FIGURE 95-1. The dramatic case of Maria Richsel, the first patient with postoperative myxedema to have come to Kocher’s attention. A, The child and her younger sister before the operation. B, Changes 9 years after the operation. The younger sister, now fully grown, contrasts vividly with the dwarfed and stunted patient. Also note Maria’s thickened face and fingers, which are typical of myxedema.
(From Kocher T: Uber Kropfextirpation und ihre Folgen, Arch Klin Chir 29:254, 1883.)
By 1920, advances in thyroid surgery had reached the point that Halsted referred to this operation as a “feat which today can be accomplished by any competent operator without danger of mishap.”1 Unfortunately, decades later, complications still occur. In the best of hands, however, thyroid surgery can be performed today with a mortality that varies little from the risk of general anesthesia alone, as well as with low morbidity. To obtain such enviable results, however, surgeons must have a thorough understanding of the pathophysiology of thyroid disorders; must be versed in the preoperative and postoperative care of patients; must have a clear knowledge of the anatomy of the neck region; and, finally, must use an unhurried, careful, and meticulous operative technique.
Important Surgical Anatomy
The thyroid (which means “shield”) gland is composed of two lobes connected by an isthmus that lies on the trachea approximately at the level of the second tracheal ring (Fig. 95-2). The gland is enveloped by the deep cervical fascia and is attached firmly to the trachea by the ligament of Berry. Each lobe resides in a bed between the trachea and larynx medially and the carotid sheath and sternocleidomastoid muscles laterally. The strap muscles are anterior to the thyroid lobes, and the parathyroid glands and recurrent laryngeal nerves are associated with the posterior surface of each lobe. A pyramidal lobe is often present. This structure is a long, narrow projection of thyroid tissue that extends upward from the isthmus and lies on the surface of the thyroid cartilage. It represents a vestige of the embryonic thyroglossal duct, and it often becomes palpable in cases of thyroiditis or Graves’ disease. The normal thyroid varies in size in different parts of the world, depending on the iodine content in the diet. In the United States, it weighs about 15 g.
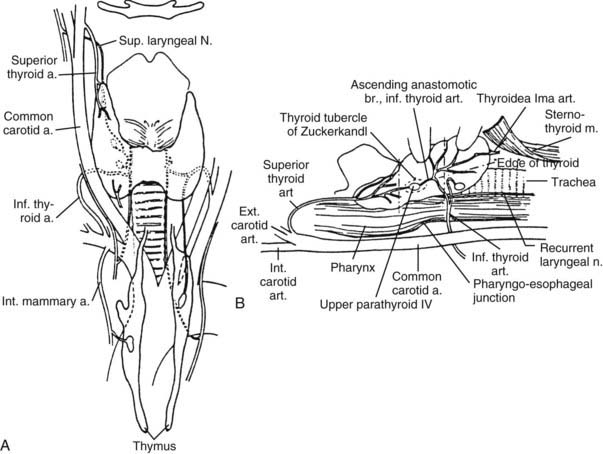
FIGURE 95-2. Anatomy of the thyroid and parathyroid glands. A, Anterior view. B, Lateral view with the thyroid retracted anteriorly and medially to show the surgical landmarks (the head of the patient is to the left).
(From Kaplan EL: Thyroid and parathyroid. In Schwartz SI [ed]: Principles of Surgery, 5th ed. New York, McGraw-Hill, 1989, pp 1613–1685. Copyright © by McGraw-Hill, Inc. Used by permission of McGraw-Hill Book Company.)
VASCULAR SUPPLY
The thyroid has an abundant blood supply (see Fig. 95-2). The arterial supply to each thyroid lobe is twofold. The superior thyroid artery arises from the external carotid artery on each side and descends several centimeters in the neck to reach the upper pole of each thyroid lobe, where it branches. The inferior thyroid artery, each of which arises from the thyrocervical trunk of the subclavian artery, crosses beneath the carotid sheath and enters the lower or midpart of each thyroid lobe. The thyroidea ima is sometimes present; it arises from the arch of the aorta and enters the thyroid at the midline. A venous plexus forms under the thyroid capsule. Each lobe is drained by the superior thyroid vein at the upper pole, which flows into the internal jugular vein; and by the middle thyroid vein at the middle part of the lobe, which enters the internal jugular or the innominate vein. Arising from each lower pole is the inferior thyroid vein, which drains directly into the innominate vein.
NERVES
The thyroid gland’s relationship to the recurrent laryngeal nerve and to the external branch of the superior laryngeal nerve is of major surgical significance because damage to these nerves leads to disability in phonation or to difficulty in breathing.4 Both nerves are branches of the vagus nerve.
Recurrent Laryngeal Nerve
The right recurrent laryngeal nerve arises from the vagus nerve, loops posteriorly around the subclavian artery, and ascends behind the right lobe of the thyroid (Fig. 95-3). It enters the larynx behind the cricothyroid muscle and the inferior cornu of the thyroid cartilage and innervates all the intrinsic laryngeal muscles except the cricothyroid. The left recurrent laryngeal nerve comes from the left vagus nerve, loops posteriorly around the arch of the aorta, and ascends in the tracheoesophageal groove posterior to the left lobe of the thyroid, where it enters the larynx and innervates the musculature in a similar fashion as the right nerve. Several factors make the recurrent laryngeal nerve vulnerable to injury, especially in the hands of inexperienced surgeons4,6

FIGURE 95-3. Anatomy of the recurrent laryngeal nerves.
(From Thompson NW, Demers M: Exposure is not necessary to avoid the recurrent laryngeal nerve during thyroid operations. In Simmons RL, Udekwu AO [eds]: Debates in Clinical Surgery, Chicago, Year Book, 1990.)
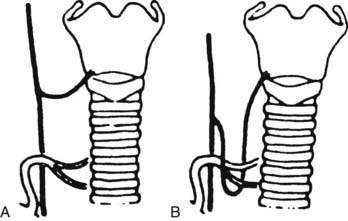
FIGURE 95-4. “Nonrecurrent” right laryngeal nerves coursing (A) near the superior pole vessels or (B) around the inferior thyroid artery. Because of the abnormal location of “nonrecurrent” nerves, they are much more likely to be damaged during surgery.
(From Skandalakis JE, Droulis C, Harlaftis N, et al: The recurrent laryngeal nerve, Am Surg 42:629–634, 1976.)
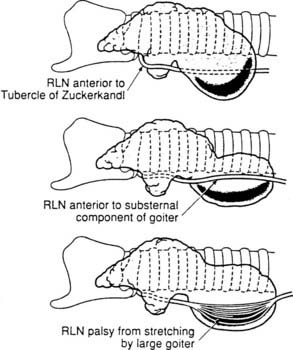
FIGURE 95-5. Recurrent laryngeal nerve displacement by cervical and substernal goiters. Such nerves are at risk during lobectomy unless the surgeon anticipates the unusual locations and is very careful. Rarely, the nerves are so stretched that spontaneous palsy results. After careful dissection and preservation, functional recovery may occur postoperatively.
(From Thompson NW, Demers M: Exposure is not necessary to avoid the recurrent laryngeal nerve during thyroid operations. In Simmons RL, Udekwu AO [eds]: Debates in Clinical Surgery. Chicago, Year Book, 1990.)
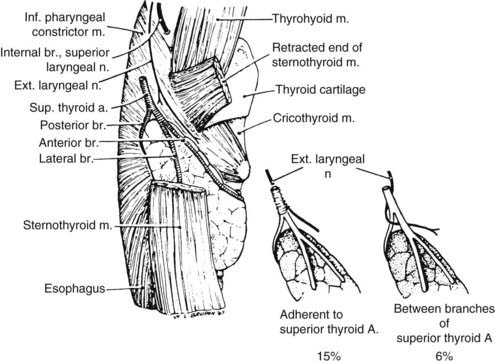
External Branch of the Superior Laryngeal Nerve
On each side, the external branch of the superior laryngeal nerve innervates the cricothyroid muscle. In most cases, this nerve lies close to the vascular pedicle of the superior poles of the thyroid lobe,7 which requires that the vessels be ligated with care to avoid injury to it (Fig. 95-6). In 21%, the nerve is intimately associated with the superior thyroid vessels. In some patients, the external branch of the superior laryngeal nerve lies on the anterior surface of the thyroid lobe, making the possibility of damage during thyroidectomy even greater.8 In only 15% of patients is the superior laryngeal nerve sufficiently distant from the superior pole vessels to be protected from manipulation by the surgeon. Unfortunately, many surgeons do not even attempt to identify this nerve before performing ligation of the upper pole of the thyroid.9,9a
PARATHYROID GLANDS
The parathyroids are small glands that secrete parathyroid hormone, the major hormone that controls serum calcium homeostasis in humans. Usually, four glands are present, two on each side, but three to six glands have been found. Each gland normally weighs 30 to 40 mg, but glands may be heavier if more fat is present. Because of their small size, their delicate blood supply, and their usual anatomic position adjacent to the thyroid gland, these structures are at risk of being accidentally removed, traumatized, or devascularized during thyroidectomy.10
The upper parathyroid glands arise embryologically from the fourth pharyngeal pouch (Figs. 95-7 and 95-8). They descend only slightly during embryologic development, and their position in adult life remains constant. This gland is usually found adjacent to the posterior surface of the middle part of the thyroid lobe, often just anterior to the recurrent laryngeal nerve as it enters the larynx.
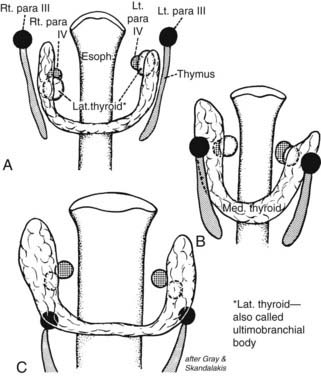
FIGURE 95-7. A and B, Shifts in location of the thyroid, parafollicular, and parathyroid tissues. C approximates the adult location. Note that what has been called the lateral thyroid is now commonly referred to as the ultimobranchial body, which contains both C cells and follicular elements.
(From Sedgwick CE, Cady B: Surgery of the Thyroid and Parathyroid Gland, 2nd ed. Philadelphia, WB Saunders, 1980; adapted from Norris EH: Parathyroid glands and lateral thyroid in man: their morphogenesis, histogenesis, topographic anatomy and prenatal growth, Contrib Embryol Carnegie Inst Wash 26:247–294, 1937.)
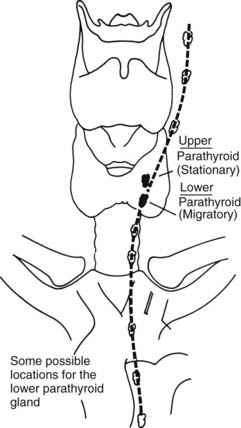
FIGURE 95-8. Descent of the lower parathyroid. Whereas the upper parathyroid occupies a relatively constant position in relation to the middle or upper third of the lateral thyroid lobe, the lower parathyroid normally migrates in embryonic life and may end up anywhere along the course of the dotted line. When this gland is in the chest, it is nearly always in the anterior mediastinum.
(From Kaplan EL: Thyroid and parathyroid. In Schwartz SI [ed]: Principles of Surgery, 5th ed. New York, McGraw-Hill, 1989, pp 1613–1685. Copyright © by McGraw-Hill, Inc. Used by permission of McGraw-Hill Book Company.)
The lower parathyroid glands arise from the third pharyngeal pouch, along with the thymus; hence, they often descend with the thymus. Because they travel so far in embryologic life, they have a wide range of distribution in adults, from just beneath the mandible to the anterior mediastinum11 (see Fig. 95-8). Usually, however, these glands are found on the lateral or posterior surface of the lower part of the thyroid gland or within several centimeters of the lower thyroid pole within the thymic tongue.
Parathyroid glands can be recognized by their tan appearance; their small vascular pedicle; the fact that they bleed freely when a biopsy is performed, as opposed to fatty tissue; and their darkening color of hematoma formation when they are traumatized. With experience, one becomes much more adept at recognizing these very important structures and in differentiating them from lymph nodes or fat. Frozen section examination during surgery can be helpful in their identification.
LYMPHATICS
A practical description of the lymphatic drainage of the thyroid gland for the thyroid surgeon has been proposed by Taylor.12 The results of his studies, which are clinically very relevant to the lymphatic spread of thyroid carcinoma, are summarized in the following section.
Central Compartment of the Neck
Lateral Compartment of the Neck
A constant group of nodes lies along the jugular vein on each side of the neck. The lymph glands found in the supraclavicular fossae may also be involved in more distant spread of malignant disease from the thyroid gland. Finally, it should not be forgotten that the thoracic duct on the left side of the neck, a lymph vessel of considerable size, arches up out of the mediastinum and passes forward and laterally to drain into the left subclavian vein, usually just lateral to its junction with the internal jugular vein. If the thoracic duct is damaged, the wound is likely to fill with lymph; in such cases, the duct should always be sought and tied. A wound that discharges lymph postoperatively should always raise suspicion of damage to the thoracic duct or a major tributary. A lateral lymph node dissection encompasses removal of these lateral lymph nodes. Rarely, the submental nodes are involved by metastatic thyroid cancer as well.
The lymph node regions of the neck are divided into levels I through VII: (1) level I nodes are the submental and submandibular nodes; (2) level II are the upper jugular nodes; (3) level III are the midjugular nodes; (4) level IV are the lower jugular nodes; (5) level V are the posterior triangle and supraclavicular nodes; (6) level VI or central compartment nodes incorporate the Delphian/prelaryngeal, pretracheal, and paratracheal lymph nodes; and (7) level VII nodes are those within the superior mediastinum (see Fig. 95-12).12a
Indications for Thyroidectomy
Thyroidectomy is usually performed for the following reasons:
SOLITARY THYROID NODULES
Solitary thyroid nodules are present in 4% to 9% of patients by clinical examination, and in 22% of patients by ultrasound in the United States; most are benign.13 Therefore, rather than operating on every patient with a thyroid nodule, the physician or surgeon should select patients for surgery who are at high risk for thyroid cancer. Furthermore, each surgeon must know the complications of thyroidectomy and must be able to perform a proper operation for thyroid cancer in a safe and effective manner or must refer the patient to a center where it can be done.
LOW-DOSE EXTERNAL IRRADIATION OF THE HEAD AND NECK
A history of low-dose external irradiation of the head or neck is probably the most important historical fact that can be obtained in a patient with a thyroid nodule because it indicates that cancer of the thyroid is more likely (in up to 35% of cases), even if the gland is multinodular.14,15 Low-dose irradiation and its implications are discussed in Chapter 89. Fortunately, treatments of low-dose radiation for thymic enlargement, tonsils, and acne have long been discontinued. However, patients who had this therapy in childhood are still seen and are still at greater risk for cancer.
HIGH-DOSE EXTERNAL IRRADIATION THERAPY
High-dose external irradiation therapy, that is, more than 2000 rad, does not confer safety from thyroid carcinoma, as was previously thought.16 Rather, an increased prevalence of thyroid carcinoma, usually papillary cancer, has been found, particularly in patients with Hodgkin’s disease and other lymphomas who received upper mantle irradiation that included the thyroid gland. Usually, a dose of about 4000 to 5000 rads was given. Both benign and malignant thyroid nodules are being recognized, now that these persons survive for longer periods.17 If a thyroid mass appears, it should be treated aggressively. These patients should also be observed carefully for the development of hypothyroidism.
RISK OF IONIZING RADIATION
Children in the area of the Chernobyl nuclear accident have been shown to have at least a 30-fold increase in papillary thyroid cancer.18 This cancer also may be more aggressive than the usual papillary carcinoma. It is thought to result from exposure to iodine isotopes that were inhaled or that entered the food chain. The mechanism of radiation-induced thyroid cancer is thought to be caused primarily by chromosomal rearrangements such as RET/PTC.19
DIAGNOSIS OF THYROID NODULES
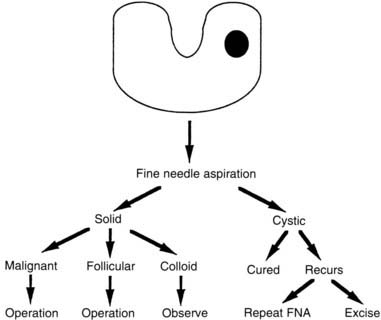
A number of diagnostic modalities have been used in the past, but currently most have been superseded by FNA of the mass with cytologic analysis. In the hands of a good thyroid cytologist, more than 90% of nodules can be categorized histologically. Approximately 65% to 70% are found to be compatible with a colloid nodule. Twenty percent demonstrate sheets of follicular cells with little or no colloid. Five percent to 10% are malignant, and less than 10% are nondiagnostic. To improve the diagnostic ability of FNA, researchers are adding biomarkers to the cytologic analyses.20,21
All patients who have malignant cytologic results should be operated on. False-positive diagnoses are rare. All patients with sheets of follicular cells with little or no colloid also should undergo surgery, because their findings are compatible with a follicular neoplasm. This nodule is called a follicular nodule or an indeterminate nodule. Most, up to 90%, prove to be benign; however, a follicular carcinoma or a follicular variant of papillary cancer may exhibit the same cytologic characteristics and cannot be differentiated by FNA. Only by careful histologic examination, after operative removal of the nodule, can follicular carcinoma and adenoma be differentiated, because follicular cancers exhibit capsular and/or vascular invasion.
When the diagnosis of colloid nodule is made cytologically, the patient should be observed and not operated on unless tracheal compression or a substernal goiter is present, or unless the patient desires the benign mass to be removed. Finally, if an inadequate specimen is obtained, FNA with cytologic examination should be repeated. With small, nonpalpable masses, FNA should be performed under ultrasound guidance. Thus, FNA with cytologic assessment is the most powerful tool in our armamentarium for the diagnosis of a thyroid nodule.
In summary, the algorithm for the diagnosis of a thyroid nodule with isotope scintigraphy and ultrasonography as initial steps (Fig. 95-9) has been replaced in most hospitals, including our own, by an emphasis on the importance of early cytologic examination of the needle aspirate (Fig. 95-10). Far fewer isotope scans are currently being done because carcinomas represent only 5% to 10% of all cold nodules. This test usually is reserved for diagnosis of a “hot” nodule.
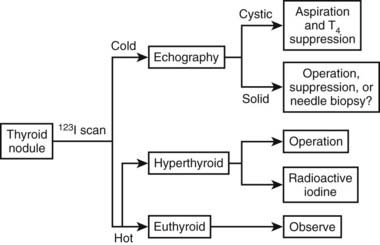
FIGURE 95-9. Algorithm for the diagnosis of a thyroid nodule that uses needle aspiration with cytologic examination of each nodule. Greater accuracy is obtained by using this diagnostic scheme.
(Courtesy Dr. Jon van Heerden.)
Preparation for Surgery
Most patients undergoing a thyroid operation are euthyroid and require no specific preoperative preparation related to their thyroid gland. Determination of the serum calcium level may be helpful, and endoscopic or indirect laryngoscopy definitely should be performed in those who are hoarse and in others who have had a prior thyroid, parathyroid, or cervical disc operation in order to detect the possibility of a recurrent laryngeal nerve injury.
HYPOTHYROIDISM
Modest hypothyroidism is of little concern when one is treating a surgical patient; however, severe hypothyroidism can be a significant risk factor. Severe hypothyroidism can be diagnosed clinically by myxedema, as well as by slowness of affect, speech, and reflexes.22 Circulating thyroxine and triiodothyronine values are low. The serum thyroid-stimulating hormone (TSH) level is high in all cases of hypothyroidism that are not caused by pituitary insufficiency, and it is the best test of thyroid function. In the presence of severe hypothyroidism, both the morbidity and the mortality of surgery are increased as a result of the effects of both the anesthesia and the operation. Such patients have a higher incidence of perioperative hypotension, cardiovascular problems, gastrointestinal hypomotility, prolonged anesthetic recovery, and neuropsychiatric disturbances. They metabolize drugs slowly and are very sensitive to all medications. Therefore, when severe myxedema is present, it is preferable to defer elective surgery until a euthyroid state is achieved.
If urgent surgery is necessary, it should not be postponed simply for repletion of thyroid hormone. Endocrine consultation is imperative, and an excellent anesthesiologist is mandatory for success. In most cases, intravenous thyroxine can be started preoperatively and continued thereafter. In general, small doses of thyroxine are given initially to patients who are severely hypothyroid, and then the dose is gradually increased.
HYPERTHYROIDISM
In the United States, most patients with thyrotoxicosis have Graves’ disease. In the United States, about 90% of all patients with Graves’ disease are treated with radioiodine therapy. Young patients, those with very large goiters, some pregnant women, and those with thyroid nodules or severe ophthalmopathy are commonly operated upon.
Persons with Graves’ disease or other thyrotoxic states should be treated preoperatively to restore a euthyroid state and to prevent thyroid storm, a severe accentuation of the symptoms and signs of hyperthyroidism that can occur during or after surgery. Thyroid storm results in tachycardia or cardiac arrhythmias, fever, disorientation, coma, and even death. In the early days of thyroid surgery, operations on the toxic gland were among the most dangerous surgical procedures because of the common occurrence of severe bleeding, as well as all the symptoms and signs of thyroid storm. Now, with proper preoperative preparation,23 operations on the thyroid gland in Graves’ disease can be performed with about the same degree of safety as operations for other thyroid conditions.
In mild cases of Graves’ disease with thyrotoxicosis, iodine therapy alone has been used for preoperative preparation, although we do not recommend this approach routinely.22 Lugol’s solution or a saturated solution of potassium iodide is given for 8 to 10 days. Although only several drops per day are needed to block the release of thyroxine from the toxic thyroid gland, it is our practice to administer two drops two or three times daily. This medication is taken in milk or orange juice to make it more palatable.
Most of our patients with Graves’ disease are treated initially with the antithyroid drugs propylthiouracil or methimazole (Tapazole) until they approach a euthyroid state. Then iodine is added to the regimen for 8 to 10 days before surgery. The iodine decreases the vascularity and increases the firmness of the gland. Sometimes thyroxine is added to this regimen to prevent hypothyroidism and to decrease the size of the gland. β-Adrenergic blockers such as propranolol (Inderal) have increased the safety of thyroidectomy for patients with Graves’ disease.23 We use them commonly with antithyroid drugs to block β-adrenergic receptors and to ameliorate the major signs of Graves’ disease by decreasing the patient’s pulse rate and eliminating the tremor. Some surgeons recommend preoperative use of propranolol alone or with iodine.24 These regimens, they believe, shorten the preparation time of patients with Graves’ disease for surgery and make the operation easier because the thyroid gland is smaller and less friable than it would otherwise be.24 We do not favor these regimens for routine preparation because they do not appear to offer the same degree of safety as do preoperative programs that restore a euthyroid state before surgery. Instances of fever and tachycardia have been reported in persons with Graves’ disease who were taking only propranolol. We have used propranolol therapy alone or with iodine without difficulty in some patients who are allergic to antithyroid medications. In such patients, it is essential to continue the propranolol for several weeks postoperatively. Remember that they are still in a thyrotoxic state immediately after surgery, although the peripheral manifestations of their disease have been blocked.
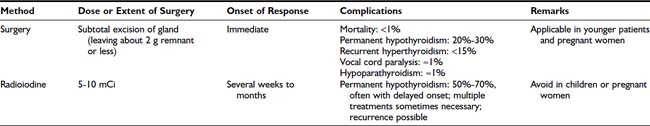
The advantages and disadvantages of radioiodine versus thyroidectomy as definitive treatment for Graves’ disease are listed in Table 95-1. Among our patients, we have never had a death from thyroidectomy for Graves’ disease in over 35 years. Surgical resection involves subtotal or near-total thyroidectomy (Fig. 95-11) or lobectomy with contralateral subtotal or near-total lobectomy. Currently we leave less than 2 g of thyroid tissue in the neck at the end of the operative procedure. Leaving more leads to a higher rate of recurrence.25 In children and adolescents, one should consider leaving smaller remnants because the incidence of recurrence of thyrotoxicosis appears to be greater in this group. Finally, when operating for severe ophthalmopathy, we try to perform near-total or total thyroidectomy. The major benefits of thyroidectomy appear to be the speed with which normalization is achieved and a lower rate of hypothyroidism than is seen after radioiodine therapy.
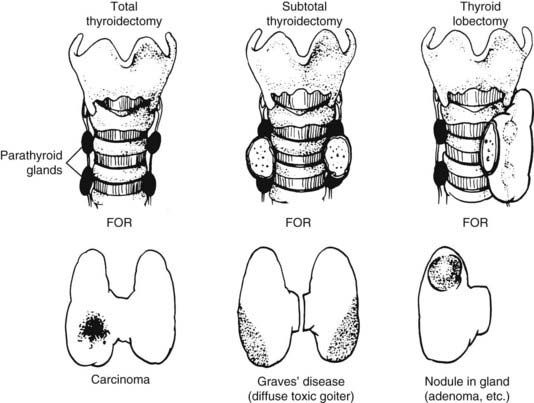
FIGURE 95-11. Common operations on the thyroid. In near-total thyroidectomy, a small amount of thyroid tissue is left to protect the recurrent laryngeal nerve and the upper parathyroid gland.
(From Kaplan EL: Surgical endocrinology. In Polk HC, Stone HH, Gardner B [eds]: Basic Surgery, 4th ed. St. Louis, Quality Medical Publishing, 1993, pp 162–195.)
Surgical Approach to Thyroid Nodules
NONIRRADIATED PATIENTS
Any nodule suspected of being a carcinoma should be completely removed, along with surrounding tissue; this means that a total lobectomy (or lobectomy with isthmectomy) is the initial operation of choice in most patients (see Fig. 95-11). A frozen section should be obtained intraoperatively. If a colloid nodule is diagnosed, the operation is terminated. If a follicular neoplasm is diagnosed, treatment is more controversial. Differentiating follicular adenoma from follicular carcinoma, or a benign Hürthle cell tumor from Hürthle cell carcinoma, with the use of frozen section is usually very difficult. These diagnoses require careful assessment of capsular and vascular invasion, which are often difficult to evaluate on frozen section. To aid in the diagnosis, enlarged lymph nodes of the central compartment are often sampled, and a biopsy of the jugular nodes is performed. If the result is negative, two options are available: (1) stopping the operation after lobectomy, with the understanding that a second operation may be necessary to complete the thyroidectomy if a carcinoma is ultimately diagnosed; or (2) performing a resection of most of the thyroid on the contralateral side. We treat most patients with benign neoplasms with thyroxine replacement anyway, even if only one lobe has been removed. Furthermore, a second operation usually is eliminated if the lesion is later diagnosed as malignant, because the remaining small thyroid remnant can be ablated with radioiodine therapy. We discuss these options with the patient preoperatively.
IRRADIATED PATIENTS
In patients with multiple thyroid nodules who have been exposed to low-dose, external irradiation of the head and neck during infancy, childhood, or adolescence, a near-total resection of the thyroid gland with biopsy of the jugular nodes is usually performed, even if a frozen section of the dominant nodule is benign. Reasons for this include the frequency of bilaterality of the disease, the known coincidence of benign and malignant nodules in the same gland, and the prevalence of papillary carcinoma in up to 35% of such patients.15 This therapy is thought to be advantageous, because small cancers can be present in the same gland, and the remaining small thyroid remnant of these patients can usually be ablated with radioiodine if a carcinoma is found on permanent section analysis. In any event, these patients require therapy with thyroid hormone. In patients with single nodules, however, we use FNA with cytology to determine the need for operation.
Patients who have received high-dose radiation to their thyroid bed (e.g., those treated with mantle irradiation for Hodgkin’s disease) are at greater risk for the development of thyroid carcinoma years later and should be monitored carefully.16 Once more, if they are operated on for nodular disease, most of the thyroid tissue should be removed, even if the dominant mass is thought to be benign.
Surgical Approach to Thyroid Cancer
PAPILLARY CARCINOMA
Surgical treatment for papillary carcinoma is best divided into two groups based on the clinical characteristics and virulence of these lesions.
Treatment for Minimal Papillary Carcinoma
The term minimal papillary carcinoma refers to a small papillary cancer, less than 1 cm in diameter, that demonstrates no local invasiveness through the thyroid capsule, that is not associated with lymph node metastases, and that often is found in a young person as an occult lesion when thyroidectomy has been performed for another benign condition. In such instances, especially when the cancer is unicentric and smaller than 5 mm, lobectomy is sufficient and reoperation is unnecessary. Thyroid hormone is given to suppress serum TSH levels, and the patient is monitored at regular intervals.
Standard Treatment for Most Papillary Carcinomas
Most papillary carcinomas are neither minimal nor occult. These tumors are known to be microscopically multicentric in up to 80% of patients; they also are known occasionally to invade locally into the trachea or esophagus, to metastasize commonly to lymph nodes and later to the lungs and other tissues, and to recur clinically in the other thyroid lobe in 7% to 18% of patients if treated only by thyroid lobectomy.26,26a
The authors firmly believe that the best treatment for papillary cancer is near-total or total thyroidectomy (see Fig. 95-11), with appropriate central and lateral neck dissection when nodes are involved. So-called cherry-picking operations, which remove only the enlarged lymph nodes, should not be performed. Rather, when tumor is found in the lateral triangle, a modified radical neck dissection should be performed27 (Fig. 95-12). At the conclusion of a modified radical neck dissection, the lymph node–bearing tissue from the lateral triangle is removed, whereas the carotid artery, jugular vein, phrenic nerve, sympathetic ganglia, brachial plexus, and spinal accessory nerve are spared and left in place. Many times sensory nerves can be retained as well. Prophylactic neck dissection of the lateral triangle should not be performed for papillary cancer; such dissections should be done only when enlarged nodes with tumor are found.
FIGURE 95-12. A, Lateral neck dissection. Note that during this procedure, the vagus nerve, sympathetic ganglia, phrenic nerve, brachial plexus, and spinal accessory nerve are preserved. In a modified neck dissection, the sternocleidomastoid muscle is not usually divided, and the jugular vein is not removed unless lymph nodes with tumor are adherent to it.
(From Sedgwick CE, Cady B: In Surgery of the Thyroid and Parathyroid Glands. Philadelphia, WB Saunders, 1980, p 180.)
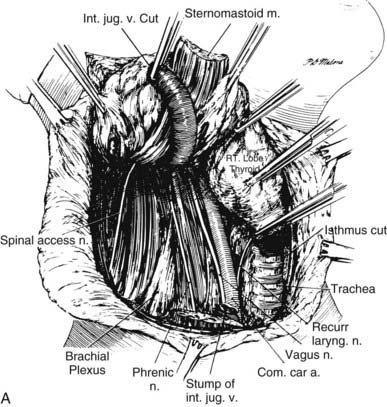
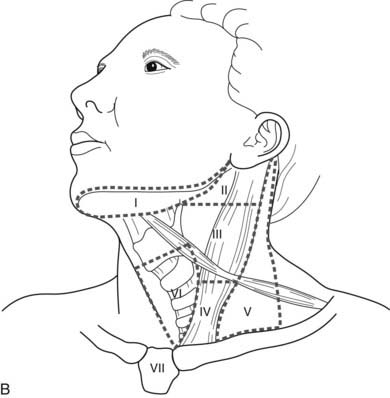
B, The lymph node regions of the neck are divided into levels I through VII: (1) level I nodes are the submental and submandibular nodes; (2) level II are the upper jugular nodes; (3) level III are the midjugular nodes; (4) level IV are the lower jugular nodes; (5) level V are the posterior triangle and supraclavicular nodes; (6) level VI or central compartment nodes incorporate the Delphian/prelaryngeal, pretracheal, and paratracheal lymph nodes; and (7) level VII nodes are those within the superior mediastinum.
In recent years, for clarity and uniformity of reporting, the location of lymph nodes in the neck and upper mediastinum has been defined as shown in Fig. 95-12B. Central lymph nodes (level VI) are frequently involved with metastases from ipsilateral thyroid cancers, as are levels III, IV, and V, which are removed in most lateral neck dissections. Although prophylactic lateral neck dissections are no longer performed, Delbridge and his group suggest that routine removal of level VI nodes (ipsilateral central compartment) should be done with total thyroidectomy to decrease the recurrence of papillary cancers postoperatively.12a They autotransplant one parathyroid as part of this procedure. We do not routinely perform this procedure because of the increased risk for hypoparathyroiditism, but we reserve it for cases in which ipsilateral central lymph nodes are clearly involved with tumor.
Surgeons with limited experience probably should not perform total or near-total thyroidectomy unless they are capable of doing so with a low incidence of recurrent laryngeal nerve injury and permanent hypoparathyroidism, because these complications are serious. Otherwise, it may be advisable to refer such patients to a major medical center where such expertise is available.
After surgery, radioiodine scanning and treatment are commonly used.28,28a 131I is taken up by most metastatic papillary cancers, but only if the TSH level is very high and normal thyroid tissue has been removed or ablated. If all or a substantial part of a lobe of normal thyroid remains, radioiodine treatment for metastases cannot be performed effectively. Usually, reoperative completion thyroidectomy is done, and then radioiodine is given. In low-risk patients, recombinant TSH preparation is sometimes used.28a
Controversies
Because randomized prospective studies have not been performed, controversy still exists over proper treatment for papillary cancer in some patients. Many clinicians now accept that patients with this disease can be separated into different risk groups according to a set of prognostic factors. With use of the AGES (age, tumor grade, extent, and size),29 AMES (age, metastases, extent, and size),30 or MACIS (metastasis, age, completeness of resection, local invasion, and tumor size)31 criteria, which evaluate risk by age, distant metastases, extent of local involvement, and size (MACIS adds completeness of excision), almost 80% of patients fall into a low-risk group. Treatment for this low-risk group is most controversial, perhaps because the cure rate is so good, certainly in the high 90% range. Should a lobectomy be done, or is bilateral thyroid resection more beneficial?
Low-Risk Papillary Cancer
Hay and associates studied 1685 patients treated at the Mayo Clinic between 1940 and 1991; the mean follow-up period was 18 years.32 Of the total, 98% had complete tumor resection, and 38% had initial nodal involvement. Twelve percent had unilateral lobectomy, whereas 88% had bilateral lobar resection; total thyroidectomy was done in 18%, and near-total thyroidectomy was performed in 60%. Cause-specific mortality at 30 years was 2%, and distant metastases occurred in 3%. These indices did not differ between surgical groups; however, local recurrence and nodal metastases in the lobectomy group (14% and 19%, respectively) were significantly higher than the 2% and 6% rates seen after near-total or total thyroidectomy.
This study is excellent. Although no differences in mortality were reported, a threefold increase in tumor recurrence rates in the thyroid bed and lymph nodes was reported in the lobectomy group. In addition, this study recognizes patients’ anxiety about tumor recurrence and their strong desire to face an operation only once and to be cured of their disease. If the operation can be done safely with low morbidity, this study supports the use of near-total or total thyroidectomy for patients with low-risk papillary cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree