FIGURE 27-1. Components of eating behavior. Homeostatic hunger is hunger that results in eating in response to metabolic deficits and the ensuing signals. Hedonic and mood-related eating lead to consumption of calories above what is necessary to maintain energy balance.
Components of Energy Expenditure
Traditional models categorize energy expenditure (EE) into basal (obligate) and adaptive (or facultative) thermogenesis (AT). Obligate EE includes all pathways involved in the maintenance of basic metabolic and physiologic processes and is also referred to as resting metabolic rate (RMR) or more recently resting energy expenditure (REE). RMR includes both sleeping metabolic rate (SMR) and the increase in metabolic rate that is seen with arousal. AT includes cold and diet-induced thermogenesis. The cellular mechanisms that regulate obligatory and adaptive thermogenesis are often similar. Finally, physical activity represents a third category which has at least two components, nonexercise activity thermogenesis (NEAT) and sports-like exercise.21 These distinct categories of EE are in fact only approximate, and regulatory mechanisms are overlapping (Fig. 27-2). For example, thyroid hormone (TH) is required for up to 30% of basal EE, and adaptive increases in TH are required for normal cold-induced thermogenesis.22,23 Furthermore, physical activity (PA) can have long-lasting effects on REE, and PA may be enacted by stimuli that are traditionally considered stimulants of facultative thermogenesis, such as caloric excess.24 Approximate contributions for the components of energy expenditure are REE, 70%; PA, 20%; and facultative, 10%, with PA representing the most variable component.25
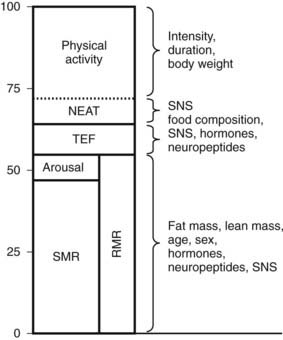
FIGURE 27-2. Approximate contribution of components of energy expenditure. Thermic effect of food (TEF) and resting metabolic rate (RMR) can be measured using a ventilatory hood. RMR and nonexercise activity thermogenesis (NEAT) can be measured in a respiratory chamber. Total energy expenditure can be measured using doubly labeled water. SMR, Sleeping metabolic rate.
Integration of Energy Balance
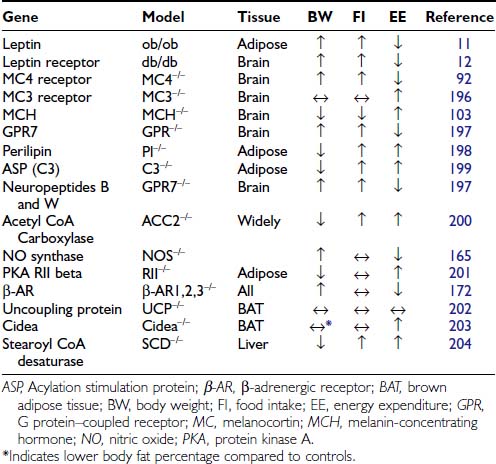
Inputs from a number of neuropeptides and neurotransmitters in the brain as well as peripheral signals integrate information to mediate energy balance.26 The interactions and pathways engaged by these signals are already complex, and understanding of the pathways is still evolving. Furthermore, it is not clear that all possible important signals have been identified. One interesting aspect of the signals involved is that many regulate both energy intake and energy expenditure in a coordinated fashion. Although a correlation of obesity with decreased sympathetic activity has been long recognized,27,28 the potential pathways regulating energy expenditure were thought to be separate from those regulating feeding and satiety. However, it is now recognized that peptides regulating appetite also play a role in regulating energy expenditure in an inverse manner. Thus, peptides that stimulate feeding decrease energy expenditure, promoting energy storage, while those that inhibit feeding increase energy expenditure (Table 27-1).
In the brain, both neurotransmitters and neuropeptides have complex functions.29 The role of neurotransmitters in regulating feeding behavior was recognized before the role of neuropeptides was appreciated. However, mechanisms of these neurotransmitters have been more difficult to define; they may act through multiple receptors, and effects may vary depending on the anatomic area targeted. Monoamine neurotransmitters may be stimulatory or inhibitory. Glutamate and γ-aminobutyric acid (GABA), which are the most abundant neurotransmitters in the hypothalamus, act to increase feeding, and some of the neurons expressing orexigenic neuropeptides appear to be GABAergic.30 One view of the interaction of transmitters and peptides is that peptides act as essential modulators of GABA and glutamate action.31 Serotonin, which acts through multiple receptors, is inhibitory,32 and some of these receptors are being considered as specific pharmacologic targets for the treatment of obesity.33 The roles of epinephrine, norepinephrine, and dopamine are more complex, and these transmitters may act to either stimulate or inhibit feeding.34,35 Although the mechanism of action is poorly understood, these pathways are the targets of the limited pharmacologic therapies that are currently available for the treatment of obesity. Biogenic amines currently in use include phentermine and sibutramine. Phentermine, an analog of amphetamine, acts to increase catecholamine release in the paraventricular nucleus of the hypothalamus. Mazindol has a similar mechanism of action. Sibutramine, which acts through its active metabolites, prevents reuptake of 5-HT but does not cause release. Sibutramine also inhibits noradrenaline reuptake.36
The number of hypothalamic neuropeptides known to be involved in body weight regulation has expanded dramatically over the past decade. Peptides that act as orexigenic signals include neuropeptide Y (NPY), agouti-related peptide (AgRP), melanin-concentrating hormone (MCH), galanin, β-endorphin, dynorphin and enkephalin, and the orexins. Peptides that act to inhibit feeding include α-melanocyte-stimulating hormone (α-MSH), cocaine-amphetamine-regulated transcript (CART), corticotropin-releasing hormone, urocortin, neurotensin, and neuromedin. The specific role of neuropeptides has been easier to identify, in part because expression of these peptides tends to be anatomically limited. Additionally, genetic studies are both easier and more readily interpretable, since ablation is not usually associated with lethality.
Recently, the importance of interaction of peptidergic systems with neurotransmitters has been recognized as playing a role. For example, leptin37,38 and MCH39,40 appear to regulate dopaminergic tone. In the arcuate, GABAergic AgRP/NPY neurons play a critical role in regulating pro-opiomelanocortin (POMC) neurons. Although ablation of AgRP or NPY individually or both peptides in combination does not result in an identifiable phenotype,41 ablation of the neurons in adult mice leads to rapid starvation.42 Consistent with the role of GABA regulating POMC neurons, mice with impaired GABA release are lean and resistant to diet-induced obesity.43
In addition to leptin, other signals from the periphery add to the complex pathways that are involved in the regulation of body weight. This includes multiple signals from the gut44,45 (Fig. 27-3). Cholecystokinin (CCK) is synthesized in the duodenum and jejunum and was recognized as a peptide capable of inhibiting appetite as early as 1973.46 CCK acts in the hindbrain to reduce meal size and duration.47 Peptide YY (PYY) is secreted by the distal portion of the gastrointestinal tract, and in addition to inhibiting gastric emptying,48 it also crosses the blood-brain barrier to act on arcuate nuclei and inhibit feeding.44 However, the role of PYY remains controversial, because when injected into the lateral ventricles of animals, PYY acts to increase food intake, and not all investigators have been able to reproduce the satiety effects.49 Glucagon-like peptide 1 (GLP-1) and oxyntomodulin are products of the preproglucagon gene and are synthesized in the gut and brain. Both act to inhibit food intake through different mechanisms.50 Thus far, the only gut peptide known to stimulate appetite is ghrelin, which is secreted by the stomach and also acts on neurons in the arcuate nucleus.51
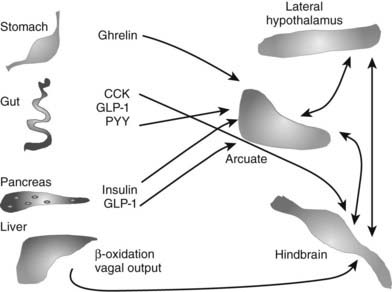
FIGURE 27-3. Schema of selected gut-to-brain signals that may play a role in mediating energy balance. A number of peptides from the gut play a role in mediating appetite and energy expenditure. Only one, ghrelin from the stomach, is orexigenic. All segments of the gut may also contribute to signals from vagal afferents. Finally, information of oxidation of fatty acids in the liver may also be transmitted by the vagus and play a role in mediating appetite. Within the brain, signaling acquires additional complexity; networks between the hypothalamus and hindbrain and cortex are all involved in regulating both intake and output.
Other factors derived from the gut that may play a role in appetite include fatty acid amides. For example, the cannabinoid receptor agonist, anandamide, is an ethanolamide synthesized in the gut and possibly regulated by nutritional status, since local concentrations increase with fasting.52 Anandamide may act centrally through cannabinoid receptors, which are known to promote appetite and increase energy homeostasis.53 In contrast oleoylethanolamide, which is also synthesized in the gut, acts to inhibit food intake and stimulate lipolysis through the activation of the peroxisome proliferator–activated receptor alpha (PPAR-α).54 Thus fatty acid–derived molecules may serve as an additional pathway of gut-mediated regulation of appetite.
Peripheral signals regarding the state of the gastrointestinal tract may also be integrated by the vagus nerve,55 which sends afferents to multiple brain areas, including the dorsal motor nucleus and the nucleus of the solitary tract. These areas appear to be involved in responses to neuropeptides, including ghrelin56 and α-MSH. The vagus may also play a role in conveying information on fatty acid oxidation in the liver. Fatty acid oxidation appears to play a role in mediating appetite; inhibition of this process is associated with increased appetite.57,58
Insulin may also play a role in inhibiting appetite, and it is known that neurons in the arcuate express insulin receptors59 and respond to insulin. Female mice lacking insulin receptor expression in the brain eat more than normal animals, and both genders develop mild obesity when placed on a high-fat diet.60 Insulin and glucose may play a role in meal initiation and meal termination.61
Thus, body weight is regulated by a complex interaction of signals involving both the gut and the brain. Additional complexity derives from the fact that these signals act through specific receptors. The receptors have anatomic-specific expression. Furthermore, some involve relatively large receptor families, as seen with the melanocortin receptors (see The Melanocortin System: α-MSH, Agouti-Related Peptide, and Central Melanocortin Receptors). For some of these pathways, the finding of spontaneous mutations associated with obesity in human populations has provided proof that body weight is regulated similarly in humans as in rodents (Table 27-2).
Table 27-2. Sample of Characterized Mutations Leading to Obesity in Humans
| Mutation | Reference |
|---|---|
| Leptin | 62, 13 |
| Leptin receptor | 14 |
| Melanocortin 4 receptor | 94, 95, 205 |
| Melanocortin 3 receptor | 206 |
| Prohormone convertase 1 | 207 |
| PPAR-γ | 208 |
| POMC | 96 |
POMC, Pro-opiomelanocortin; PPAR, peroxisome proliferator–activated receptor.
Specific Hormones and Neuropeptides
ADIPOSE TISSUE DERIVED
Leptin, identified through positional cloning of the ob gene,11 is a 167-amino-acid peptide hormone secreted by adipocytes. It signals through a membrane receptor that has six splice variants and belongs to the class I cytokine receptor family.12 Leptin signaling is required, although not sufficient alone, for normal energy balance. Animals, including mice and humans, lacking leptin62 or the leptin receptor14 have a syndrome of severe hyperphagia and obesity. In the case of leptin mutations, leptin administration leads to a marked resolution of the syndrome in both ob/ob mice63,64 and in rare human patients with leptin mutations.65,66 However, in the vast majority of obese mammals, leptin levels are elevated, correlating well with available fat stores,67,68 and administration of peripheral leptin has little effect on appetite. These findings revised the perception of leptin. While the complete absence of leptin has major consequences on appetite, the incremental increases in leptin that are seen with increased adiposity have little effect on the continued ingestion of calories or the storage of calories as fat. In contrast, repletion of leptin with fasting leads to attenuation of many of the neuroendocrine changes seen with fasting.69 In human females, leptin replacement leads to some of the abnormalities seen in hypothalamic amenorrhea secondary to strenuous exercise or low body weight.70 Thus the critical physiologic role of leptin appears to be to signal caloric deficiency and thus mediate the appropriate metabolic changes rather than to signal caloric excess.
Leptin targets specific neurons in the brain, specifically in the hypothalamus, although leptin receptors are also seen in other areas, including the ventral tegmental area (VTA). The best-characterized neurons are the NPY/AgRP and POMC neurons in the arcuate.30,71 NPY and AgRP are both orexigenic (appetite-inducing) peptides synthesized by the same population of neurons. POMC is expressed in a different population of arcuate neurons that process the preprohormone to a number of peptides, including α-MSH, which acts to suppress appetite. To date, the leptin-to-arcuate pathway represents the best-characterized pathway involved in the regulation of body weight, especially insofar as mutations disrupting this pathway have also been shown to be important in human obesity as well as rodent obesity (Fig. 27-4).
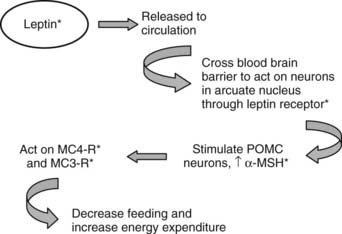
FIGURE 27-4. The leptin pathway. Leptin, a hormone secreted by adipocytes, crosses the blood-brain barrier to act on neurons in the arcuate nucleus. One set of target neurons are those synthesizing prepro-opiomelanocortin (POMC). Leptin acts to stimulate these neurons to synthesize POMC and release one of the POMC gene products, α-melanocyte-stimulating hormone (α-MSH). This peptide mainly acts through the melanocortin 4 receptor (MC4R) to decrease feeding, and through this receptor and the melanocortin 3 receptor (MC3R) to increase energy expenditure. Mutations in this pathway lead to disruption of the appropriate signals and to obesity. Known mutations leading to obesity in humans are marked with asterisks. (See text and Table 27-2 for details.)
Adipocytes synthesize many biologically active proteins with potential endocrine function (reviewed in Ref. 58 and Chapter 37). These include cytokines, immune-related proteins, complement and complement-related proteins, enzymes involved in steroid metabolism, and proteins of the rennin-angiotensin system. Furthermore, receptors for traditional endocrine hormones, nuclear hormones, cytokines, and catecholamines are all expressed by adipose tissue. These peptides are likely to form causal links between obesity, insulin resistance, and cardiovascular disease. Two recently discovered peptides, adiponectin and resistin, may play a role in modulating insulin resistance. Adiponectin inversely correlates with insulin resistance, declines with obesity, and increases with weight loss.72 In contrast, resistin impairs glucose tolerance and insulin sensitivity, and secretion increases with increasing adiposity.73 They may also be involved in determining predisposition to obesity and responses to a high-fat diet. Recently, excess adiposity has been associated with finding increased expression of multiple inflammatory markers in fat tissue. Thus, expression of interleukin 1 (IL-1), IL-5, plasminogen activator inhibitor 1 (PAI-1), tumor necrosis factor (TNF), and suppressor of cytokine signaling 3 (SOCS3) are all increased in obesity.74 These factors play a role in the decrease in insulin sensitivity associated with obesity; however, it is unclear (and seems unlikely) that any of these factors have direct effects on either appetite or energy expenditure.
THE HYPOTHALAMUS
Neuropeptide Y
The potential role of neuropeptides in feeding behavior was first suggested by studies indicating that NPY was synthesized by arcuate75 neurons and elicited a robust feeding response when injected intracerebroventricularly (ICV).76,77 Chronic infusion of NPY leads to obesity in rats.78,79 Furthermore, expression of NPY increases with fasting, indicating that neurons making NPY respond to peripheral signals, signaling the state of energy balance.80,81 Interestingly, ablation of the NPY gene was not associated with altered body weight or feeding,82 although when mice lacking NPY were bred to mice lacking leptin, substantial attenuation of the ob/ob obesity syndrome was noted.83 However, animals without NPY show an abnormal response to refeeding after short-term fasting84 and also show an attenuated feeding response to hypoglycemia.85
The Melanocortin System: α-MSH, Agouti-Related Peptide, and Central Melanocortin Receptors
Humans and rodents require an intact melanocortin system in order to maintain normal body weight. The effect of α-MSH to decrease appetite was described in the late 1980s.86 However, the key role of melanocortins in the physiology of energy balance was not appreciated until the molecular mechanism of obesity of the yellow Ay mouse was identified. In this model, obesity is secondary to a mutation in the gene encoding a protein, agouti, which mediates coat color and leads to ectopic expression of the protein in all tissues, including the central nervous system.87 Subsequently it was discovered that agouti protein acted on melanocortin receptors to block melanocyte-stimulating hormone (MSH) action.88,89 These findings led to speculation that another protein normally expressed in the brain might have an action similar to that of agouti and to the discovery of agouti-related peptide, AgRP,90 which is expressed in the hypothalamus and interacts with the central melanocortin receptors, MC3R and MC4R.91 Overexpression of AgRP recapitulated an obesity syndrome similar to that seen in the Ay mouse, as did disruption of the MC4R.92 Mice with targeted disruption of the MC3R demonstrated a small increase in body fat and feeding efficiency, suggesting that at least in rodents, MC4 plays the dominant role in energy homeostasis.
The profound effects caused by disruption of the melanocortin pathway stimulated a search of MC4R mutations in humans, especially in children with early-onset obesity and a strong family history of obesity. Several such mutations were readily identified,93,94 and currently it is estimated that 5% of persons with severe familial early-onset obesity have MC4 mutations.95 In humans, obesity has also been associated with mutations in the POMC gene, which encodes multiple transcripts. Disruption of this gene leads to deficiency in both adrenocorticotropic hormone (ACTH) and MSH, and patients present with adrenal insufficiency and obesity. Since MSH expression outside of the central nervous system mediates hair color, patients with POMC mutations will frequently also have red hair.96
Melanin-Concentrating Hormone
Melanin-concentrating hormone is a 19-amino-acid peptide synthesized in magnocellular neurons of the lateral hypothalamus; it plays a key role in maintaining energy balance in animals.97,98 The peptide structure and anatomic distribution is highly conserved, and the sequence is identical in rodents, sheep, and humans. When injected ICV in rats, MCH induces an acute increase in feeding behavior. Chronic infusions in mice lead to a syndrome of mild obesity associated with decreased energy expenditure.99 Deletion of both the MCH and the MCH receptor genes are associated with leanness.100–102 In the case of the receptor knockouts, leanness is secondary to increased expenditure, because animals without the receptor eat as much or more than wild-type animals. Deletion of MCH from mice lacking leptin leads to a marked attenuation of the obesity phenotype, which is secondary to changes in energy expenditure rather than feeding.103 Pharmacologic blockade of the MCH receptor leads to leanness and reduces meal size.104 Chronic infusions of MCH agonists also lead to obesity similar to that seen with MCH infusion.105 The importance of the MCH system has not been validated in humans, since a phenotype of MCH deficiency would present with a lean phenotype. However, the homology of MCH in all strains of mammals examined strongly suggests that MCH will play a role in humans.
THE GUT
Ghrelin
Ghrelin, produced in the stomach, was identified as the endogenous ligand for the receptor responsible for growth hormone secretion.106 Subsequently it was found to produce adiposity in rodents, an effect that is independent of its ability to stimulate growth hormone secretion.107 Although infusions of ghrelin induce hunger and increased feeding,108 endogenous levels are low in obese individuals and increase with weight loss.109 This rise is not seen after gastric bypass surgery, which may help to explain the success of this procedure in mediating weight loss in obese humans.110,111 Ghrelin levels are extremely high in the Prader-Willi syndrome of genetic obesity.112 Ghrelin is transported into the brain, where it acts to stimulate NPY/AgRP neurons in the arcuate nucleus and is thus part of a circuit mediating energy homeostasis involving the stomach and the hypothalamus.113
Peptide YY
Peptide YY is synthesized and secreted throughout the intestine, although concentrations are higher in the distal portion, particularly in the colon and rectum, and the 3-36 form crosses the blood-brain barrier. Food intake stimulates PYY release, and higher serum concentrations are seen after fatty meals. As release occurs prior to nutrients reaching the distal parts of the gastrointestinal tract, neural reflexes may act to stimulate release, possibly through the vagus. PYY 1-36 has structural similarity to NPY and binds with high affinity to all five NPY receptors; the 3-36 form binds preferentially to the Y2 receptor. PYY acts on both the intestine and the brain. In the intestine, it increases fluid absorption and delays gastric emptying. In the brain, the 3-36 form has substantial effects on appetite. When given intravenously to human volunteers, it reduces caloric intake and increases the sensation of satiety.114 Similar effects have been reported in rats115; however, this effect is controversial because other investigators have been unable to reproduce the satiating effect.49 ICV injection of PYY clearly increases feeding, presumably through targeting a different receptor subset.116
PYY levels are low in patients with morbid obesity. One report suggests that levels rise after weight loss secondary to gastric bypass surgery.117 This suggests a potential role of PYY in the treatment of obesity.
Glucagon-Like Peptide-1 and Oxyntomodulin
GLP-1 and oxyntomodulin, along with GLP-2, are products of the preproglucagon gene and result from posttranslational processing by prohormone convertases. The preproglucagon gene is expressed in the central nervous system, in intestinal L cells, and in the pancreas. Both GLP-1 and oxyntomodulin act as satiety signals through the GLP-1 receptor.50,118,119 Release from the small intestine is seen after food ingestion; however, the peptides are rapidly cleaved by dipeptidyl peptidase IV and thus have a short half-life. GLP-2 does not affect satiety.120 GLP-1 has effects on insulin secretion and beta cell mass, while GLP-2 affects the growth of intestinal epithelial cells.121 GLP-1 has therapeutic potential in the treatment of obesity and type 2 diabetes, although this could be limited because of the short half-life. One approach aimed at circumventing this problem is the use of peptidase inhibitors and long-acting analogs such as exenatide.122
The Role of Energy Expenditure in Body Weight Regulation
MEASURING ENERGY EXPENDITURE
Measuring ingested food is straightforward, at least in experimental animals. However, measuring energy expenditure is complicated because one must account for all components as well as the relative contribution of each component. The most accurate method for determination of EE is by direct calorimetry, which can be measured either by water immersion or closed-chamber heat convection, but both of these methods are cumbersome and are rarely used. Ingestion of doubly labeled water allows interpolation of EE from the amount of 2H218O ingested, and the amount of 2H and 18O released as water and carbon dioxide has been shown to be accurate to within 5% of indirect calorimetry.123 However, these techniques require use of both expensive non-radioactive isotopes and instrumentation. Since more than 90% of oxygen consumption arises from mitochondrial metabolism,124 O2 consumption can be used as an index of energy expenditure. For rodent studies, indirect calorimeters consist of closed multichambered modules with oxygen and CO2 sensors that measure gas exchange. Most are also equipped with laser beam break systems that allow simultaneous monitoring of spontaneous locomotor activity. Models with continuous access to food and water are available, and these can be used to monitor animals over intervals as long as days or weeks. Software is supplied to calculate VO2, VCO2, and RER, as well as total heat production based on VO2. In humans, respirometers such as the Deltatrac or Cosmed are most commonly used. A significant limitation of these monitors is that observation requires wearing space helmet–like head gear which results in a limited observation period. Some clinical research facilities have closed room-sized chambers which measure gas exchange using methodology similar to that used by rodent monitors.
Comparing Energy Expenditure Between Individual Subjects
Using indirect calorimetry to compare EE among organisms that differ in body weight has inherent inaccuracies. Differences in body weight are usually associated with differences in tissue distribution; for example, animals that are obese will have similar lean body mass but have increased adipose tissue. Energy expenditure of different tissues varies over a broad range,125 and it is not possible to calculate the contribution of each organ. While fat has a relatively low EE, in obese animals, it may represent a relatively high proportion of total mass. Many investigators normalize VO2 for body weight or, preferably, lean body mass that more closely reflects total EE.126 However, there is no clear-cut agreement about how EE is best expressed. To control for this confounder, some perform pair feeding experiments. When two groups of animals are fed the same amount of food, and one group loses more weight, the group experiencing the greater weight loss either had greater EE or lower energy absorption in the intestine. If digestive loses are accounted for, one can conclude that the group that lost more weight had higher EE. An example of pair feeding (PF) is shown in Fig. 27-5.127 The PF paradigm also has flaws, possibly owing to a relative state of semistarvation that is perceived by PF animals. For example, compared to leptin-treated rats that have decreased food intake, PF rats are relatively hypothyroid due to decreased hepatic conversion of T4 to T3.128
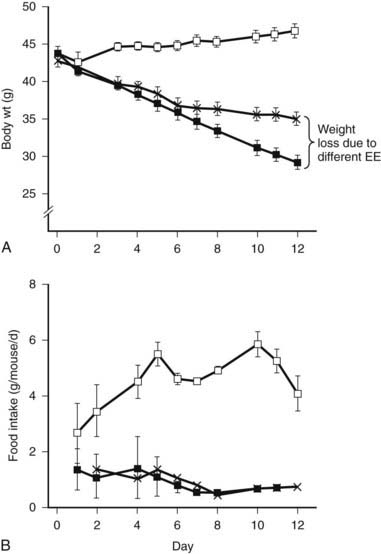
FIGURE 27-5. Pair feeding in ob/ob mice results in less weight loss, implying increased energy expenditure (EE) from leptin treatment. Leptin-deficient ob/ob mice are hyperphagic (control open squares) and respond to leptin treatment by reducing food intake and increasing EE. The increased body weight loss in the ob/ob leptin-treated group (closed squares) compared to the pair-fed group is due to increased EE.
(From Levin N, Nelson C, Gurney A et al: Decreased food intake does not completely account for adiposity reduction after ob protein infusion, Proc Natl Acad Sci U S A 93:1726–1730, 1996.)
To demonstrate changes in EE between subjects, either EE needs to be measured directly or weight and body composition need to be taken into account. In addition, careful PF experiments should be performed and correlated to findings seen with indirect calorimetry.
HOW DOES ENERGY EXPENDITURE CONTRIBUTE TO OBESITY?
Small discrepancies between energy intake and EE over a long time can result in net positive energy balance and obesity. For example, assuming constant energy expenditure, the current epidemic of obesity could theoretically be stabilized by lowering food intake by 100 kcal per day according to one estimate.129 By analogy, if food intake is constant, a small increase of activity leading to an increased expenditure of 100 calories would have the same effect. Increasing energy expenditure is known to be an important contributor to resistance to diet-induced obesity in rodents and appears to be strain specific, even in mice eating the same diet and total calories. When an obesity-susceptible strain is placed on a high-fat diet, there is a very small increase in oxygen consumption. In contrast, the obesity-resistance strain shows a substantial increase in oxygen consumption both secondary to increased RMR and increased spontaneous locomotor activity.130
In humans it is extremely difficult to assess the role of EE. On an absolute basis, obese patients have increased EE. Thus, only relative differences in EE might account for predisposition to obesity. Evidence exists both to support and refute an important role for abnormal EE in human obesity.
The role of EE in the pathogenesis of obesity remains unresolved. A number of studies support the hypothesis that reduced EE plays a pathogenic role in the development of obesity. Early studies, based on the comparison of self-reported food diaries to weight gain, suggested that obese patients have significantly lower EE compared to lean patients. However, these differences could not be confirmed in studies using the doubly labeled water technique,123,131 and differences were attributed to underreporting of food consumption. Nonetheless, there is compelling evidence that lower EE and predisposition to obesity is genetically determined. Obesity itself has a strong genetic component,132 and resting metabolic rate also appears to be an inherited trait, and is independent of fat-free mass, age, and sex as a predictor of EE.133 Overfeeding studies in monozygotic twins show a high degree of similarity in weight gain between but not among twins and also argue strongly that genetic factors play a major role in controlling EE.134 Also, the environment in which identical twins are raised has little influence over eventual body mass index (BMI).135 Finally, direct and indirect measurements of EE and respiratory quotient (RQ) have shown small but measurable differences between obese and lean patients, particularly in certain ethnic groups such as Pima Indians.136,137 Longitudinal studies have confirmed that differences in EE are associated with tendency to develop obesity over a period of years.138
In contrast, other studies failed to find significant differences in EE between obese and lean human patients. For example, EE increases linearly with increasing BMI, so increased EE at higher body weight would function to resist further body weight change.25 Similarly, children aged 5 to 10 with varying known susceptibility to obesity have similar increases in RMR.139 Furthermore, no differential activity between lean and obese individuals in systems regulating body weight has been reported; this includes sympathetic nervous system (SNS) activity,140 catecholamine turnover,141 lipolysis,142 the thermic effect of food,25 and thyroid hormones.143 In summary, some studies have reported data to support the hypothesis that relatively low EE contributes to the development of obesity. These findings, in addition to clear defects in EE that are seen in obese rodent models, suggest that defects in EE may be attractive targets for antiobesity treatments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree