FIGURE 32-1 Amino acid sequence of human and hagfish insulins, with substitutions occurring at each position in 70 other known vertebrate insulins shown below for comparison. Invariant residues are enclosed in boxes.
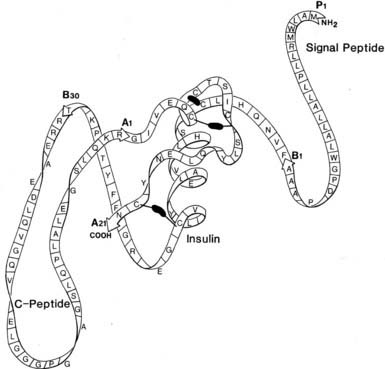
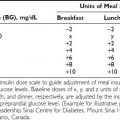
FIGURE 32-2 Schematic structure of human preproinsulin. Rapid removal of the first 24 amino acids (signal peptide) gives rise to proinsulin, which then folds to form the native insulin domain stabilized by three disulfide bonds (black bars). The connecting segment is not structurally organized. Cleavage after B30 (T) and before A1 (G) then gives rise to insulin and the free C peptide. (See text for details.)
MORPHOLOGIC ORGANIZATION OF THE INSULIN BIOSYNTHETIC MACHINERY
The β cells of the islets of Langerhans share many features with other endocrine and neurosecretory cells. Preproinsulin is the initial translational product of insulin mRNA, as discussed earlier, and is rapidly cleaved to proinsulin in the RER. After folding and disulfide oxidation, proinsulin is transported from the ER to the Golgi apparatus in small coated vesicles20 (Fig. 32-3) in an energy-dependent process that requires about 20 minutes.22,24,25 The biochemical basis of the energy requirement for the intracellular transport of secretory proteins is associated with the budding and/or fusion of small vesicles that transfer secretory products from the ER to and through the cis to trans Golgi cisternae.26,27
FIGURE 32-3 Schematic model of the subcellular transport of preproinsulin after its synthesis on membrane-bound ribosomes of the rough endoplasmic reticulum (RER) and rapid cleavage to proinsulin (within 1 to 2 minutes). Proinsulin is then released into the intracisternal spaces of the RER, where it folds and forms the native disulfide bonds of insulin. It is then transported to the Golgi apparatus by an energy-dependent process. The clathrin-coated early granules budding from the trans-Golgi cisternae are rich in proinsulin and contain the converting proteases, PC2 and PC1/3. Processing occurs mainly, if not exclusively, in the early secretory granules24,30 giving rise to the more condensed mature granules. Fractionation studies have confirmed that the mature granule-dense cores consist almost entirely of insulin, often in crystalline arrays (see Fig. 32-9), whereas the granule-soluble phase that surrounds the inclusion consists mainly of C peptide and small amounts of proinsulin.84 The release of newly synthesized proinsulin and insulin begins only about 1 hour after synthesis in the RER; hence, granules must undergo a maturation process that renders them competent for secretion. There is no evidence for significant nongranular routes of secretion of either proinsulin or insulin in normal islets. Exocytosis of granules is regulated by glucose and many other factors (see section on insulin secretion), and in humans and dogs, it results in the release of insulin and C peptide in approximately equimolar proportions under both basal and stimulated conditions.95 The mechanism of recycling of the granule membrane and its components is not well understood.
The role of the Golgi apparatus in forming insulin-containing secretory vesicles, or β-granules, was first recognized in the 1940s and subsequently confirmed and extended by Munger,28 who used electron microscopy to identify pale, homogeneous-appearing, immature “progranules” near the Golgi body. The structural organization and various functions of this complex organelle continue to engage the attention of cell biologists and biochemists.29 Orci and coworkers demonstrated that these newly formed clathrin-clad vesicles are derived from the trans-Golgi network (TGN) cisternae and contain a high proportion of proinsulin, definitively confirming their proposed role as the major sites of proinsulin processing to insulin.30 Conversion of proinsulin to insulin in vivo behaves kinetically as a pseudo–first-order reaction having a half-time ranging from about 20 minutes to 1 hour.22,31,32 Peak labeling of proteins in the Golgi apparatus occurs 30 to 40 minutes after pulse labeling islets with 3H-amino acids, and relatively little radioactivity remains in this region after 1 hour.33 A similar pattern for proinsulin is observed by means of electron microscopic immunocytochemistry. Thus, although small amounts of proinsulin conversion may be initiated in the TGN, most of it occurs in newly formed secretory vesicles, or progranules, which mature biochemically in the cytosol30 (see Fig. 32-3). Numerous subsequent studies have confirmed that newly synthesized neuroendocrine precursor peptides pass via the Golgi apparatus into secretory granules of the regulated secretory pathway, where they are cleaved and processed to their mature products and then stored until secretion in response to signals such as glucose.10
STRUCTURE AND PROPERTIES OF PROINSULIN
Mammalian proinsulins range in size from 81 (cow) to 86 (human, horse, rat) amino acid residues, owing to variations in the length of the C peptide. Various C-peptide sequences are compared in Fig. 32-4. Proinsulin is closely similar to insulin in many properties, including solubility, isoelectric point,22 self-associative properties,34 and reactivity with insulin antisera.11,35 Indeed, the conformation of the insulin moiety in proinsulin is essentially identical to that of insulin itself.36 It is noteworthy that the highly flexible C peptide is much longer than necessary simply to bridge the short 8-Å gap between the ends of the B and A chains as they exist in the folded insulin molecule (see Fig. 32-2). The C-peptide segment overlays a portion of the surface of the insulin monomer, reducing its potency to about 3% to 5% of that of insulin in vitro,22,37 and it undergoes little if any proteolysis or activation in the circulation or tissues.38 The presence of the C peptide in proinsulin also does not prevent the dimerization or hexamerization of its insulin moiety39 (Fig. 32-5). It lies outside the zinc-stabilized globular insulin hexamer in a disordered loop, as assessed by nuclear magnetic resonance (NMR) spectroscopy. Since low levels of proinsulin can form mixed hexamers with insulin, it can be efficiently incorporated into insulin crystals.40 This property accounts for the presence of 1% to 2% of proinsulin in most crystalline preparations of insulin prepared from animal pancreata.41 However, x-ray analysis of crystals of proinsulin have failed to reveal any details regarding the structure of the C-peptide segment.42,43
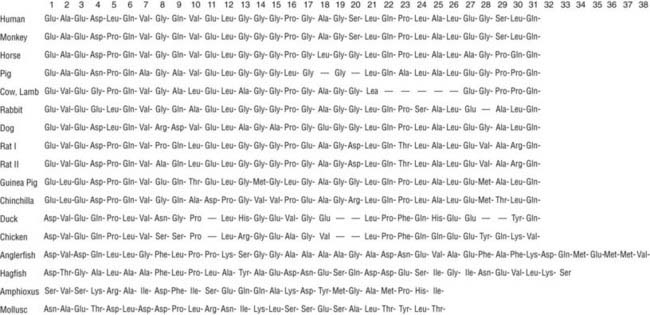
FIGURE 32-4 Compilation of amino acid sequences of proinsulin C peptides in vertebrates, amphioxus, and in a mollusk, Lymnae stagnalis (for sources see Ref. 96).
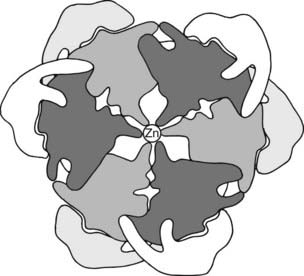
FIGURE 32-5 Hypothetical 2-Zn proinsulin hexamer as viewed along the threefold axis. The connecting peptide is shown in light gray and white around the periphery of the darker outline of an insulin hexamer arranged according to the structural data of Blundell et al.88 The central density represents two zinc atoms in coordination linkage to the six (three above and three below hexamer plane) histidine side chains at position 10 in the B chain.
The major intermediate cleavage products of proinsulin consist mainly of forms cleaved at only one site and lacking the exposed basic residues (i.e., des-31,32 or des-64,65 intermediates).12,22,41,44,45 Their relative ratios in the circulation differ among species, depending on differences in the amino acid sequences surrounding the cleavage sites.46 Proinsulin-like proteins having comparably sized C peptides have been found throughout the vertebrates and also in a variety of invertebrates. Although it seems likely that the single-chain insulin-like growth factors, IGF-1 and IGF-2, arose from a single proinsulin-like gene in protochordates,47 some invertebrates, such as Caenorhabditis elegans,48 have numerous insulin-like peptides that lack defined C peptides and typical paired basic residue sites for cleavage by the evolutionarily well-conserved prohormone convertases.
ENZYMATIC BASIS OF THE CONVERSION OF PROINSULIN TO INSULIN
The major proteolytic cleavages required for converting proinsulin to insulin are summarized in Fig. 32-6. In early studies, it was shown that the joint action of pancreatic trypsin and carboxypeptidase B gives rise to the naturally occurring conversion products—C peptide and native insulin in high yields—quantitatively converting proinsulin to insulin in vitro.49 This model also explains the major intermediate forms found in pancreatic extracts,44,50 and it led to a search for a cellular trypsin-like convertase, assumed to be a serine protease related to trypsin,22 and for carboxypeptidases related to carboxypeptidase B, an exocrine pancreatic exopeptidase with specificity for C-terminal basic residues.49 Early studies with isolated islet secretory granules revealed that these were major sites of proinsulin conversion, and that conversion resulted in the release of insulin along with free arginine, rather than basic dipeptides,51 confirming the likely participation of both trypsin-like and carboxypeptidase B–like proteases in maturing secretory granules.52 Carboxypeptidase E (or H), a homolog of carboxypeptidase B but with a more acidic pH optimum, was first identified in islets52 and subsequently by Fricker in brain.53 Molecular cloning confirmed its structural and evolutionary relationship to the pancreatic carboxypeptidases. Additional processing carboxypeptidases have been uncovered in brain and other tissues.54
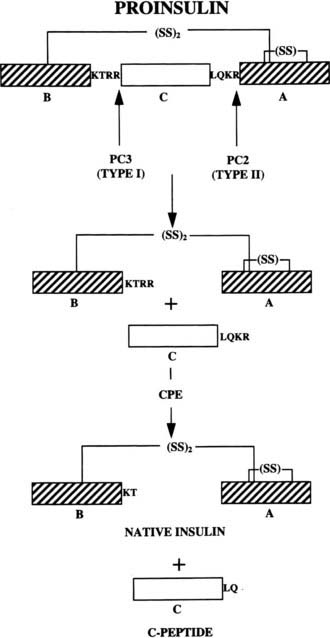
FIGURE 32-6 The cleavage of proinsulin to insulin by the combined action of the subtilisin-like prohormone convertases, PC2 and PC1/PC3, and carboxypeptidase E. (See text for details.)
The first authentic processing endoprotease, kexin, was identified through studies on the processing of the yeast alpha mating–factor precursor and proved to be a calcium-dependent serine protease related to bacterial subtilisin and the subtilases rather than to trypsin.55–57 This information enabled the discovery of mammalian homologs, which form a family of seven closely related endoproteases with differing points of action within the secretory pathway.10,58,59 These have been designated as subtilisin-like proprotein convertases (SPCs), or more simply as PCs. Two members of this family, PC1/3 and PC2, have proven to be the principal effectors of neuroendocrine peptide precursor processing and are largely confined in their expression to brain and endocrine tissues in most animal species.10 For further information on the extended SPC/PC family and its multiple functions, please see the reviews in Refs. 60 to 62.
Role of PC2 and PC1/3 in Proinsulin Processing
Both PC1/3 and PC2 are required for proinsulin processing and have been shown to be identical with the calcium-dependent type I and type II insulinoma granule-processing activities, respectively, originally described by Davidson et al.63 The importance of calcium for the transport and proteolytic maturation of proinsulin has been well documented.64 The role and order of action of PC2 and PC1/3 in proinsulin conversion has also been carefully studied.65 Rhodes et al.66 demonstrated that the type II convertase (PC2) prefers the proinsulin intermediate that has already been processed at the B chain–C peptide junction (des-31,32 intermediate) as a substrate. This observation has led to the scheme for conversion outlined in (Fig. 32-7), in which PC1/3 acts first to generate the des-31,32 intermediate, which is then cleaved at the C peptide–A chain junction by PC2. This order of cleavage is consistent with observations that PC1/3 achieves an enzymatically active form more rapidly than PC2 and has a somewhat higher pH optimum. Thus, PC1/3 may begin cleaving proinsulin as it is concentrated into immature secretory vesicles in the TGN, whereas PC2 acts only in the maturing granules as the pH decreases to around 5.5. According to this scheme, PC1/3 plays a more important role in proinsulin processing, as born out by observations on islets from mice lacking PC2 or PC1/3.46,67–69
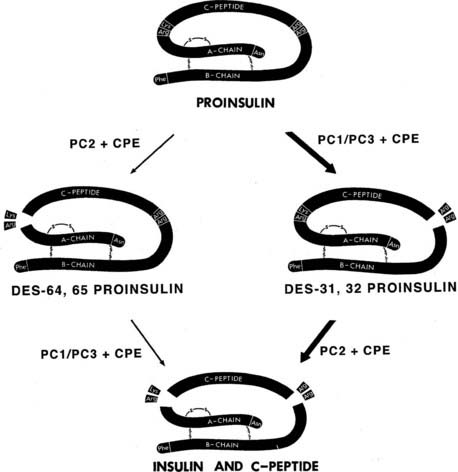
FIGURE 32-7 Routes of processing of proinsulin in the pancreatic β cell. The pathway on the right is probably more dominant under normal conditions because des-31,32 proinsulin is a preferred substrate for PC2,66 and the more acidic pH optimum and slower maturation of this enzyme may delay its action during the initial phases of secretory granule maturation. The C-terminal basic residues are removed by CPE (CPH) after endoproteolytic cleavage by the PCs.
(Modified from Rouillé Y, Duguay SJ, Lund K et al: Proteolytic processing mechanisms in the biosynthesis of neuroendocrine peptides: the subtilisin-like proprotein convertases, Front Neuroendocrinol 16:322–361, 1995.)
PC2-null mice are not diabetic, but they exhibit significant hyperproinsulinemia, with plasma proinsulin levels in the range of 60%.67 Pancreatic extracts also show increased proinsulin levels, but only in the homozygous nulls, as indicated in Table 32-1. Pulse-chase studies of insulin biosynthesis in isolated islets, comparing PC2(−/−) mice with wild-type (WT) controls, also confirm significantly slower processing of proinsulin to insulin, with accumulation of significant amounts of des-31,32 intermediate proinsulin.46,67 Approximately a third of the labeled proinsulin remains after a 3- or 4-hour chase, consistent with the levels found by radioimmunoassay in pancreatic extracts. Thus in normal mice, PC2 converts at most about a third of the available proinsulin, while PC1/3 is responsible for processing the remaining two-thirds.69
Table 32-1 Percent Proinsulin-Like Immunoreactivity in Pancreatic Extracts of Wild-Type, PC2-Null, and PC1/3-Null Mice
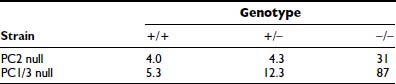
A human subject with inactivating mutations in both copies of the PC1/3 gene has been reported.70 This 43-year-old woman is obese and had gestational diabetes. Examination of the subject’s serum revealed no detectable circulating insulin, in association with greatly elevated intact proinsulin and significant amounts of des-64,65 intermediate proinsulin but little or no des-31,32 intermediate proinsulin. Similar results with respect to proinsulin processing have been reported for the PC1/3-null mouse, which has very high levels of proinsulin and elevated des-64,65 intermediate proinsulin68,69 (see Table 32-1). This picture is consistent with the conversion scheme outlined in Fig. 32-7 and indicates that the pathway shown on the right side of the diagram is the predominant one. It also confirms the likelihood that PC1/3 is the more important convertase in the processing of proinsulin. The PC1/3-null mice, however, are not obese like the human subject; instead, they exhibit a severe growth defect, most likely due to lack of normally processed growth hormone–releasing hormone.69 These mice are also unable to produce GLP-1 but did not have altered intraperitoneal glucose tolerance. Altered proopiomelanocortin processing and other endocrine abnormalities, as well as intestinal malfunction, also are present in these mice.68
Significance of Circulating Proinsulin and Des-31,32 Intermediate in Man
An important clinical issue concerns observations that in man, des-31,32 intermediate proinsulin is a major intermediate, making up a very significant proportion of the circulating proinsulin-like material.71 It has been suggested that the elevated accumulation of proinsulin and des-31,32 proinsulin in diabetics might be due to defective action of PC2.72 Isolated normal human islets of Langerhans also have been reported to convert proinsulin to insulin with significant accumulation of des-31,32 intermediate, despite the presence of normal levels of PC2.73 However, des-31,32 intermediate only reaches levels of 15% to 20% of total immunoreactive insulin-like material during biosynthetic pulse-chase studies in the islets of PC2-null mice.46 Thus, even the complete absence of PC2 should not in itself give rise to such high levels of this intermediate as are seen in human serum samples. It has recently been clarified that this phenomenon arises due to the faster rate of cleavage by the PCs of substrates having a basic residue in the fourth position upstream (P4 position) of the usual dibasic cleavage sites. Such an upstream basic residue is present at the B chain–C peptide junction in human proinsulin (B29 is Lys) but is lacking at the A chain–C peptide junction (C62 of proinsulin is Leu) (see Fig. 32-6). This causes an imbalance in the relative susceptibility of these two sites to either of the two convertases and tends to favor the accumulation of the des-31,32 intermediate.46 On the other hand, in the dual proinsulins of rats and mice,22 other P4 sequence changes in these cleavage sites produce different ratios of intermediates than those seen in man.46
Studies on the regulation of the biosynthesis of PC2 and PC1/3 in β cells suggest that the rates of translation of both of these enzymes are up-regulated by glucose, similar to that of proinsulin on glucose stimulation.74 Also both PC2 and PC1/3 mRNA levels are equally elevated along with insulin mRNA during more prolonged stimulation of islets with glucose.75 However, under conditions of chronic stimulation, a relative deficiency of PC2 could develop that could exaggerate the abnormalities in circulating proinsulin intermediates seen in diabetics. Accordingly, the normal accumulation of des-31,32 intermediate proinsulin in human subjects merely reflects sequence differences in the two cleavage sites of human proinsulin, whereas increased levels of both proinsulin and des-31,32 proinsulin in prediabetics and diabetics may result from a deficiency of convertase action when islets are stressed by hyperglycemia. Genetic studies have not yet indicated a major role for mutations in the PC1/3,76 PC2,77 or CPE78 genes in susceptibility to any form of diabetes, although common amino acid polymorphisms in PC1/3 may increase risk of obesity.79 However, loss-of-function mutations in the transcription factor PAX6 have recently been described which result in reduced expression of PC1/3 in the islets and are associated with hyperproinsulinemia and mild age-related diabetes.80
SECRETORY GRANULE FORMATION AND MATURATION
One of the unsolved puzzles of neuroendocrine and other secretory cells is the nature of the mechanism underlying the efficient sorting of proteins destined for regulated secretion into immature secretory vesicles in the TGN. In the β cell, this process is remarkably efficient, resulting in very low levels of unregulated or “constitutive” release of proinsulin (<1% to 2%). However, the newly formed secretory granules have a clathrin coat (Fig. 32-8) which appears to be involved in some reorganization of the granule contents after and/or during their formation in the TGN.81 This passive sorting presumably occurs via small clathrin-clad vesicles that transport some proteins that are excluded from the condensing granule cores into endosomal pathways that either recycle to the TGN or to the cell surface. As a consequence of this “constitutive-like” pathway, proteins such as furin, procathepsin B, and possibly others briefly pass through the immature granule compartment, where they may play an active albeit transient role (e.g., furin may participate in processing of some prohormones).81,82 Also, small amounts of abundant soluble granule components such as proinsulin and/or C peptide may exit the granules within these vesicles.83 Passive sorting may also play a role in maintaining synchrony between granule membrane area and granule volume as maturation proceeds.81
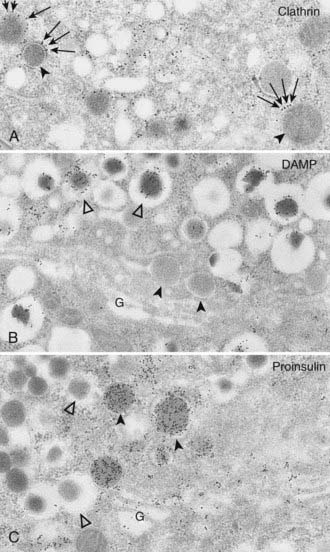
FIGURE 32-8 A, Clathrin immunolabeling; B, 3-(2,4-dinitroanilino)-3′-amino-N-methyldipropylamine (DAMP) immunolabeling; and C, proinsulin immunolabeling of Golgi areas (G) of B cells (protein A–gold techniques). These electron micrographs show that the population of secretory granules with tightly fitting cores (black arrowheads) is clathrin coated (arrows in A), DAMP poor (B), and proinsulin rich (C). These granules correspond to the maturing coated secretory granules freshly released from the Golgi complex. Conversely, secretory granules with wide, clear halos (white arrowheads) are deprived of clathrin (not shown here), are DAMP rich (B). and are proinsulin poor (C). These correspond to the noncoated mature (storage) insulin-containing secretory granules. Because DAMP immunoreactivity is assumed to represent an indirect measure of intraorganelle acidity, this may indicate a decreasing pH gradient between proinsulin-rich and insulin-rich granules (i.e., between the converting and the storage compartments) (A, ×28,000; B and C, ×27,000).
(From Orci L: The insulin cell: its cellular environment and how it processes proinsulin, Diabetes Metab Rev 2:71, 1986.)
Newly formed secretory vesicles in neuroendocrine cells undergo biochemical and morphologic maturation to typical dense-core granules. In β cells, the progranules are larger, less dense, and more uniform in appearance.29,30 The most important biochemical change taking place as these progranules mature is the proteolytic conversion of proinsulin to insulin, accompanied by reorganization of the products.30 Electron microscopic studies indicate that they progressively acquire a crystalline dense central core (Fig. 32-9). High magnification reveals repeat-unit spacings in the cores that are closely similar to those observed in ordinary zinc insulin crystals.84 Thus, as insulin is liberated from proinsulin, it tends to crystallize with zinc that is concentrated by the β cells. Recent studies have demonstrated that zinc is taken up into maturing granules via the ZnT8 zinc transporter, and they do not assume the normal dense-core appearance in its absence, even though proinsulin conversion is not impaired.85 Biochemical fractionation of mature islet secretory granules confirms that the cores contain only insulin, whereas the C peptide liberated in the conversion process remains in solution in the clear fluid space surrounding the dense crystalline core.84 There is no evidence for co-crystallization of the C peptide with insulin under these conditions or in vitro.
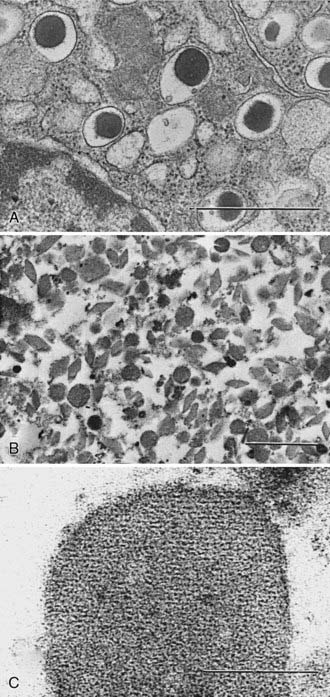
FIGURE 32-9 A, Photomicrograph of normal rat β cells (×28,000) showing morphology of mature granules (bar = 1 µm). B, Isolated rat β-granule cores (×17,000)236 (bar = 1 µm). C, High-magnification view (×250,000) showing repeat unit structure of a crystalline core (bar = 0.1 µm). The cores are made up of both rat insulin I and II in approximately equal proportions (Michael J and Steiner DF, unpublished data). Samples were fixed with Karnovsky’s solution and stained with osmium tetroxide.
(Electron micrographs courtesy Hewson H. Swift.)
Most of the zinc in islets is present in the β granules and is liberated proportionately to insulin during secretion, in keeping with its role in crystallization of the hormone.86 The insulins of some species, including the guinea pig, coypu, and other hystricomorph rodents42 and the primitive hagfish,87 lack the histidine residue at position 10 of the B chain required for zinc binding during the association of insulin dimers into hexamers.88 A human subject heterozygous for a mutation at B10 (His B10 Asp) had elevated levels of this proinsulin in the blood because it tended to be released constitutively at much higher levels than normal proinsulin.89 However, in a transgenic mouse model of this mutation, there was no defect in its conversion to insulin in the granules, despite its altered self-association and sorting properties.90
The pH of the interior of the mature secretory granule appears to be between pH 5.0 and 6.0,51,91 an optimal pH range for insulin crystallization in vitro. The neutral or slightly alkaline pH in the cisternal spaces of the RER favors proinsulin folding and sulfhydryl oxidation. The pH remains near neutral throughout the Golgi apparatus but becomes more acidic (pH 6.1) in the TGN as the secretory products are sorted into granules and proteolytic processing begins. Vesicular proton pumps may begin to increase the uptake of protons, which then displace the cationic arginine and lysine residues liberated during conversion. As these move out of the granules and are replaced by hydrogen ions, a downward shift in intragranular pH may occur. Thus the initially mildly acidic progranules91 undergo gradual acidification as they mature in the cytosol (see Fig. 32-8), creating appropriate conditions for the conversion and crystallization of the newly formed insulin. One recently discovered role of the constitutive pathway convertase, furin, in the β cell is to activate the proton pump, which acidifies the secretory granules. As a result, proinsulin processing is impaired in β cells lacking furin.92
The cellular processes related to the biosynthesis of insulin via preproinsulin and proinsulin and their intracellular transport, sorting, proteolysis, and ultimate storage in secretory granules are remarkably well integrated, both topologically and biochemically. This delicately poised integration of processes leading to the formation and storage of insulin is disturbed in islet cell tumors, which often show unregulated release of insulin together with large amounts of proinsulin; measurements of the latter can provide a useful diagnostic indicator93 (see Chapter 47).
BIOSYNTHETIC ROLE AND BIOLOGICAL ACTIONS OF THE C PEPTIDE
Because of its cosecretion with insulin in essentially equimolar amounts,22,94,95 the C peptide has been of great value as a marker of insulin secretion in humans under a variety of conditions. Representative vertebrate C-peptide amino acid sequences are compared in Fig. 32-4.96 These peptides exhibit a 15-fold higher rate of mutation acceptance than do the corresponding insulins, a finding that has often been interpreted as indicating that this region in the proinsulin molecule is unlikely to have any specific hormonal function. Nonetheless, several acidic residues are consistently present at certain positions in mammalian C peptides. These offset the added cationic charges due to the pairs of basic residues at the proinsulin cleavage sites, such that the isoelectric pH of proinsulin is nearly the same as that of insulin (i.e., in the range of pH 5.1 to 5.5).22
A large body of evidence supports a biosynthetic role for the C-peptide segment in proinsulin. Primarily, it converts the insulin A and B chain interaction from an inefficient bimolecular reaction to a highly efficient and concentration-independent unimolecular reaction.97 Certain regions of the connecting peptide may also facilitate the folding of the proinsulin polypeptide chain and the formation of the correct disulfide bonds, or guide the enzymatic cleavage of proinsulin to insulin by helping to orient the basic residue pairs for efficient binding and cleavage by the convertases.98,99 Recent molecular modeling studies indicate that the C peptide may assist in achieving important conformational changes in the N-terminal helical region of the A-chain segment, aiding its interaction with the convertases during processing.100
The conservation of a length of 30 to 35 amino acids in almost all proinsulin C peptides, including those of insects, mollusks, and nematodes, despite the short 8- to 10-angstrom separation between A1 and B30 in the native insulin molecule88 (see Fig. 32-2), supports the existence of an important length-related function. Since much shorter connecting segments do not impair sulfhydryl oxidation and formation of the native structure,99,101 it is clear that this is not a critical constraint. A highly plausible reason for the evolutionary retention of a relatively long C peptide in proinsulin may be to facilitate the translocation of proinsulin across the RER membrane during its synthesis. The length of polypeptide chain required to span the large ribosomal subunit and the RER membrane has been estimated to be about 65 residues in extended configuration.102 Moreover, the arrest of translation by the signal recognition particle (SRP) occurs only after synthesis of a nascent chain of about this length and thus may play a role in translational control of insulin biosynthesis.102 Efficient intracellular transport and correct targeting to secretory granules may impose additional demands on the primary (and tertiary) structure of proinsulin and other precursor proteins. However, miniproinsulins with deleted or greatly truncated C peptides do not fold efficiently but are correctly targeted to the regulated secretory pathway.98,101,103
Another very important function of the C-peptide is to facilitate its removal from proinsulin after it has served its biosynthetic functions, as mentioned earlier. The kinetics of insulin metabolism in vivo, as well as its biological activity, are both dependent upon its high affinity for the insulin receptor. Proinsulin’s much lower receptor-binding affinity leads to a much slower rate of clearance, which explains its relatively higher apparent biological activity in vivo. The rapid clearance of insulin is adaptively as important a characteristic as its bioactivity. To assure its interaction with the convertases, proinsulin must present more than just a pair of basic residues to the convertases. Their active sites require an extended β strand that is at least eight residues in length for recognition at each cleavage site. Molecular modeling studies have suggested how the full length of the connecting segment contributes to achieving the necessary conformations for effective proinsulin binding and cleavage by the convertases.100
Since the early 1990s, a number of reports have appeared describing a variety of biological actions of the C peptide and/or smaller peptides derived from it.104 These putative effects include enhancement of glucose transport and utilization; improvements in microcirculation in muscle, skin, retina, and nerve in diabetics; and stimulation of renal tubular Na+,K+-adenosine triphosphatase (ATPase) activity and other parameters of renal function. It has been suggested that tissue receptors for C peptide might exist, and that the circulating C peptide may contribute to improved glycemic control and help to slow the development of the vascular and neural complications of diabetes.105 Further study is needed in this area in view of reports that some C-peptide effects do not follow the usual rules of ligand-receptor chemistry (i.e., chirality does not matter). Thus, a C peptide synthesized entirely of d amino acids is equally as active as a peptide made with l amino acids in reversed order,106 whereas a random sequence of the same amino acids leads to loss of activity. These tantalizing findings suggest the need for a controlled clinical trial of combined insulin and C-peptide therapy in diabetics to fully evaluate its therapeutic potential.
The availability of biosynthetic human proinsulin and insulin, as well as of human C peptide, has opened many new possibilities for studies of the role, metabolism, and antigenicity of these peptides.107–109 In recent years, active insulin analogs with shortened linking peptides have also been developed. Such miniproinsulins and/or “single-chain insulins” appear to readily oxidize to form correct disulfide bridges and either can be used intact or after cleavage to insulin.98,99,101 Other efforts have been directed towards synthesis of modified insulins with improved absorption, aggregation, and/or pharmacokinetic properties for therapeutic use.
Regulation of Insulin Production
Under normal circumstances the pancreatic β cell retains a remarkable state where insulin secreted in response to a stimulus is rapidly replenished at the biosynthetic level in parallel, thus keeping intracellular insulin stores optimal. The vast majority (98% to 99%) of insulin is secreted via the “regulated” secretory pathway110 and only occurs in response to increases in specific nutrients, certain hormones, neuropeptides, and some pharmacologic reagents.111,112 In general, most nutrients that regulate insulin secretion also control proinsulin biosynthesis,111 and the most physiologically relevant of these is glucose.112 Glucose metabolism is required for both glucose-induced insulin secretion and production,111 but the secondary stimulus-coupling mechanisms are quite distinct. For example, stimulated insulin secretion is Ca2+ dependent, but glucose-induced proinsulin biosynthesis is Ca2+ independent.112,113 There are effective inhibitors of glucose-induced insulin secretion, such as diazoxide, epinephrine, and somatostatin, but these have no effect on glucose-induced proinsulin biosynthesis.111 In contrast, effective stimulators of insulin secretion, such as sulfonylureas and fatty acids, have no effect on proinsulin biosynthesis.111,114 This differential regulation of insulin secretion and proinsulin biosynthesis indicates that glucose-induced proinsulin biosynthesis is not regulated by a positive feedback of locally secreted insulin.113 For stimulated insulin secretion, the intracellular secondary signaling mechanisms are relatively well defined,115 but those for glucose-induced proinsulin biosynthesis, other than a need for mitochondrial metabolism and subsequent succinate production,116 are not currently well understood. However, it is known that both glucose-induced insulin secretion and production can be potentiated by an elevation in [cAMP]i secondary to the action of incretins such as GLP-1.117 The glucose-dependent effect of GLP-1 to increase proinsulin biosynthesis is predominately at the translational level, not at the transcriptional level.118
Glucose regulation of proinsulin biosynthesis is relatively specific and occurs independently of the control of general protein synthesis in the β cell.119 There is a minor subset of β-cell proteins (~50) that are also specifically regulated by glucose at the biosynthetic level in parallel to proinsulin, with these mostly being insulin secretory-granule proteins, including the proinsulin-processing endopeptidases, PC1/3 and PC2.74,75,120,121 This provides a mechanism whereby the enzymes that process proinsulin and the intracellular storage compartment in which insulin is stored are coordinately increased in response to the up-regulation of proinsulin biosynthesis.
The mechanism for specific regulation of glucose-induced proinsulin biosynthesis is complex and can occur at multiple levels depending on the temporal exposure to elevated glucose levels. Under normal fluctuations in glucose concentrations that occur over periods of ≤3 hours, glucose-induced proinsulin biosynthesis is entirely mediated at the translational level.111,113,122,123 For periods of ≥12 hours, this translational regulation is supplemented by glucose promoting preproinsulin mRNA stability124 to provide more preproinsulin mRNA template for translational regulation.113 Longer-term increased proinsulin biosynthesis can also be contributed to by increased insulin gene transcription.125,126
However, even under these longer-term circumstances, the primary control of glucose-induced proinsulin biosynthesis is mediated at the translational level. Yet despite glucose-induced translational regulation of proinsulin biosynthesis being known for nearly 40 years,22,122,127 the molecular mechanism remains unresolved. There are adaptive responses of the general translational machinery to up-regulate preproinsulin mRNA translation that have been shown to occur at the initiation and elongation phases of translation,22,123,127 as well as reduction in the duration of SRP signal peptide–mediated arrest of nascent preproinsulin-chain elongation prior to ribosome docking in the early phases of RER translocation.123 However, the specific translational regulation of proinsulin biosynthesis lies in the preproinsulin mRNA itself, particularly in the untranslated regions (UTRs).128 The 3′ UTR of preproinsulin mRNA contains elements such as a polypyrimidine-rich tract (PRT)129 and a highly conserved UUGAA element111,128 that likely control its stability. The control of preproinsulin mRNA stability via the 3′ UTR PRT also involves a glucose-responsive association of the polypyrimidine tract binding protein (PTB).128 The 5′ UTR of preproinsulin mRNA contains a conserved translational control cis element, ppIGE (for preproinsulin glucose element), that is required for glucose-induced translational control of proinsulin biosynthesis.128,130 The ppIGE has a highly conserved ppIGE “mirrored” core of GUCxnCUG or GUUxnUUG (where n ≤ 4 bases). There is a protein trans-acting factor (ppIE-BP) found in islet cytosolic extracts that binds to this translational control ppIGE cis element of preproinsulin mRNA in a glucose-dependent manner that parallels the characteristics of glucose-regulated proinsulin biosynthesis.130 The identity of the ppIGE-BP is currently unknown. Nonetheless, it is intriguing that the ppIGE is also conserved in the 5′ UTR of the mRNA templates of other secretory granule proteins whose biosynthesis is specifically controlled at the translational level in β cells, including PC1/3 and PC2.98,99 As such, the glucose-induced specific translational control of proinsulin biosynthesis and that for other insulin secretory-granule protein is likely via the same mechanism. For the longer-term transcriptional regulation of insulin gene expression by glucose, this is known to be a Ca2+-dependent mechanism131 involving the putative phosphorylation of key β-cell transcription factors, Pdx-1 and MafA.125 Prolonged glucose stimulation can also lead to increased β-cell hyperplasia and hypertrophy,132 which might also be additionally influenced by a wide variety of growth factors and other nutrients.133 Increased numbers of β cells will also increase insulin production, as occurs in nondiabetic obesity and pregnancy.133
Insulin secretory-granule turnover should also be considered in the long-term regulation of insulin production and availability. An insulin secretory granule has an estimated half-life of 3 to 5 days,94 and if it does not undergo exocytosis, it is degraded intracellularly. Degradation of intracellular organelles like insulin secretory granules is mediated via autophagic mechanisms.134,135 Under normal circumstances, autophagy plays a janitorial role, removing aged secretory granules.136 However, under some circumstances where insulin secretion is compromised and proinsulin biosynthesis is not, then autophagy is up-regulated to prevent overaccumulation of intracellular insulin stores.94,136–138 It is thought that glucose also influences the autophagic degradation of intracellular insulin, but the mechanism is largely unknown94; recent studies suggest that LAMP2, ATG-7, and VMP1 may be involved.136,139,140
Insulin Secretion and Its Regulation
Insulin regulates glucose disposal in humans, maintaining blood glucose levels between approximately 3.8 and 6.1 mM in the fasting state; one definition of diabetes mellitus is a fasting blood sugar greater than 7 mM (see Chapter 39 in this volume). In normal, healthy individuals, the glucose level may rise to about 10 mM after a meal and decline to 3.3 mM during a prolonged fast. A sophisticated glucose-sensing and control mechanism controls insulin secretion, primarily linked to blood sugar concentrations but also dependent on numerous other factors, such as the incretins, GLP-1 and GIP, that all act to maintain blood sugar levels within these limits.
Similar to other neuroendocrine cells, insulin-secreting cells are electrically excitable.141 This means that insulin secretion in response to glucose is dependent on initiation of electrical activity from a basal electro-negative resting state. A summary of the many factors that regulate the secretory activity of the β cell is illustrated in Fig. 32-10. The importance of electrical control is most dramatically illustrated in the cases of neonatal diabetes caused by mutations in the two subunits of the ATP-dependent potassium channel (KATP), Kir6.2 and SUR1.142,143 In the normal course of glucose excitation coupling to insulin secretion, glucose enters the cell via GLUT2 (and GLUT1) glucose transporters and is trapped in the cell by phosphorylation via glucokinase, a specialized high-Km hexokinase. The high Km of glucokinase for glucose underlies its role as the “glucose sensor” of the β cell, in that its enzyme activity reflects physiologic circulating glucose concentrations. There is good evidence from studies of patients with loss-of-function mutations in glucokinase that this enzyme determines the insulin secretory response to changes in glucose concentration across the physiologic range.144 Following glucose phosphorylation, further metabolism via glycolysis, the Krebs (tricarboxylic acid [TCA]) cycle, and oxidative phosphorylation in the mitochondria leads to an increase in the ATP/ADP ratio in the cytoplasm.
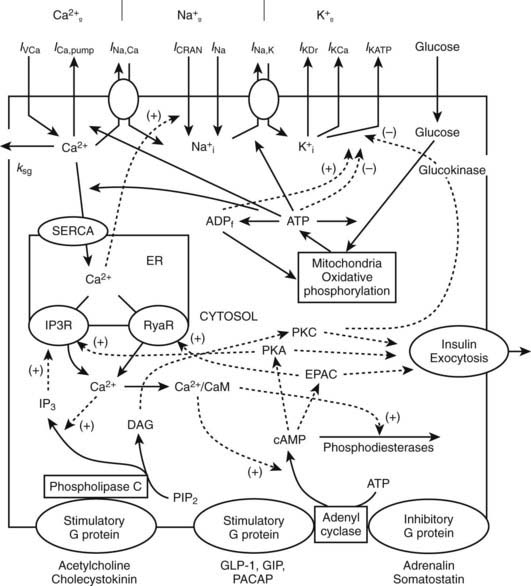
FIGURE 32-10 Interaction between membrane channels, ions, receptors, and selected mechanisms of cAMP and IP3 pathway regulation in insulin secretion. Top, plasma membrane currents: voltage-dependent Ca2+ current (IVCa), a calcium pump current (ICa,pump), Na+/Ca2+ exchange current (INa,Ca), Ca2+ release-activated nonselective cation current (ICRAN); inward Na+ currents (INa); a sodium-potassium pump current (INa,K), a delayed rectifying K+ current (IKDr), the small conductance Ca2+-activated K+ current (IKCa), ATP-sensitive K+ current (IKATP). Note that ksg is a coefficient of the sequestration rate of Ca2+ by the secretory granules, SERCA is the endoplasmic reticulum calcium pump, Ca2+ leaks out of the ER through IP3 receptor (IP3R) and ryanodine receptor (RyaR). Signals originating from fuel metabolism increase cytosolic calcium. Bottom, CaM, calmodulin, Ca2+/CaM is Ca2+-bound calmodulin. Synthesis and degradation of cAMP are catalyzed by adenylyl cyclase (AC) and phosphodiesterase (PDE), respectively. Epac is a guanine exchange protein activated by cAMP; PKA, protein kinase A; GLP-1 is glucagon-like peptide-1; PACAP is pituitary adenylate cyclase–activating polypeptide; GIP is glucose-dependent insulinotropic peptide. Synthesis of IP3 and diacylglycerol (DAG) from phosphatidylinositol-4,5-bisphosphate (PIP2) is catalyzed by phospholipase C (PLC). A variety of kinases activates exocytosis of insulin granules. Solid lines indicate fluxes, and dashed lines indicate inhibitory or stimulatory influences on currents or fluxes.
(Courtesy L. Fridlyand.)
While there are alternative hypotheses, it is the ATP/ADP ratio increase driven by metabolism that leads to KATP channel inhibition, in turn leading to accumulation of positive charge (K+ and Na+) inside the cell, causing the cell membrane to depolarize. As the membrane potential reaches about −20 mV from the resting level of about −70 mV, voltage-dependent calcium channels open, allowing entry of Ca2+. The rise in Ca2+ is soon opposed by opening of voltage-dependent and Ca2+-dependent K+ channels, contributing to the appearance of tonic or periodic transients of both membrane potential and Ca2+.145 The action potentials following glucose administration occur in grouped bursts of spikes on a depolarized plateau, with a variable quiet interval between bursts (Fig. 32-11). Some studies have shown that Ca2+ entry can lead to release of Ca2+ from intracellular (presumably endoplasmic reticulum) pools where it has been sequestered by the action of the sarcoplasmic/endoplasmic reticulum calcium ATPases (SERCA). Release of intracellular calcium through the action of inositol trisphosphate (IP3) on the IP3 receptors, as well as via ryanodine receptors and additional messengers, may all play complex roles in shaping intracellular Ca2+ transients. Mitochondria are also important stores of calcium and take up Ca2+ during metabolic activity, in part to regulate the key dehydrogenases in the TCA cycle. The elevation in intracellular free Ca2+ activates multiple proteins (e.g., small G proteins such as Rabs and soluble N-ethylmaleimide attachment protein receptor [SNARE] pathways) regulating the Ca2+-triggered fusion of the (predocked) insulin-containing granules with the cell membrane, resulting in the first phase of insulin secretion. As in neurotransmitter release, β-cell granule fusion depends on interactions of synaptosome-associated proteins, v-SNAREs (VAMP2 and synaptotagmin), with plasma membrane receptors such as SNAP-25, a t-SNARE (target localized SNAP receptor), and syntaxins. The importance of the depolarization step in insulin secretion is indicated by activating mutations in Kir6.2 and SUR1 that keep the KATP channel from closing in response to glucose metabolism, completely preventing physiologic insulin secretion and resulting in permanent neonatal diabetes.142,143 In contrast, loss-of-function mutations in these proteins that result in a persistently closed channel cause continued insulin release, leading to the condition known as hyperinsulinemia of infancy.146 Second-phase insulin secretion refers to the continued release of insulin following the initial peak. The kinetics of second-phase secretion at the β cell or islet level are variable and species specific. Granules are recruited via microtubules and associated kinases, chaperones, and small GTP-binding proteins (syntaxin4, Munc18) through the actin network until they too can dock with the plasma membrane at t-SNARE sites.147
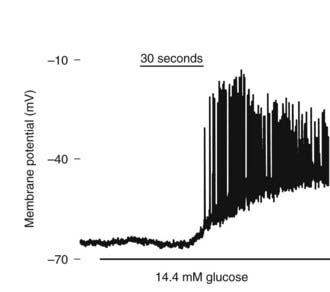
FIGURE 32-11 Effect of glucose on membrane potential in a mouse islet. The graph shows the onset of electrical bursting activity in a mouse islet, where the patch electrode was placed on one cell still connected to other islet cells.
(Courtesy D. Jacobson.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree