Technetium-99m (99mTc) in the form of pertechnetate is trapped by the thyroid gland and other sites that concentrate iodide (salivary glands, gastric mucosa), but it is not organified in the thyroid and is therefore not a true tracer of iodine metabolism.1 The radiation exposure to the thyroid from 99mTc is even lower than that from 123I. 99mTc is readily available in nuclear medicine laboratories and is relatively inexpensive. 99mTc-pertechnetate is administered intravenously in amounts ranging from 2 to 10 mCi (74 to 370 MBq), and imaging of the thyroid is usually begun 15 to 30 minutes after injection.2
123I and 99mTc have largely replaced 131I for thyroid scintigraphy. Radiation exposure to the thyroid from 131I per microcurie administered is 100-fold higher than that from 123I, and 131I-labeled images of the gland are generally inferior in quality because of the high γ energy of 131I.
The principal diagnostic use of 131I is in whole-body scanning to search for functioning metastases that are potentially treatable with 131I in patients who have had thyroid cancer surgery. The 8-day half-life of 131I permits scanning over a period of several days, which facilitates proper identification of anatomic sites that accumulate inorganic iodine but do not produce or harbor thyroxine and also iodine excretory routes. In distinction to these transient foci of radioactivity, functioning metastases retain activity and slowly release their organic product. Thus the signal-to-noise ratio is enhanced greatly. The long half-life also allows for dosimetry in preparation for 131I therapy. A high beta-particle radiation exposure to the thyroid gland (in contrast to all other organs and tissues) from 131I, the long half-life, and selective concentration of the isotope by the thyroid together permit destruction of benign or malignant thyroid tissue.
SCINTISCANNING INSTRUMENTATION
In most nuclear medicine laboratories, the scintillation camera has largely replaced the rectilinear scanner for thyroid imaging. The camera is fitted with a pinhole collimator, which provides a variable-size image of the gland and yields higher resolution than that obtained with a parallel-hole collimator or rectilinear scanner3 (Fig. 78-1). The pinhole technique permits oblique views of the gland, which is an advantage in detecting posterior nodules, but accurate estimation of gland size is not possible. In dealing with thyroid nodules, it is important to correlate the image with the palpable lesion by placing radioactive spot markers on the skin overlying or adjacent to the nodule. Particular care must be taken in placing radioactive markers because parallax errors are possible with the pinhole method, and in the case of small nodules (<1 cm), skin markers may even be misleading. Furthermore, it is extremely difficult and undependable for a physician to palpate for thyroid pathology when a patient is “under” a gamma camera, which is necessary to correlate anatomy and image in the scanning position. The parallel-hole collimator technique is better at assessing size because it avoids parallax error, but standards of image contrast and intensity are arbitrary, and the assessment of thyroid dimensions is subjective and inconsistent. The resolution of nodules with this collimator is very poor.

FIGURE 78-1. Scintiscan of the thyroid in a 72-year-old patient with Graves’ hyperthyroidism. This image was obtained with a pinhole collimator 6 hours after oral administration of 200 µCi 123I. Thyroid uptake was 24% at 6 hours. Note the diffuse pattern of 123I distribution throughout the gland. The faint activity extending superiorly from the right lobe is a pyramidal lobe.
Rectilinear scanners equipped with a focused collimator and a coaxial, narrow beam of light that is projected onto a palpated anatomic feature provide life-size images and allow accurate correlation of an image and the palpation. If desired, the pencil of light can be used to place markers over nodules and landmarks, or the scan film can be marked directly to localize a lesion or physical feature. The resolution of a rectilinear scanner image is not as high as that produced by a camera with a pinhole collimator.3 These scanners are currently not commercially available.
Whole-body scintiscans, obtained by using either a scintillation camera or a rectilinear scanner and a special scanning table, are used in surveys for thyroid cancer metastases that involve the administration of 131I or other radiolabeled agents. A scanning system that results in a composite image of the entire body provides more reliable anatomic orientation and is easier to interpret than multiple scans of isolated areas. However, spot-scans of a specific area such as the neck may offer superior anatomic detail.
Single-photon emission computed tomography (SPECT), which is widely used in nuclear medicine and requires more isotope than standard scintiscanning, provides three-dimensional images or tomographic slices through the organ of interest. When used with either 99mTc or 123I, SPECT of the thyroid has an advantage over other methods of scintigraphy (including the pinhole technique) in defining the function of small nodules that may be obscured by overlying normal thyroid tissue.4 SPECT is also useful for estimating the volume of functioning thyroid and for identifying thyroid tissue in ectopic sites such as the substernal area. 131I SPECT whole-body scanning in thyroid cancer patients greatly enhances anatomic localization of metastases. Fusion of SPECT images with CT or MRI images provides the most impressive and precise anatomic localization.
Positron emission tomography (PET) requires special tomographic equipment that is capable of imaging the high-energy γ-rays produced by positron-emitting radionuclides (e.g., 18F and 124I).
As a caveat, with scanning in general and particularly with whole-body scanning, one must keep in mind that the scan image of a metastasis that accumulates abundant isotope might appear to be considerably larger than the mass. Especially in the neck, ultrasonography is the best way to estimate the volume of a metastasis.
PATIENT PREPARATION
For thyroid scanning, the patient need not be fasting on the morning of the study, but a heavy meal can retard absorption of iodide and reduce uptake values for the initial hours. Patients are asked about medications and dietary items that interfere with thyroid radioiodine uptake. When the uptake of radioiodine is low for any reason, the quality of the image is impaired. The most common interfering substances are radiographic contrast dyes, drugs that contain iodine (e.g., amiodarone), and iodine-containing food supplements such as kelp. Thyroid hormone in any form reduces thyroid radioiodine uptake except when autonomously functioning thyroid tissue is present or there is an abnormal thyroid stimulator. Because the administration of radioactive materials is contraindicated during pregnancy and breastfeeding, these aspects of the history must be included in the preliminary interview when appropriate.
DIAGNOSTIC APPLICATIONS OF THYROID SCINTIGRAPHY
The Thyroid Nodule
The terms cold and hot are commonly used to describe the functional activity of thyroid nodules as revealed by scintigraphy. These descriptors refer to the apparent amount of radionuclide in the lesion relative to that in surrounding normal thyroid tissue. Until recently, this distinction was diagnostically important to identify thyroid cancer. Nearly all malignant tumors in the thyroid concentrate less radioiodine or 99mTc than the normal gland and therefore appear cold (hypofunctional). However, since many benign tumors and nontumorous nodules are also cold, that characteristic is now of limited clinical use because of the advent of fine-needle biopsy (FNB). Now “hot versus cold” is important in the choice not to do an FNB in patients with a nodule when TSH is low and the nodule is hot; hot nodules are very rarely malignant, and the biopsy may be misleading by incorrectly suggesting malignancy (Fig. 78-2).
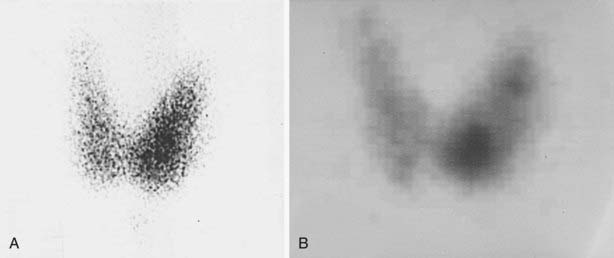
FIGURE 78-2. Thyroid scintiscans in a mildly hyperthyroid patient (suppressed serum thyroid-stimulating hormone, borderline-high free thyroxine and triiodothyronine levels) with a palpable 1.5-cm solitary nodule in the lower portion of the left thyroid lobe. A, Pinhole image showing that most of the 123I uptake is in the lower pole of the left lobe, which corresponds to the palpable nodule. B, Single-photon emission computed tomographic (SPECT) image showing a more clearly delineated hyperfunctioning nodule in the lower pole and two smaller (nonpalpable) foci of uptake in the upper portion of the left lobe. Both pinhole and SPECT images were obtained 6 hours after administration of 123I (200 µCi). The diagnosis was multiple autonomously functioning nodules.
The term warm nodule is ambiguous and not helpful in assessing the risk of cancer. The term should not be used. A nodule that is not clearly delineated on a scintiscan may in fact be a cold nodule that is too small or too close to normal activity to be distinguishable from surrounding normal thyroid tissue. In general, a cold nodule must be almost 1 cm or larger in diameter to be detected by pinhole imaging.
Because the great majority of nodules are cold on radioisotope scintiscanning, and such cold nodules may be either benign or malignant, it is not cost effective to obtain a scintiscan as the initial diagnostic test in a euthyroid (normal TSH) patient with a nodule. A fine-needle aspiration (FNA) biopsy is usually performed first. However, when the FNA result indicates sheets of follicular cells that do not look malignant but could be a tumor, scintigraphy may be helpful to identify a hot nodule, thus avoiding surgery.
There are two kinds of hot nodules. The majority of them are reactive to elevated TSH in an otherwise failing thyroid gland and thus are compensatory. These are called hyperplastic nodules. The hot nodules associated with low TSH are autonomous nodules. They function autonomously because the TSH receptor of the thyroid cell has mutated and does not require TSH to stimulate cell activities such as the production of thyroxine or cell replication and nodule growth. The clone of the mutated cells is a benign tumor, which is the nodule, and may grow large enough over time to lead to hyperthyroidism (“toxic” nodule, TAN). When TAN-produced thyroid hormone levels increase, TSH falls, leading to suppression of the normal paranodular tissue in both thyroid lobes.5 The chance of malignancy in a hot nodule is less than 1%.1 Therefore, when TSH is undetectable in a patient with a thyroid nodule, a scintiscan may be the next appropriate test. In some cases, a hyperfunctioning nodule undergoes degeneration or hemorrhage, and therefore part of it, or uncommonly all of it, becomes hypofunctioning or cold. Some of the reported instances of cold areas in a hot nodule are in fact cases of small, coexisting carcinomas in close proximity to a larger, benign hot nodule. Although documented cases have been reported in which the entire hot nodule is malignant, these cases are quite rare.
Occasionally, follicular neoplasms (including follicular adenomas and even some carcinomas) may appear hot on a 99mTc-pertechnetate image but cold on a radioiodine image, presumably because such tumors are able to trap but do not organify iodine. This type of discordance between 99mTc and radioiodine images occurs infrequently and must be recognized when 99mTc is used for thyroid scintiscanning.5–7
In the past, one spoke of a solitary thyroid nodule. We assumed incorrectly that if the rest of the thyroid gland was normal to palpation, it was free of nodules. Examination by ultrasound and correlation with pathology has disclosed that nonpalpable nodules occur commonly when a dominant nodule has been palpated.
Multinodular Goiter
Scintiscanning by itself does not reveal the etiology of a multinodular goiter. Scintiscanning has a role in the diagnostic assessment of multinodular goiter in some patients. When the nodules are discrete and larger than 1 cm in diameter, the scintiscan reveals the functional activity of a particular nodule relative to that of paranodular tissue (Fig. 78-3). When a nodule is clinically dominant—that is, a nodule that on palpation or by ultrasonography is different from the other nodules or is growing faster—the finding on scintiscan that this nodule contains all or most of the functional activity helps to guide management. Such a functioning nodule is unlikely to be malignant. When a multinodular goiter is large and causes symptoms and signs of compression of the trachea or esophagus, scintiscanning may complement other imaging modalities such as MRI or sonography. Either of the latter two methods depicts the extent of the goitrous mass, but only scintiscanning can reveal functioning tissue, information that is often helpful in making therapeutic decisions such as surgery or 131I therapy.

FIGURE 78-3. Anterior pinhole scintiscan of a multinodular goiter in a euthyroid patient. Physical examination revealed many firm nodules with the largest nodule (2 × 3 cm) in the left lobe. The image, obtained 24 hours after administration of 250 µCi 123I (thyroid uptake, 23%), shows the left lobe nodule to be cold (arrow). A functioning nodule is seen in the isthmus. Surgical excision of the gland showed all nodules to be mixed solid/cystic and benign.
In a hyperthyroid patient with a nodular goiter, there may be several different patterns on scintigraphy. The image may show many functioning, widely dispersed nodules, generally smaller than 0.5 cm, that have a salt-and-pepper appearance; a coarsely patchy distribution may be evident, or a uniform pattern of uptake not unlike that of Graves’ disease can be seen. In contrast, there may be a cold zone correlating with a nodule that should be evaluated by other means, such as sonography and aspiration biopsy.
In a hypothyroid patient with nodular goiter, the uptake is usually low (unless there is iodine deficiency or dyshormonogenesis), and thus the scintigraphic image shows a “patchy” distribution of radioisotope because of low “counts” that result in poor scan statistics. However, scintigraphy may be of clinical value to identify a reactive, hyperplastic, functional area that is rarely malignant.
Diffuse Goiter Including Graves’ Disease
Assessing the thyroid uptake of radioiodine is diagnostically important to differentiate the low accumulation of the tracer in silent thyroiditis and its high accretion in hyperthyroid Graves’ disease and for precise dosimetry of 131I therapy. However, thyroid scintiscanning usually is not clinically useful in diffuse goiters. If assessing size is desired, an ultrasonogram offers superior results. Yet, some clinicians order scintiscans for patients with Graves’ disease.
The pattern of isotope accumulation in Graves’ disease usually is uniform, but irregular distribution may occur, especially in a geographic region where goiter is endemic. The heterogeneity should not be misconstrued as reflecting toxic nodular goiter when the clinical setting and serologic tests are more consistent with Graves’ disease. At times, a patient with Graves’ disease may have a palpable thyroid nodule or an unusually firm area, or a nonisotopic neck-imaging procedure might have disclosed an incidentaloma (discussed later) that leads to scintiscanning to assess whether it is cold, in which case sonography and aspiration biopsy might be appropriate. Similarly, a “routine” scintiscan might have revealed a cold area that should be investigated.
Substernal Goiter
A substernal goiter is suspected when chest radiographs or CT reveal an anterior mediastinal mass. A positive radioiodine scintigram definitively identifies such a mass as thyroid tissue. 123I or 131I is preferred over 99mTc in such cases because of interference by circulating 99mTc in the mediastinal blood vessels. SPECT (using 123I) is of particular value in visualizing substernal thyroid tissue and SPECT/CT or MR can precisely localize it to an anatomical structure.
Scintigraphy in Patients With Thyroid Carcinoma
In general, thyroid carcinoma takes up and retains radioiodine much less efficiently than normal thyroid tissue does. Therefore, most thyroid cancers are cold nodules. However, after the thyroid gland has been removed surgically and under the stimulation of elevated TSH levels and iodine deprivation, the uptake in differentiated thyroid carcinoma is often sufficiently high to permit detection by scintigraphy and therapy with 131I. Thus diagnostic imaging with radioiodine is indicated for patients who have recently undergone thyroid surgery for differentiated thyroid carcinoma. The rationale for imaging in such patients is to identify and quantify uptake in the thyroid remnant and to detect any functioning metastases in the neck or in distant sites. This information helps to determine the amount of 131I that should be administered to ablate the normal remnant and treat functioning metastases.
To stimulate uptake of radioiodine by malignant thyroid tissue, it is necessary to raise serum TSH levels to 30 mU/L or higher.7 In routine practice, levothyroxine therapy is discontinued for 5 to 6 weeks before administration of the diagnostic dose of radioiodine for imaging. To shorten the period of hypothyroidism, liothyronine (triiodothyronine [T3]) is often given (25 to 50 µg/day in divided doses) for 3 weeks after discontinuation of levothyroxine therapy. T3 therapy is discontinued 2 weeks before radioiodine administration. Alternatively, it is possible to prepare patients by giving their usual thyroxine dose every other day for 6 weeks, which induces mild hypothyroidism and raises the level of TSH to about 50 mIU/L.
Recently, recombinant human TSH (rhTSH, Thyrogen, Genzyme Corp., Cambridge, MA) has been developed and in clinical trials has been shown to stimulate uptake of 131I by thyroid remnants and metastases and to raise serum thyroglobulin (Tg) levels in patients who remain euthyroid while taking thyroid hormone therapy.8,9 The Food and Drug Administration has approved the use of rhTSH for radioiodine imaging and serum Tg testing in such patients and for the destruction (ablation) of thyroid tissue that remains after a total thyroidectomy has been performed because of thyroid cancer.
Patients who are scheduled to undergo diagnostic whole-body scintigraphy are advised to follow a low-iodine diet for at least 7 to 10 days before administration of the radioiodine. A simple low-iodine diet has been described.10 It is even more important to avoid iodine-containing medications and radiographic contrast agents.
Diagnostic administration of 131I may reduce the uptake of subsequent therapeutic 131I by normal thyroid remnants or functioning metastases. This phenomenon, which has been termed stunning, seems to involve a sublethal, presumably temporary suppression of iodine uptake (reviewed elsewhere11,12). To avoid stunning, many authors recommend limiting the quantity of 131I given for diagnostic imaging to 2 mCi (74 MBq)11,13 or even less.14 An alternative is to use 123I for whole-body imaging,15 but the present cost of this radionuclide in millicurie amounts is prohibitive for many centers. While 123I offers superior imaging of deposits of thyroid tumor in the neck when compared to 131I, its efficiency for deposits deep in the rest of the body remains to be established convincingly.
Physicians who interpret whole-body radioiodine scintigrams must be familiar with the distribution of inorganic iodine in the blood pool and extracellular fluid and its dynamics over time, the normal, nonthyroid sites that accumulate the radioactive iodine tracer, and the behavior of isotope-labeled thyroxine that has been produced in thyroid gland or metastases. The salivary glands, gastric mucosa, kidneys, and lactating breasts concentrate iodide but do not convert it to thyroxine. Nasal secretions, saliva, sweat, urine, stool, and milk may contain high concentrations of inorganic radioiodine and can cause artifacts, depending on the time after isotope administration. Skin and hair are easily contaminated with saliva, urine, or vomitus. Radioiodine-labeled thyroxine is observed later than inorganic iodide and has a different pattern of distribution, including the liver as part of the enterohepatic circulation of thyroxine. Nonthyroid tumors, inflammatory lesions, and cysts may occasionally contain radioiodine as part of their vasculature and result in a false-positive scintigram.11,16
In interpreting 131I planar whole body scans, there may be atypical or cryptic findings. 131I SPECT/CT is useful to characterize challenging foci more accurately, differentiate thyroid cancer from physiologic activity or nonthyroid pathology, and reduce false positives. By identifying nonthyroid cancer activity, SPECT/CT can reduce inappropriate treatment with 131I.
131I scanning is not 100% sensitive for metastatic thyroid carcinoma. In some series, the rate of false-negative radioiodine scans approaches 35%.17 When diagnostic 131I scans are negative and metastases are suspected on the basis of elevated serum Tg levels, some advocate empirical treatment with 131I. Scans that are done 1 week after 131I therapy are frequently positive in these cases (reviewed by Clark and Hoelting18) (Fig. 78-4). Indeed, a routine pre-ablation scan after thyroidectomy for thyroid cancer may not be cost effective. Therefore, many centers employ a protocol of administering a standard therapeutic dose of 131I without prescanning and perform the whole body scan a week later. This protocol is limited by an inability to do dosimetry for the treatment, which some authorities deem essential, and fails to assess for undetected metastases in the head or spine, which may swell after 131I and cause neurologic complications.
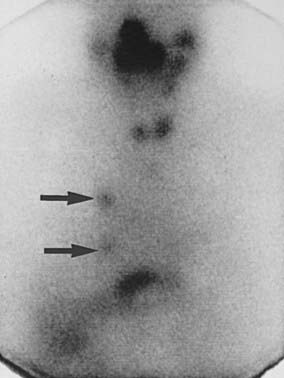
FIGURE 78-4. Anterior scintiscan of head, neck, chest, and upper part of the abdomen in a male patient who 72 hours previously had received 212 mCi 131I as therapy for follicular thyroid carcinoma metastatic to the lung. The image shows intense activity in the nose, mouth, and salivary glands; small right and left thyroid lobe remnants; two discrete foci of uptake in the right side of the chest (arrows) corresponding to small lung nodules seen on computed tomography; and physiologic radioiodine in the stomach and bowel. The liver is faintly visualized, a common finding in post-therapy scintiscans with no pathologic significance.
It is useful in 131I scan-negative, Tg-positive patients to search for metastases by performing sonography of the neck and, if negative, performing MRI of the neck and chest. Especially if 131I therapy is anticipated, contrast CT studies are not employed, but noncontrast CT may suffice. The aim is to find metastases that either are surgically accessible or can be treated by external radiotherapy, if appropriate. When the above imaging techniques do not reveal a source of the elevated Tg, scintiscanning with other radiolabeled agents or fluoro-deoxyglucose (FDG)-PET scanning may succeed in localizing 131I-negative metastases19 (see Table 78-2).
Thallium (201Tl) has been useful in localizing metastases in selected patients (reviewed by Cavalieri12 and Sisson19). However, 201Tl is concentrated by a variety of benign and malignant lesions other than thyroid carcinoma.
99mTc-sestamibi (MIBI) is a cationic, lipophilic agent that concentrates in normal and neoplastic thyroid tissue and in a variety of other cancers. Experience indicates that like 201Tl, 99mTc-MIBI can be useful in 131I-negative patients in whom one has reason to suspect persistent or recurrent tumor.19,20 99mTc-MIBI is the agent of choice for imaging Hürthle cell carcinoma, which typically takes up radioiodine poorly.21
Other agents that have been shown to concentrate in some metastatic differentiated thyroid tumors are 99mTc-tetrofosmin, which like MIBI is a myocardial perfusion imaging agent, and 99mTc-labeled dimercaptosuccinic acid in the pentavalent form (DMSA [V]) (reviewed by Sisson19). Clinical experience with these agents is still limited. Indium-111-labeled octreotide is used to localize metastatic medullary thyroid carcinoma.22
18Fluoro-2-Deoxyglucose Positron Emission Scanning
18F-fluoro-2-deoxyglucose (18FDG), a radiolabeled analogue of glucose, is actively concentrated in a variety of malignant tumors, including thyroid carcinoma.23 18FDG uptake tends to be higher in thyroid tumors that are not well differentiated, in contrast to 131I, which is accumulated by differentiated cancers. For this reason, 131I-negative tumors are more often positive with 18FDG, and 18FDG-negative tumors tend to be positive with 131I.23 18FDG-PET scans show low background in the chest and liver, which gives this agent a relative advantage over 201Tl and 99mTc-MIBI. Enhanced clinical value of PET images is obtained when they are fused with CT or MRI images. The last section of this chapter, Positron Emission Tomography and Bimodality CT or MRI Fusion Scanning, offers an in-depth discussion of the subject.
Nonisotopic Thyroid Imaging Tests
The nonisotopic thyroid-imaging tests consist of sonography, CT, and MRI. Sonography reveals how the tissue transmits and/or reflects sound waves, CT is a computerized analysis of the relative density of tissues to x-rays, and MRI depicts the response of hydrogen atoms to a magnetic field. Both CT and MRI provide sectional images that can be electronically assembled in perpendicular planes. None of these techniques are a substitute for histopathology, and none differentiate benign and malignant lesions.
SONOGRAPHY (ECHOGRAPHY)
Sonography is efficiently used to (1) elucidate cryptic findings on physical examination, (2) identify nonpalpable nodules or the solid component of a complex nodule for guiding FNA, (3) determine the comparative size of nodules in patients who are under observation, (4) detect small nodules in patients who were exposed to therapeutic irradiation of the head or neck, (5) identify sonographic characteristics of a nodule that are associated with a greater than average risk of cancer, (6) improve the accuracy of needle placement in percutaneous biopsy, and (7) evaluate for recurrence of thyroid cancer after surgery, particularly in cervical lymph nodes.
Technical Aspects
Sonography uses high-frequency sound waves (ultrasound) in the megahertz range to produce a photographic image of the internal structure of the thyroid gland and its region.24,25 No ionizing radiation is involved, nor is iodinated contrast material given. Sonography is safe; tissue damage has not been reported, and it is less costly than other imaging procedures. Preparation of the patient for the procedure is unnecessary, and it is performed without discontinuing TSH suppressive therapy. To image the thyroid gland and surrounding regions, the patient’s neck is examined in the sagittal, transverse, and oblique planes with a probe called a transducer that both generates the sound energy and receives the reflected signal. The sound enters the body and is transmitted or reflected by interfaces within the tissues. Air does not transmit ultrasound, and calcified areas block its passage. The images are produced quickly and are assembled electronically in “real time.” Each frame of the sonogram shows a static image, and sequential pictures depict motion. Swallowing is used to elevate the thyroid to examine the lower pole of an enlarged lobe, and this maneuver may facilitate identification of the esophagus. With the use of a signal having a frequency of 7.5 to 12 MHz, thyroid nodules and lymphadenopathy as small as 2 to 3 mm are identified in shades of gray. Dynamic information such as blood flow is added by using physics principles called the Doppler effect.26 The signals are translated into colors to differentiate static fluid-filled cystic spaces and blood flowing through the vasculature. Thus the direction and velocity of flow and the degree of vascularity are revealed. Color is assigned to the signal by assuming that venous flow is parallel to, but in the opposite direction to, arterial flow. Arterial signals are made red, and the accompanying venous signals are made blue. The shade of a color is proportional to the direction of flow as it relates to the transducer and flow velocity.
Routine protocols for ultrasound scanning by a technologist are not satisfactory but unfortunately are used too often, degrading the value of the test. Rather, the ultrasound operator must be experienced and aware of the clinical question that has been posed to provide an appropriate answer. Close supervision by a sonographer-physician or endocrinologist who is expert in physical examination and ultrasonography is needed.
It is important to comprehend that the optimal clinical value of sonography depends on the quality of the ultrasound examination, including the maturity of the examiner and the characteristics of the equipment. Grossly misleading results are common with quick, incomplete studies and unsophisticated machines or readouts. Therefore, routine sonography in a medical or radiology office will require proper preparation of the professional and technical staff. Without study, training, and experience, there are likely to be unacceptable results and adverse outcomes.
Sonography of the Normal Thyroid Gland and Environs
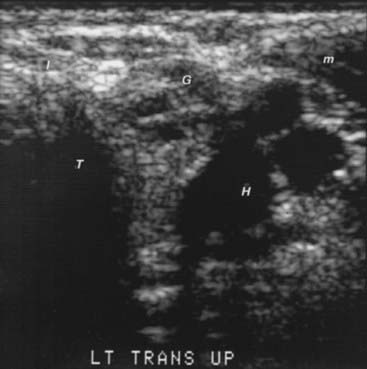
With standard gray-scale technique, the normal thyroid gland has a homogeneous appearance like ground glass (Fig. 78-5). The surrounding muscles are of equal or lower echogenicity. Tissue planes are identified. The air-filled trachea, which does not transmit the ultrasound signal, is poorly imaged, and dense echoes represent its calcified tracheal ring anteriorly. The carotid artery and other blood vessels are echo-free unless calcified. Lateral and anterior to the carotid arteries is the jugular vein, which is frequently collapsed and can be identified when it is distended during a Valsalva maneuver. Small blood vessels on the surface of the thyroid and the inferior thyroid artery and vein can sometimes be seen. Color Doppler enhances the identification of blood vessels and flow. The esophagus is sometimes detected behind the thyroid and left of center, anteromedial to the longus colli muscle. It can be observed to distend after the patient swallows a sip of water. Lymph nodes can be seen normally as less than 1 × 3 mm, elliptical, uniform structures with an echo-dense central hilum. The parathyroid glands are not visualized unless they are enlarged. They are less dense to ultrasound than the thyroid gland because of the absence of iodine.
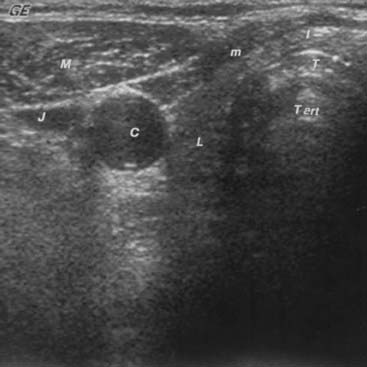
FIGURE 78-5. Sonogram of the neck in the transverse plane, showing a normal right thyroid lobe and isthmus. C, Carotid artery (note the enhanced echoes deep to the fluid-filled blood vessel); I, isthmus; J, jugular vein; L, thyroid lobe; M, sternocleidomastoid muscle; m, strap muscles; T, anterior portion of the tracheal ring (the dense white arc is calcification); T art, artifact in the trachea.
Generally, imaging procedures are not useful in patients whose thyroid gland is normal to palpation unless the patient has a history of exposure to therapeutic irradiation in youth or metastatic thyroid cancer has been discovered and a primary lesion in the gland is being sought. However, in selected circumstances, an ultrasound image may be used to supplement or confirm physical examination findings and identify the size and shape of regional structures accurately and relatively inexpensively. This test is useful when thyroid anatomy is in question but clinical perception is confused by obesity, great muscularity, distortion by abnormal adjacent structures, tortuous blood vessels, a prominent thyroid cartilage, metastatic tumor, lymphadenopathy, prior surgery, or examiner inexperience. On the other hand, the sonogram is so sensitive that many small, nonpalpable thyroid nodules may be detected. Management of these nodules, which are called incidentalomas, requires mature clinical judgment. Objective diagnostic evaluation of all of them is needless and impractical. Selective attention to those found in a patient with a high risk of cancer, those with special characteristics frequently seen in cancers, or those that grow is prudent. Neglecting all of them is inappropriate and occasionally dangerous.
Sonography When There Is Thyroid Enlargement (Goiter)
Enlargement of the thyroid gland is common. In general terms, enlargement may be diffuse and symmetrical, asymmetrical, smooth and uniform, or nodular. It is not generally necessary to obtain a sonogram to confirm thyroid enlargement unless a specific question has attracted clinical concern. Such questions may involve a dominant nodule, a tender spot, focal hardness, or substernal extension. At times, a physician may obtain a sonogram to explain a cryptic finding, such as differentiating goiter from fat or muscle, documenting a controversial observation, estimating the size of the thyroid gland for 131I dosimetry, or assessing volume changes in response to suppressive therapy with thyroid hormone. Sonography has been used in population studies to objectively identify thyroid enlargement as a screen for iodine deprivation.
Sonography can show alterations of the echo pattern of the thyroid gland and its size. Cystic and/or hemorrhagic degeneration, which is depicted by an echo-free zone, is common (Fig. 78-6). These findings are not specific for any particular type of pathology. However, sonography can identify one region in a uniform goiter whose echo pattern is different from the rest of the goiter, which is suggestive of a focal lesion, especially if that focus is surrounded by a distinctive rim or halo.
Sonography in Patients With Thyroiditis and Graves’ Disease
The greatest value of ultrasonography in patients with immune or inflammatory thyroid disease is to identify incidental focal lesions. However, because most focally distinct zones in these glands are not neoplastic, the need for their subsequent management requires judgment. In situations in which localized firm consistency, focal enlargement, or pain call attention to a part of Graves’ or Hashimoto’s goiter, or if a scintigram shows a cold area, a sonogram may demonstrate a region that has a distinctive appearance, which should be subjected to accurate aspiration biopsy (Fig. 78-7).

FIGURE 78-7. Sonogram of the right lobe of the thyroid gland in the longitudinal plane from a 33-year-old, 235-pound woman. The serum contained high titers of antithyroid antibodies. The thyroid gland was difficult to palpate, and examiners could not agree on the findings. Therefore, a sonogram was done. It shows a 7.7 × 10.0-mm nodule (× and + symbols) that is less echo-dense than the rest of the thyroid lobe. Fine-needle aspiration biopsy demonstrated and surgery confirmed papillary carcinoma. L, Thyroid lobe.
Sonography may demonstrate an image of the thyroid gland that correlates with subacute thyroiditis, Hashimoto’s thyroiditis, and Graves’ disease, but such correlation is of debatable practical diagnostic importance. Several types of thyroiditis show reduced echogenicity. During the active phase of subacute thyroiditis, the echogram is characterized by a severely reduced echo density of the thyroid gland that returns to a normal pattern with healing.27 Some patients with Hashimoto’s thyroiditis have low echogenicity (see Fig. 78-7). Marcocci and co-workers reported that only 44 of 238 (18.5%) patients with autoimmune thyroiditis had diffuse hypoechogenicity, especially when they were hypothyroid.28 The accuracy of a heterogeneous, hypoechoic sonographic pattern in diagnosing Hashimoto’s thyroiditis was compared to that of antithyroid peroxidase antibody thyroid peroxidase antibody (TPOAb) concentration in 451 ambulatory patients with unknown thyroid status, excluding those with suspected hyperthyroidism or who were on drugs known to cause hypothyroidism. There was high intraobserver and interobserver agreement on the abnormal thyroid ultrasound patterns, which were judged highly indicative of autoimmune thyroiditis and allowed the detection of thyroid dysfunction with 96% probability.29 Furthermore, in another investigation, patients with postpartum thyroiditis who had both high levels of antithyroid peroxidase antibody and a hypoechoic thyroid gland also had a high risk of long-term thyroid dysfunction.30 Graves’ disease goiters and a few goiters without thyroid autoantibodies have a similar appearance. In Graves’ disease, color Doppler imaging can detect diffuse hyperemia in the thyroid gland,31 a condition that has been called a “thyroid inferno.”32 Increased flow velocity in hyperthyroid patients has been demonstrated with duplex Doppler techniques.33 However, neither the sensitivity nor the specificity of these observations is known.
Sonography of the Thyroid Nodule
Thyroid nodules are identified by sonography because they distort the uniform echo pattern or the shape of the gland. Most nodules have a less dense appearance than normal thyroid tissue does. Most of the remainder are more echogenic, and isoechogenicity is less common. Some nodules have a sonolucent rim called a halo. Nodules may contain regions of calcium (Fig. 78-8) that are extremely echo-dense. The echo texture within a small nodule tends to be uniform, but nodules larger than 2.5 cm usually have irregular zones that are free of echoes. These areas represent cystic and/or hemorrhagic degeneration that may occur in benign or malignant nodules (see Fig. 78-6). Such nodules are called complex. Careful examination of echo-free zones is necessary to discern internal echoes that represent septa or small solid regions that differentiate common, complex cystic nodules and a true thyroid cyst. A cyst is encountered once in approximately 500 to 1000 nodules and is globular shaped, smooth walled, and without internal echoes.
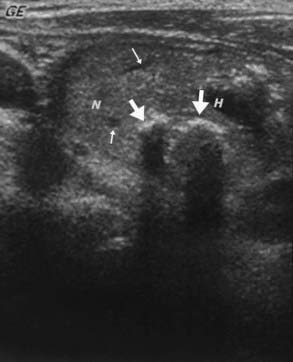
FIGURE 78-8. Sonogram of the neck in the longitudinal plane, showing a large nodule. The small arrows point to echo-free zones that Doppler examination identified as small blood vessels. The thick straight arrows point to calcifications. Note that passage of the ultrasound signal distal to the calcium is blocked in a linear fashion and creates an artifact. H, Hemorrhagic/cystic degenerated area; N, nodule.
The prevalence of palpable thyroid nodules in members of the general population who are screened by palpation is 1.5% to 6.4%.34 It is 10-fold greater when they have been screened by ultrasonography.35 The prevalence of sonographically detectable nodules increases with age to around 50% in older adults. The risk of malignancy of palpable nodules is 5% to 15%; in ultrasonically detected nonpalpable nodules, the risk is smaller.36 The major use of ultrasonography is to determine which of the many nodules are the relatively few malignancies. Sonography can help in this triage, but the ultrasonic appearance of a nodule cannot reliably differentiate benign lesions and cancer.37 Table 78-3 lists the sonographic features of a nodule that are associated with high or low risk of thyroid cancer. Cancers may be minute or large, entirely solid or complex. Some features of a nodule can be helpful to select nodules that are likely malignant. The most reliable ultrasonic predictor of malignancy is vascular invasion, but this feature is observed uncommonly. Adenopathy associated with a nodule is also very good evidence, providing there is no other reason for enlarged nodes such as infection, as will be discussed later. It is important to realize that in children, adenopathy is a relatively nonspecific finding and must be interpreted with caution. The characteristics of nodules that studies have shown most useful for identifying carcinomas include the intensity of the echoes, the lack of sharpness and irregularity of the boundary of the nodule, the presence of an incomplete “halo” or calcifications, and internal structure, including vascularity.38,39 However, there is considerable variation in the cancer-predictive value of these characteristics. The most optimistic data is a 97.2% positive predictive value for cytologically diagnosed cancer and 96.1% predictive value for benign disease among 1244 nodules in 900 patients who were stratified according to ultrasound characteristics on a scale of 1 to 5 assessing cancer-risk.40 The author is considerably less confident. As a group, malignancies tend to be rather hypoechoic.44,45 In one study, 62% of cancers were hypoechoic among 202 patients with nodules, and few were hyperechoic.41 In another series, none of the 14 cancers were hyperechoic among 132 consecutive ultrasound-guided fine-needle aspiration biopsies.42 However, most benign nodules are also of low echo density. Nevertheless, it can be said that hyperdense nodules are probably not cancerous and need not be biopsied unless there are other factors that indicate a high risk of cancer.43 Internal cystic spaces in thyroid nodules are degenerative and have no cancer-predictive value. In distinction, cystic space in lymph adenopathy is important because it may be seen more often with thyroid cancer than in inflammatory nodes. Deposits of calcium may be seen in benign or malignant nodules. Frequently, large irregular plaques or eggshell calcifications are found, and because benign nodules are more common than malignant ones, these concretions do not correlate with cancer. In distinction, punctate calcifications or microcalcifications are not common in nodules but have high specificity for thyroid cancer (95.2%), low sensitivity (59.3%), and a diagnostic accuracy of 83.8%.36 They may represent psammoma bodies in papillary cancer. A halo around a nodule is thought to represent a boundary, capsule, or vasculature that may be seen in benign or malignant conditions.44,45 Demonstrating in multiple images and in several planes that a halo is incomplete correlates with cancer, but the finding is of low specificity and sensitivity. Lack of distinctness of a nodule has little diagnostic value, but an ill-defined edge has been reported with infiltrating, poor-prognosis lesions.46 In general, the shape of a nodule has limited diagnostic significance except that cancers tend to exhibit a tall and thin shape. The patterns of blood flow as depicted by Doppler examination offer insight into the potential for malignancy. An internal or central flow pattern in a hypofunctioning (“cold”) nodule or lymph node should raise one’s suspicion of malignancy. In one study of 125 nodules, 55 of 92 (60 percent) cold nodules had a peripheral flow pattern, 34 no internal flow, and only 3 had increased internal flow. All 3 cold nodules with an enhanced internal color flow pattern were carcinomas. However, among the 27 patients who had pathology correlation, there were a total of 7 cancers, only 3 of which had increased internal flow; the other 4 had either diffuse or no internal flow.47 Another study of 203 patients, the addition of color flow Doppler imaging to conventional sonography only slightly increased the screening sensitivity and accuracy from 71.9% to 83.3% in identifying the 36 malignant thyroid nodules.48
Table 78-3. Ultrasonographic Features of a Thyroid Nodule and the Risk of Thyroid Cancer
| Increased Risk of Thyroid Cancer | Decreased Risk of Thyroid Cancer |
|---|---|
| Hypoechoic | Hyperechoic |
| Microcalcifications | Large, coarse calcifications (except medullary cancer) |
| Central vascularity | Peripheral vascularity |
| Irregular margins | Looks like Napoleon or puff pastry |
| Incomplete halo | Comet-tail shadowing |
| Nodule is taller than wide | |
| Documented interval enlargement of a nodule | |
| Associated rounded adenopathy (especially with cystic spaces) |
Ultrasonic features of a nodule that specifically favor benign disease include hyperechogenicity and characteristics that suggest the presence of abundant colloid accumulation within the nodule. A “Napoleon” or puff-pastry, layered appearance of the nodule, or a bright spot with a trailing, fading comet tail have been reported with colloid nodules.
Thyroid palpation might not accurately predict the need for sonography in patients with a thyroid nodule. One suspects that routine sonography will be employed, especially when palpation is uncertain or skills are tentative.
Evidence is mounting in support of routine sonography for patients with palpable uninodular thyroid disease with or without a palpable goiter. Thyroid ultrasonography has been reported to show that among 114 patients who were referred because of a solitary thyroid nodule, ultrasonography detected additional nonpalpable thyroid nodules that were at least 1 cm in diameter in 27 patients and no nodules in 23. In this investigation, sonography provided information to the clinician that importantly altered management in 63% (109 of 173) of patients who were referred to a tertiary endocrine group. Sonography showed an indication for needle aspiration or demonstrated that the procedure was not necessary. Among 59 patients who were referred because of goiter, sonography revealed nonpalpable nodules that were at least 1 cm in diameter in 39 patients, requiring aspiration that was not anticipated.49
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree