by TRH and other hypothalamic factors. These granules contain mostly TSH, whereas free α subunit is contained in the secretory vesicles that constitute a nonregulated secretory pathway.
TSH SECRETION
In healthy humans, the production rate of TSH is between 100 and 400 mU/day.64,65 The distribution space of TSH is slightly greater than the plasma volume. In euthyroid subjects, the half-life of TSH in plasma is approximately 50 minutes, with a plasma clearance rate of approximately 50 mL/min. In hypothyroid subjects, TSH secretion rates increase by 10 to 15 times normal rates, and the clearance rate decreases slightly. In hyperthyroid subjects, TSH secretion is suppressed, and metabolic clearance is accelerated.
Ontogeny of TSH Levels
At 8 to 10 weeks of gestation in the human, TRH is measurable in the hypothalamus, with progressive increases in TRH levels until term. By 12 weeks of gestation, immunoreactive TSH cells are present in the human pituitary gland,66 and TSH is detectable in the pituitary and the serum.67,68 Serum and pituitary TSH levels remain low until week 18, when TSH levels increase rapidly, followed by increases in serum T4 and T3 concentrations. Fetal serum TSH and T4 concentrations continue to increase between 20 and 40 weeks of gestation. Pituitary TSH begins to respond to exogenous TRH early in the third trimester, and negative feedback control of TSH secretion develops during the last half of gestation and the first 1 to 2 months of life.69
An abrupt rise in serum TSH levels occurs within 30 minutes of birth in term infants. This is followed by an increase in serum T3 concentrations within 4 hours and a lesser increase in T4 levels within the first 24 to 36 hours. The initial increase in serum TSH levels appears to be stimulated by cooling in the extrauterine environment. Serum TSH levels fall to the adult range by 3 to 5 days after birth, and serum thyroid hormone levels stabilize by 1 to 2 months. Serum TSH levels in healthy premature infants (less than 37 weeks gestational age) are highly variable but tend to be lower at birth compared with those of term infants. TSH levels decrease slightly during the first week of life, followed by a gradual increase to normal term levels. Serum TSH levels are even lower in ill premature infants but rise toward normal levels during recovery.70,71
Patterns of TSH Secretion
TSH is secreted from the pituitary gland in a dual fashion, with secretory bursts (pulses) superimposed upon basal (apulsatile) secretion (Fig. 73-4, upper panel). Basal TSH secretion accounts for 30% to 40% of the total amount released into the circulation, and secretory bursts account for the remaining 60% to 70%. TSH pulses occur approximately every 2 to 3 hours, although considerable variability is noted among individuals.72 TSH pulses appear to directly stimulate T3 secretion from the thyroid gland, as cross-correlation analysis has shown that a free T3 peak occurs between 0.5 and 2.5 hours after a TSH peak. However, changes in free T3 levels from nadir to peak are only 11% of mean free T3 levels, probably because T3 has a long serum half-life, and most T3 does not arise from the thyroid gland.73
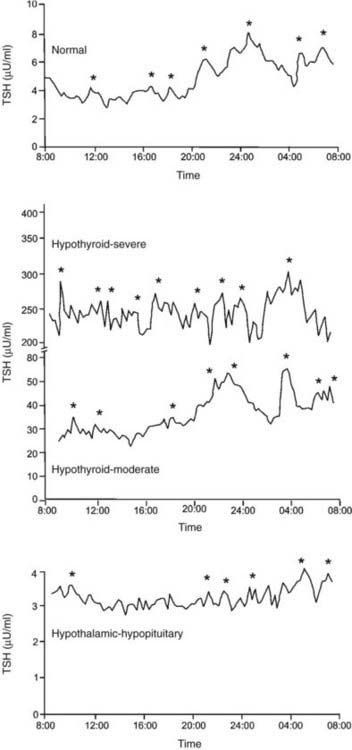
FIGURE 73-4. Serum thyroid-stimulating hormone (TSH) levels measured every 15 minutes in a healthy subject (upper panel), in two subjects with primary hypothyroidism (middle panel), and in a subject with hypothyroidism due to a craniopharyngioma (lower panel). Significant TSH pulses were located by cluster analysis, a computerized pulse detection program, and are indicated by asterisks.
(Data from Sarapura VD, Samuels MH, Ridgway EC: Thyroid-stimulating hormone. In: Melmed S [ed]: The Pituitary, 2nd ed. Blackwell Science, Malden, MA, pp 187–229, 2002.)
In healthy euthyroid subjects, TSH is secreted in a circadian pattern, with nocturnal levels increasing to up to twice daytime levels72 (Fig. 73-4, upper panel). Peak TSH levels occur at between 2300 and 0500 hours in subjects with normal sleep-wake cycles, and nadir levels occur at about 1100 hours. The TSH circadian rhythm is not present in infants younger than 4 weeks old but emerges between 1 and 2 months of life and is well established in healthy children.74 The circadian variation in TSH levels is due to increased mass of TSH secreted per burst at night, as well as slightly increased frequency of bursts and more rapid increase to maximal TSH secretion within a burst.72 The nocturnal increase in TSH levels can precede the onset of sleep, and sleep deprivation enhances TSH secretion. Therefore, in contrast to other pituitary hormones with a circadian variation, the nocturnal rise in TSH levels is not sleep entrained. Instead, a sleep-related inhibition of TSH release is of insufficient magnitude to counteract the nocturnal TSH surge.
Subjects with mild primary hypothyroidism retain the nocturnal rise in TSH levels, and patients with severe primary hypothyroidism have markedly increased TSH pulse amplitude throughout the day with loss of circadian variation in TSH levels (Fig. 73-4, middle panel).72 l-Thyroxine therapy reestablishes the normal TSH circadian variation. In contrast, patients with hypothalamic-pituitary causes of hypothyroidism secrete less TSH over a 24 hour period, with loss of the nocturnal TSH surge in pulse amplitude75 (Fig. 73-4, lower panel). A similar pattern of reduced 24 hour TSH secretion occurs in critical illness.76
The origin of pulsatile and circadian TSH secretion is not known. Thyroid hormones alter TSH pulse amplitude but have little effect on pulse frequency, and therefore are unlikely to participate in TSH pulse generation. The TSH pulse generator may reside in the hypothalamus, with TRH neurons acting in concert to stimulate a burst of TSH secretion from the pituitary gland. However, constant TRH infusions do not change TSH pulse frequency in humans, which casts doubt on this theory.77 Dopamine suppresses TSH pulse amplitude but does not alter TSH pulse frequency, and therefore dopamine does not appear to control pulsatile TSH secretion. A diurnal variation in the activity of anterior pituitary 5′-monodeiodinase in the rat may control circadian TSH secretion.78 However, this has not been confirmed in the human.
Physiologic serum cortisol levels may control circadian TSH secretion, although cortisol does not appear to affect TSH pulse frequency. When subjects with adrenal insufficiency were studied under conditions of glucocorticoid withdrawal, daytime TSH levels were increased, and the usual TSH circadian rhythm was abolished. When these subjects were given physiologic doses of hydrocortisone in a pattern that mimicked normal pulsatile and circadian cortisol secretion, daytime TSH levels were decreased, and the normal TSH circadian rhythm was reestablished. Hydrocortisone infusions at the same dose given as pulses of constant amplitude throughout the 24 hour period also decreased 24 hour TSH levels, but no circadian variation was noted.79 Similarly, when healthy subjects were given metyrapone (an inhibitor of endogenous cortisol synthesis), TSH levels increased during the day, leading to abolition of the usual TSH circadian variation.80 These data suggest that the normal early morning increase in endogenous serum cortisol levels decreases serum TSH levels and leads to the observed normal circadian variation in TSH.
REGULATION OF TSH BIOSYNTHESIS
TSH biosynthesis is regulated by coordinated signals from the central nervous system and feedback from the peripheral circulation. The most important positive input for TSH biosynthesis is hypothalamic TRH, and the most powerful negative regulators are circulating thyroid hormone levels. However, additional hypothalamic factors and circulating hormones have important modifying effects. Most of these factors have independent effects on the biosynthesis of the two subunits of TSH.
Hypothalamic Regulation of TSHβ Subunit Biosynthesis
Thyrotropin-releasing hormone (TRH) is a tripeptide that is secreted from the hypothalamus and transported to the pituitary via the hypothalamic-hypophyseal portal system; it is a major activator of TSH production with a significant three- to fivefold increase in the transcription of both TSHβ and α subunit mRNAs.81 TRH from maternal or fetal sources is not required for normal thyrotrope development during ontogeny, and TRH-deficient mice are not hypothyroid at birth. However, TRH is required for the postnatal maintenance of TSH activation.82
TRH binding to its receptor initiates a cascade of intracellular events. In GH3 cells, the TRH-receptor complex interacts with a guanine nucleotide binding regulatory protein (G) that then binds and activates GTP(G′). G′ binds to phospholipase C (C) and activates it (C′). C′ catalyzes the hydrolysis of phosphatidylinositol 4,5 bisphosphate, which results in the formation of two intracellular “second messengers,” inositol triphosphate (InsP3) and 1,2-diacylglycerol (1,2-DG). InsP3 diffuses from the cell-surface membrane to the endoplasmic reticulum, where it causes the release of sequestered Ca2+. This activates the movement of secretory granules to the cell surface and their exocytosis. Simultaneous with these events is a parallel activation of protein kinase C by 1,2-DG, which also leads to phosphorylation of proteins involved in exocytosis. TRH has been shown to stimulate a nuclear protein, Islet-brain-1 (IB1)/JIP-1, in the anterior pituitary gland and in cultured rat GH3 cells83 and has been implicated in the action of TRH in stimulating the TSHβ gene in thyrotropes. Studies in somatomammotrope cells, where TRH stimulates prolactin production, have suggested that phosphatidylinositol, protein kinase C, and calcium-dependent pathways may be involved,84 although TRH stimulation of the TSHβ subunit promoter may be mediated by AP1.85
Two TRH-response regions are located from −128 to −61 and from −28 to +8 of the human TSHβ promoter.86 The upstream region contains binding sites for the pituitary-specific transcription factor, Pit-1, suggesting a role for this or a similar factor in the regulation of the TSHβ subunit gene by TRH. In the rat TSHβ subunit gene, responsiveness to TRH has been localized to regions upstream of −204, where Pit-1 binding sites are also found.87 Furthermore, it has been shown that both protein kinase C and protein kinase A pathways can phosphorylate Pit-1 at two sites in response to phorbol esters and cyclic adenosine monophosphate (cAMP),88 thus altering the binding to Pit-1 transactivation elements on the human TSHβ gene.89
Dopamine acting via DA2 dopamine receptors inhibits TSHα and β subunit gene transcription by decreasing the intracellular levels of cAMP.81 Studies of the TSHβ subunit gene have localized two regions of the promoter necessary for cAMP stimulation, from −128 to −61 bp and from +3 to +8 bp. The upstream region coincides with the TRH-responsive region and contains Pit-1 binding sites. The downstream region resides within the regions responsive to T3 (+3 to +37) and TRH (−28 to +8). The downstream region also overlaps with an AP1 binding site (−1 to +6). The sequence from −1 to +6 appears to cooperate with Pit-1 in mediating responses to cAMP and TRH.85 Thus, multiple interactions between transcription factors and hormonal regulators appear to converge on sequences close to the transcriptional start site.
Peripheral Regulation of TSHβ Subunit Biosynthesis
Thyroid hormone is thought to act predominantly through a classical TR-mediated genomic model. T4 serves as a minimally active prohormone that is converted into a metabolically active T3 via a family of tissue deiodinases, termed D1, D2, and D3. These selenoprotein enzymes are membrane bound and can activate or inactivate substrate in a time- and tissue-specific manner.90 D2 is the major T4-activating deiodinase. It is present on the endoplasmic reticulum close to the nucleus and produces 3,5,3′-triiodothyronine (T3) through the removal of an iodine residue from the outer ring of thyroxine. D2 activity is rapidly lost in the presence of its substrate T4 by a ubiquitin proteasomal mechanism.91 Rat pituitary thyrotropes coexpress D2 RNA and protein, and both are increased in hypothyroidism. Murine thyrotropes in TtT-97 tumors or the TαT1 cell line have extremely high levels of D2, which accounts for the sustained production of T3 by thyrotropes even in the presence of supraphysiologic T4 levels. Serum TSH levels in normal mice are suppressed by administration of T4 or T3, although only T3 was effective in the mouse with targeted disruption of the D2 gene. The observed phenotype of pituitary resistance to T4 demonstrated the critical importance of D2 in controlling negative thyroid hormone regulation of TSH in thyrotropes.
T4 can also act, in some cases, via nongenomic mechanisms that do not involve classical nuclear TR mechanisms. T4 can bind to a cell-surface integrin αVβ3 receptor followed by activation of a mitogen-activated protein kinase cascade, which transduces the signal into a complex series of cellular and nuclear actions. These nongenomic hormone actions are likely to be contributors to basal rate setting of transcription of some genes, and they may control complex cellular events.92
TSHβ and α subunit gene transcription rates are markedly inhibited by treatment with triiodothyronine (T3). Studies using mouse TtT-97 thyrotropic tumors have demonstrated that suppression of TSHβ and α subunit mRNA transcription rates measured by nuclear run-on assays is evident by 30 minutes after treatment and is maximal by 4 hours.93 This effect was seen in the presence of the protein synthesis inhibitor cycloheximide, indicating that it did not require an intermediary protein. Other studies using mouse and rat pituitaries along with mouse thyrotropic tumors have demonstrated that steady-state mRNA levels of TSHβ and α subunits are dramatically decreased by T394 (Fig. 73-5). The mechanism of action of T3 involves interaction with nuclear receptors that act mainly at the transcriptional level. The transcriptional response to T3 is proportional to the nuclear receptor occupancy,95 and the time course of T3 nuclear binding and that of transcriptional inhibition are also in agreement96 (see Fig. 73-5).
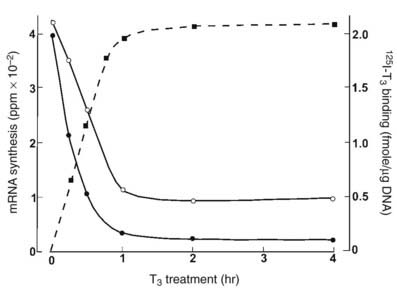
FIGURE 73-5. The effect of thyroid hormone on the transcription of the thyroid-stimulating hormone (TSH)β (black circles) and α subunit (white circles) genes. Murine thyrotropic tumor explants were incubated for up to 4 hours with 5 nmol T3 for transcription measurements or with 5 nmole 125I T3, with or without 1000-fold excess of unlabeled T3 for binding measurements. Transcription rates were measured in pools of isolated nuclei. An inverse relationship has been noted between T3 binding and TSHβ and α subunit mRNA synthesis.
(Data from Shupnik MA, Ridgway EC: Triiodothyronine rapidly decreases transcription of the thyrotropin subunit genes in thyrotropic tumor explants. Endocrinology 117:1940–1946, 1985.)
The T3 inhibitory effect on the TSHβ gene requires ligand-occupied T3 receptor (TR), specifically the TRβ1 or TRβ2 isoform, because patients with thyroid hormone resistance and inappropriate secretion of TSH have abnormalities only in the TRβ, not the TRα, gene.97 TRβ interacts with specific cis-acting DNA sequences close to the transcriptional start. T3 response elements have been reported to be located between +3 and +37 of the human TSHβ gene.98 Two T3 receptor binding sites, from +3 to +13 and from +28 to +37, may mediate T3 inhibition. T3 responses can be mediated through receptor monomers, homodimers, or heterodimers involving retinoid X receptors (RXR).99 An RXR selective ligand was shown in vitro to inhibit TSHβ expression in TtT-97 thyrotropic tumor cells100 and in cultured TαT1 thyrotropes.101 This finding has been confirmed in vivo and resulted in central hypothyroidism (low T4 and low TSH) in cancer patients treated with the retinoid bexarotene.102 The RXR-selective retinoid (LG 268) decreased circulating TSH and T4 levels in mice with marked lowering of pituitary TSHβ mRNA without decreasing TRH, suggesting a direct effect on thyrotropes.101
Other, more recent studies have disputed the requirement of the negative response element located in exon 1 of the human gene, because its deletion did not eliminate T3 suppression of TSHβ promoter activity in a reconstitution system.103 These studies showed that liganded TRβ can associate with Gata2 in vitro and in vivo via direct interaction between the zinc fingers of Gata2 and the DNA binding domain of TRβ. In addition, T3-occupied TR can physically interact with TRAP220.24 Thus, it is likely that interference with the transactivation function of the Pit-1/Gata2/TRAP220 complex on the proximal TSHβ promoter plays an important role in T3 negative regulation.
Abundant information exists as to the mechanisms involved in gene stimulation by T3. Generally, TRs bind to cis-acting DNA response elements (TRE) in the absence of ligand, interact with a family of nuclear receptor corepressor molecules that recruit histone deacetylases, and locally modify chromatin structure to result in repression of the target gene.104 In the presence of T3, the corepressor complexes rapidly dissociate and are replaced by coactivator complexes that bind to TRs and increase histone methylation and acetylation locally on the chromosomal DNA, which unwinds the chromatin into an open configuration.105 Other activating transcription factors such as TRAP220 are then recruited to the TR via protein-protein interactions, which then activate RNA polymerase II–mediated transcription.
In contrast, the molecular mechanisms involved in negative T3 regulation, such as the TSH subunit genes, have not been well characterized. Liganded TRβ has been reported to recruit histone deacetylase 3 and reduce histone H4 acetylation that modifies histones, resulting in a fully repressed chromosomal state of the TSHβ gene.103 Several recent studies have demonstrated the requirement of an intact DNA binding domain of TRβ in the negative regulation of the TSHβ gene in vitro106 and in vivo.107 In one study, a combination of Pit-1 and Gata2 activated a human TSHβ (−128/+37) reporter construct along with vectors containing TRβ1 constructs in the absence or presence of T3. These investigators found that unliganded TRβ1 did not stimulate promoter activity, whereas a mutation lacking the N-terminus and DNA binding domain of TRβ1 lost the ability of T3-treated cells to negatively regulate TSHβ promoter activity. This demonstrated the importance of various modular domains that constitute the molecular structure of TRs. Moreover, using a gene targeting approach in transgenic mice and replacing the wild-type TRβ gene with a mutant that abolished DNA binding in vitro did not alter ligand and cofactor interactions.107 Homozygous mutant mice demonstrated central thyroid hormone resistance with 20-fold higher serum TSH in the face of two- to threefold higher T3 and T4 levels, which were similar to those of TRβ homozygous null mice.
Although thyrotrope cells contain all TRs—TRα1, TRβ1, and TRβ2, as well as non-T3 binding variant α2108—it is TRβ2 that is expressed predominantly in the pituitary and in T3-responsive TRH neurons109 and is most critical for the regulation of TSH.110 Moreover, TRβ2-deficient mice had a phenotype consistent with pituitary resistance to thyroid hormone, with increased TSH and thyroid hormone levels, even in the presence of TRβ1 and TRα1, showing the lack of compensation between TR isoforms.111 However, TRβ1 and TRα1 still may play a role, in that they are able to form heterodimers with TRβ2. Heterodimers of a TR and a TR accessory protein, such as RXR, may also bind to DNA,112 constituting heterodimeric complexes that may have different affinities for specific DNA sequences and different functional activities. A particular RXR isoform, RXRγ1, is uniquely expressed in thyrotropes and appears to mediate the inhibition by 9-cis-retinoic acid through a region extending from −200 to −149 of the mouse TSHβ subunit promoter, an area upstream and distinct from that mediating negative regulation by thyroid hormone.100 Other proteins that interact with TR include the coactivators, such as the glucocorticoid receptor interacting protein-1 (GRIP-1) and the steroid receptor coactivator-1 (SRC-1),113 and corepressors, such as the silencing mediator for retinoid receptors and thyroid hormone receptors (SMRT) and the nuclear receptor corepressor (NCoR).114 These coactivators and corepressors modulate the effects of many members of the steroid-thyroid hormone receptor superfamily. Their role in the regulation of TSH subunit promoters by thyroid hormone remains to be elucidated in detail.
Studies with genetic knockout mouse models in which both TRH and TRβ genes were removed have recently showed an unexpected dominant role for TRH in vivo in regulating the hypothalamic-pituitary-thyroid axis. It appears that the presence of both TRβ and TRH is necessary for a normal thyrotroph response during hypothyroidism, suggesting that unliganded TRβ stimulates TSH subunit gene expression.115
Posttranscriptional effects of T3 have also been described. T3 decreases the half-life of TSHβ subunit mRNA and decreases the size of the poly(A) tail.116 The shortening of the poly(A) tail is thought to cause mRNA instability. Leedman et al. showed that T3 increased the binding of an RNA-binding protein present in rat pituitary to the 3′-untranslated region of the rat TSHβ mRNA117 and also induced a shortening of the poly(A) tail of the mouse TSHβ mRNA from 160 to 30 nucleotides.118
Steroid hormones, specifically glucocorticoids, inhibit TSH production, but TSH subunit mRNA levels do not change significantly.119 Their major effect may be seen at the secretory level. Estrogens mildly reduce both α and TSHβ subunit mRNA in hypothyroid rats compared with euthyroid controls.120 In this study, estrogen also abolished the early rise in subunit mRNA levels seen following T3 replacement. Testosterone has been shown to increase TSHβ subunit mRNA in castrate rat pituitary and mouse thyrotropic tumor.121
Leptin and neuropeptide Y have opposite effects on TSH biosynthesis. Leptin is the product of the ob gene, which is found mainly in adipose tissue and regulates body weight and energy expenditure.122 Neuropeptide Y (NPY) is a neuropeptide that is synthesized in the arcuate nucleus of the hypothalamus and plays many roles in neuroendocrine function.123 In dispersed rat pituitary cells, leptin stimulated and NPY inhibited TSHβ mRNA levels in a dose-related manner.124 In contrast, both agents increased α subunit steady state mRNA levels.
Hypothalamic Regulation of α Subunit Biosynthesis
TRH stimulates α subunit biosynthesis through a novel mechanism. A CRE-binding protein that binds to the region from −151 to −135 of the human α subunit promoter appears to be important for TRH regulation, as well as a Pit-1–like protein that binds to a more distal region from −223 to −190.125 The CRE of the human glycoprotein hormone α subunit gene promoter consists of an 18 bp repeat and extends from −146 to −111.126 The mechanisms involved in TRH stimulation of the α subunit gene appear to involve two transcription factors, P-Lim and CREB binding protein (CBP). When stimulated with TRH, both of these factors transcriptionally cooperate to activate α subunit promoter activity caused by direct protein-protein interactions.127 Both of these factors synergistically activated the α subunit gene promoter during TRH stimulation and interact in a TRH-dependent manner. P-Lim binds to the α subunit promoter directly, but CBP does not possess a DNA binding domain, so it must be recruited to the promoter via interaction with another factor. The P-Lim/CBP binding is formed in a TRH signaling-specific manner, in contrast to forskolin, which mimics protein kinase A signaling and dissociates both the binding and the transcriptional synergy. α subunit gene expression in thyrotropes is inhibited by dopamine in coordination with expression of the TSHβ subunit gene. Its action is mediated by decreases in intracellular cAMP levels.
Peripheral Regulation of α Subunit Biosynthesis
Thyroid hormone inhibition of α subunit gene transcription is observed in thyotropes in coordination with that of the TSH β subunit. The T3 response element of the human α subunit gene promoter has been reported to be located from −22 to −7.128 Similar to the TSHβ subunit gene, the T3 response elements of human and of mouse129 and rat130 genes are located close to the transcriptional start. T3 inhibition may be mediated by different isoforms of the T3 receptor131 in combination with the corepressors SMRT and NCoR.132 Studies have suggested that mutations of the T3 response element of the human α subunit promoter that eliminate TR binding do not abrogate the inhibitory effect of T3, suggesting that protein-protein interactions may be more important than protein-DNA binding.133
Steroid hormone regulation of α subunit gene transcription is probably of limited importance. Androgen inhibition and androgen receptor (AR) binding have been localized to a region from −120 to −100. Negative regulation by estrogen was described in the gonadotropes of transgenic mice expressing a reporter gene under the control of both human and bovine promoters, but no binding of these regions to the estrogen receptor (ER) was detected, suggesting an indirect effect.134 However, other studies using rat somatomammotropes have found positive regulation by estrogen localized to the proximal 98 bp of 5′-flanking DNA of the human α subunit gene and binding of the ER to the T3 response element from −22 to −7.135 Transcriptional inhibition by glucocorticoids may be mediated by binding of the glucocorticoid receptor to sequences between −122 and −93 of the human α subunit gene.136 However, no direct binding was detected in other studies, suggesting that the GR inhibits transcription by interfering with other transactivating proteins.137
Regulation of TSH Glycosylation
Glycosylation is a regulated process that is primarily modulated by TRH and thyroid hormone.138 Primary hypothyroidism139 and TRH administration140 have been found to increase oligosaccharide addition, which results in an increased bioactivity of TSH.141 The same was noted in patients with resistance to thyroid hormone. TSH glycosylation patterns were found to differ in several pathologic states such as central hypothyroidism, TSH-producing pituitary adenomas, and euthyroid sick syndrome.142 Also observed were changes in the sulfation and sialylation of the oligosaccharide residues, which modulate bioactivity.139,143,144 Recently, thyroid hormone was shown to increase TSH bioactivity, and this was correlated with decreased sialylation.145
REGULATION OF TSH SECRETION
As with biosynthesis, TSH secretion is a result of complex interactions between central and peripheral hormones (Fig. 73-6).
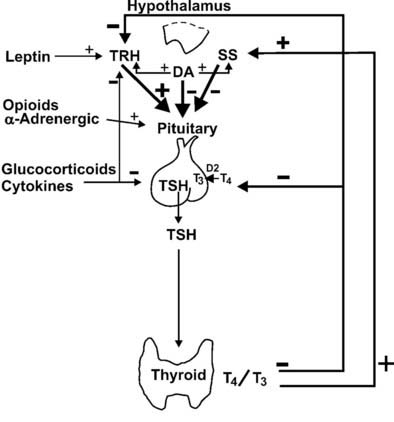
FIGURE 73-6. Hypothalamic and peripheral control of thyroid-stimulating hormone (TSH) secretion. Positive and negative stimuli are indicated at various levels within the hypothalamic-pituitary-thyroid axis. T4, thyroxine; T3, triiodothyronine; TRH, thyrotropin-releasing hormone; SS, somatostatin; DA, dopamine; D2, deiodinase type II.
Hypothalamic Regulation of TSH Secretion
TRH directly affects TSH secretion in vivo and in vitro at concentrations that exist in the pituitary portal blood.146 Immunoneutralization of TRH in animals leads to a decline in thyroid function,147 and TRH knockout mice have a reduced postnatal TSH surge, followed by impaired baseline thyroid function with a poor TSH response to hypothyroidism. Lesions of the paraventricular nucleus (PVN) decrease circulating TRH and TSH levels in normal or hypothyroid animals and cause hypothyroidism148 and electrical stimulation of this area causes TSH release. Although baseline levels of TSH are reduced in animals with lesions of the PVN, TSH levels still show appropriate responses to changes in circulating thyroid hormone levels. Thus, TRH likely determines the set point of feedback control by thyroid hormones.
Acute intravenous administration of TRH to human subjects causes a dose-related release of TSH from the pituitary. This occurs within 5 minutes and is maximal at 20 to 30 minutes. Serum TSH levels return to basal levels by 2 hours. More prolonged (2 to 4 hour) infusions of TRH lead to biphasic increases in serum TSH levels in humans and animals.149 The early phase may reflect release of stored TSH, and the later phase may reflect release of newly synthesized TSH. Interpretation of TSH responses to even more prolonged TRH infusions is complicated by the increase in serum T3 levels, with feedback to suppress further TSH release.77 Continuous TRH administration in vitro also causes desensitization of TSH responses, which may further explain decreased TSH levels with long-term TRH exposure.150
Somatostatin (SS) in humans and animals inhibits basal and TRH-stimulated TSH secretion in vivo and in vitro at concentrations that exist in the pituitary portal blood.151 In the hypothalamus, the highest concentrations of SS occur in the anterior paraventricular region.152 From this region, axonal processes of SS-containing neurons project to the median eminence. Animals that have undergone sectioning of these fibers have depletion of SS content of the median eminence and increased serum TSH levels.153 Similarly, immunoneutralization of SS in animals increases basal TSH levels and TSH responses to TRH.154 In humans, SS infusions suppress TSH pulse amplitude, slightly decrease TSH pulse frequency, and abolish the nocturnal TSH surge.155 Thus, TSH secretion probably is regulated through a simultaneous dual-control system of TRH stimulation and SS inhibition from the hypothalamus.
SS binds to specific, high-affinity receptors in the anterior pituitary gland. Five subtypes of the SS receptor (SST1 through SST5) have been identified,156 and SST1 and SST5 have been localized to thyrotropes.157 Binding of SS to its receptor inhibits adenylate cyclase via the inhibitory subunit of the guanine nucleotide regulatory protein, which lowers protein kinase A activity156 and decreases TSH secretion. SS may also exert some effects by cAMP-independent actions on intracellular calcium levels. Hypothyroidism reduces the efficacy of SS in decreasing TSH secretion in vitro, which is reversed by thyroid hormone administration.158 Additional studies in mouse thyrotropic tumors indicate that both SST1 and SST5 are markedly downregulated in hypothyroidism and are induced by thyroid hormone.157 Although short-term infusions of SS lead to pronounced suppression of TSH secretion in humans, long-term treatment with SS or its analogues does not cause hypothyroidism.159 This probably reflects compensatory mechanisms in the thyroid hormone feedback loop. GH deficiency is associated with increased TSH responses to TRH, and GH administration decreases basal and TRH-stimulated TSH secretion,160 possibly owing to GH stimulation of hypothalamic SS release.
Dopamine also inhibits basal and TRH-stimulated TSH secretion in vivo and in vitro at concentrations that exist in the pituitary portal blood.161,162 Exogenous dopamine antagonists, including those that do not penetrate the blood-brain barrier, increase TSH levels.163 In humans, dopamine infusions rapidly suppress TSH pulse amplitude, do not affect TSH pulse frequency, and abolish the nocturnal TSH surge155; administration of a dopamine antagonist has the opposite effect.164 Dopamine also has direct effects on hypothalamic hormone secretion that may indirectly affect TSH secretion. For example, dopamine and dopamine-agonist drugs stimulate both TRH and SS release from rat hypothalami.165
In the hypothalamus, dopamine is secreted by neurons in the arcuate nucleus.166 From the arcuate nucleus, neuronal processes project to the median eminence. Dopamine acts by binding to type 2 dopamine receptors (DA2) on thyrotrope cells.167 This leads to inhibition of adenylate cyclase, which decreases the synthesis and secretion of TSH. In addition, TSH may downregulate its own release through the induction of DA2 receptors on thyrotrope cells.168 The inhibitory effects of dopamine on TSH secretion vary according to sex steroids, body mass, and thyroid status. Dopamine antagonist drugs cause greater increases in serum TSH levels in women than in men. Recent studies show that obesity is associated with enhanced TSH secretion, which may be mediated via blunted central dopaminergic tone.169 Dopamine inhibition of TSH release is greater in patients with mild hypothyroidism than in normal subjects, although subjects with severe hypothyroidism may be less responsive.170 Although short-term infusions of dopamine lead to pronounced suppression of TSH secretion, long-term treatment with dopamine agonists does not cause hypothyroidism. This probably reflects compensatory mechanisms in the thyroid hormone feedback loop.
Adrenergic effects have also been reported in vivo and in vitro. α-Adrenergic activation stimulates TSH release directly from the rat pituitary gland at physiologic concentrations of catecholamines.171 α-Adrenergic agonists stimulate TSH release in rats, and blockade of norepinephrine synthesis or treatment with adrenergic receptor blockers decreases TSH levels.166,172 It is unclear whether these effects are mediated via changes in TRH and/or SS levels. In humans, data regarding adrenergic effects on TSH secretion are limited. α-Adrenergic blockade diminishes serum TSH responses to TRH.173 However, administration of epinephrine does not alter TRH-stimulated TSH secretion.174 These data suggest that endogenous adrenergic pathways do not have a major role in TSH secretion. Noradrenergic stimulation of TSH secretion is mediated by high-affinity α1-adrenoreceptors linked to adenylate cyclase.173 Therefore, dopamine and epinephrine appear to exert opposing actions on thyrotropes through opposite effects on cAMP generation.
Opioid administration to rats suppresses basal or stimulated TSH levels, and the opioid receptor antagonist naloxone reverses these effects.175 Acute opiate administration in humans may slightly stimulate TSH levels, and acute naloxone administration has little effect.176 In contrast to these acute studies, when naloxone is given over 24 hours, 24 hour TSH secretion decreases, primarily owing to a decrease in nocturnal TSH pulse amplitude.177 TSH responses to TRH are also decreased. Serum T3 levels are decreased as well, suggesting that the magnitude of TSH suppression is sufficient to affect thyroid gland function. These findings suggest that endogenous opioids may play a role in tonic stimulation of TSH secretion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree