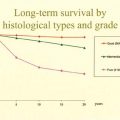
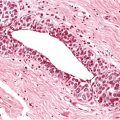
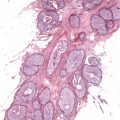
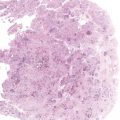
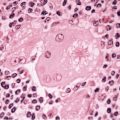
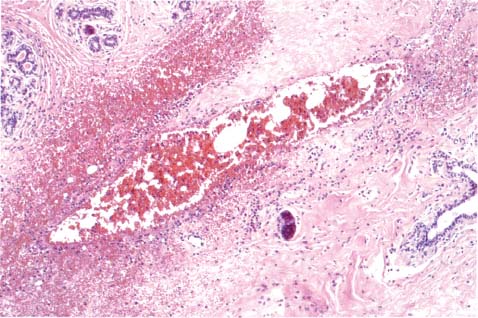
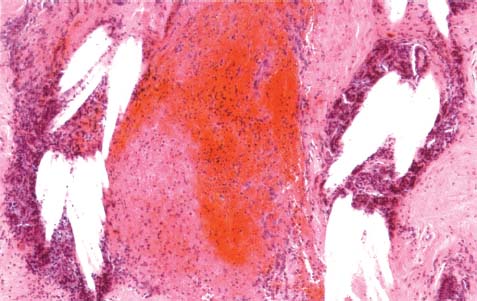
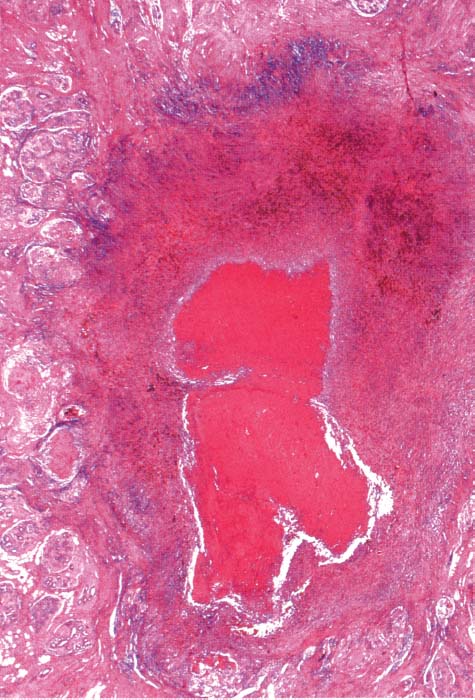
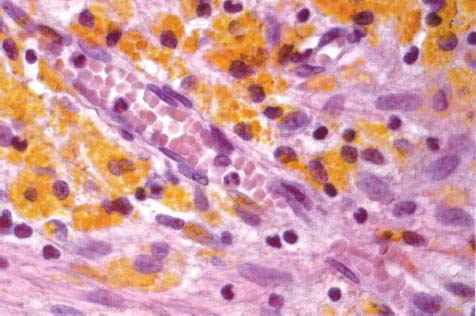
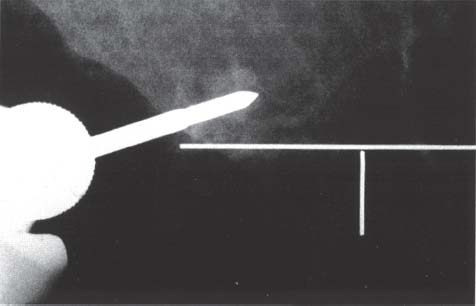
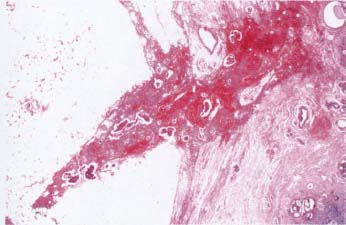
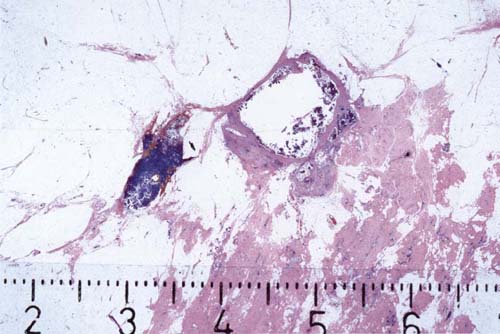
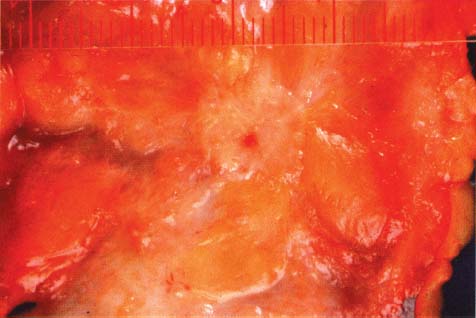
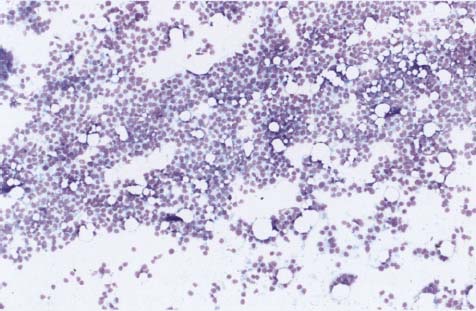
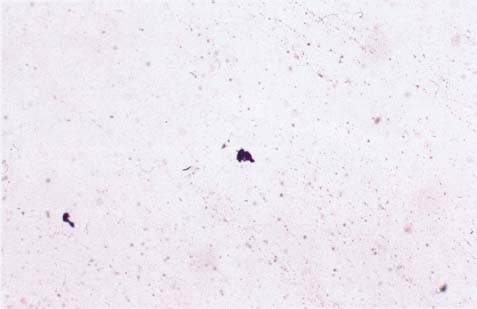
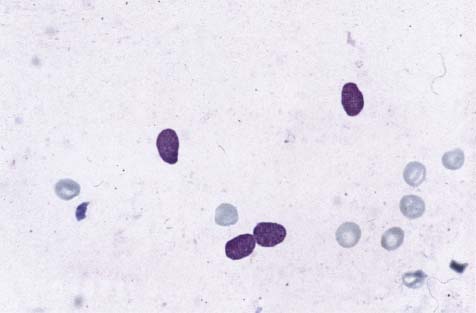
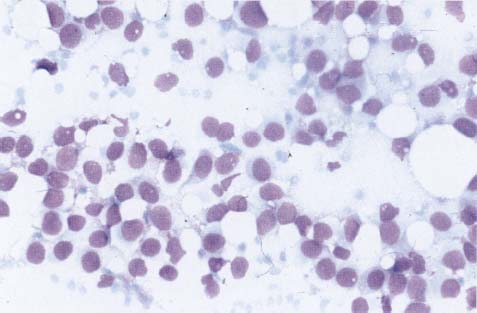
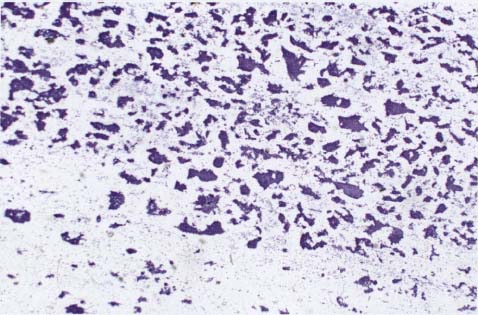
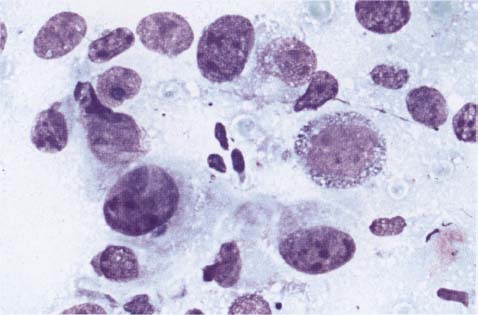
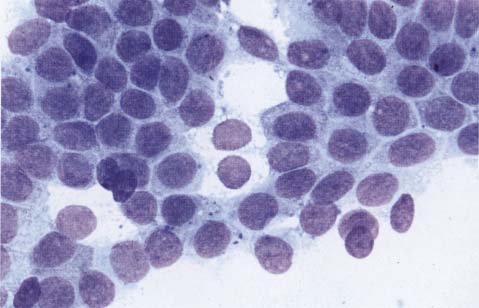
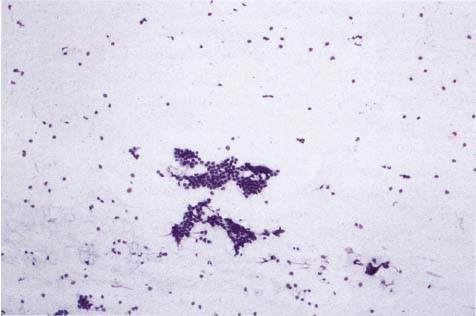
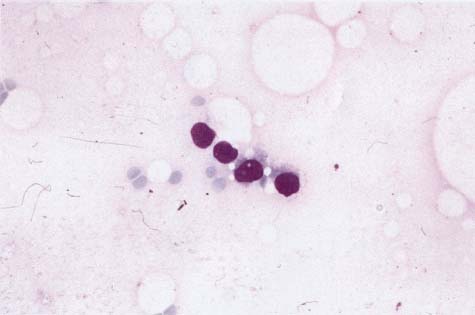
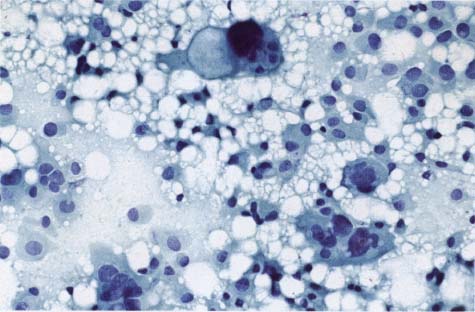
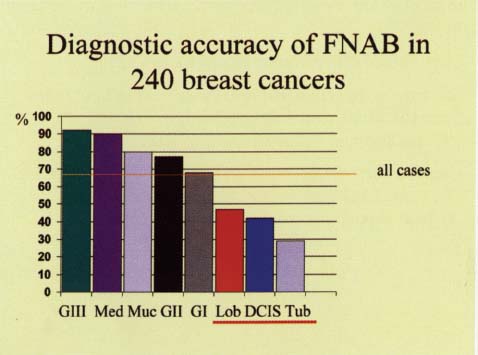
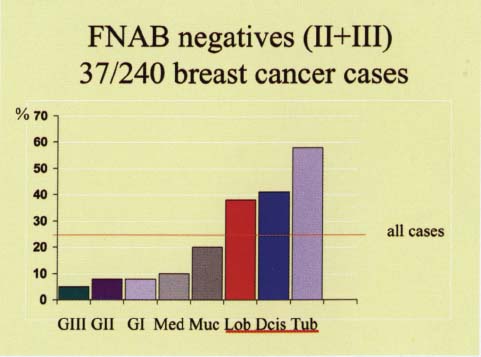
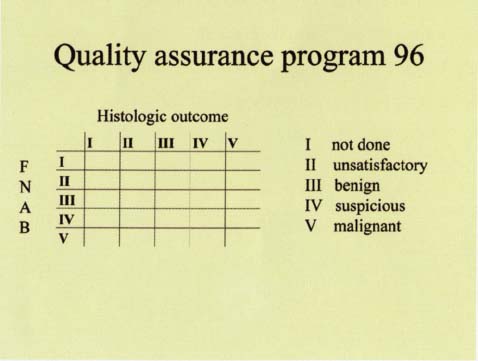
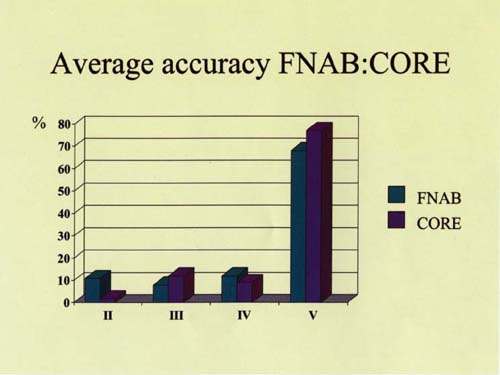
Chapter 7 Fine-needle Aspiration or Core Biopsy: A Preoperative Diagnostic Algorithm Any procedure involving use of a needle causes mechanical damage to the targeted tissue. The same is true in cases of fine-needle aspiration or core biopsy of the breast. Necrosis, needle tracks containing blood (Fig. 7.1), inflammatory cells, or cholesterol crystals (Fig. 7.2) are the most common findings. Fig. 7.1 Fig. 7.2 Sometimes an inflammatory pseudotumor forms around the damage (Fig. 7.3), with hemosiderin-containing macrophages surrounding the needle tracks (Fig. 7.4). Fig. 7.3 Fig. 7.4 Fig. 7.5 Fig. 7.7 Epithelial displacement may make it difficult for the pathologist to determine the extent of invasion (Figs. 7.6 and 7.7). Fig. 7.6 There is insufficient evidence to determine whether or not a needling procedure can initiate metastatic tumor spread, but this possibility cannot be ruled out. Because of this uncertainty, we recommend a restrictive approach when using these procedures. The aim of the diagnostic needling procedure is to obtain the minimum representative tissue needed for a definite preoperative diagnosis, while at the same time causing the least harm to the patient (compare Figs. 7.8 and 7.9). Fig. 7.8 Fig. 7.9 Fig. 7.10 Fig. 7.11 Fine-needle aspiration biopsy (FNAB) is a simple, quick, and very useful method for the preoperative diagnosis of breast lesions. In experienced hands, when used in conjunction with clinical and radiologic findings, FNAB has high sensitivity, specificity, and accuracy. Fig. 7.12 Fig. 7.13 Fig. 7.14 Fig. 7.15 Fig. 7.16 The most useful cytologic diagnostic criteria of malignancy are: – high cellularity (compare Figs. 7.10 and 7.11) – absence of myoepithelial cells (seen best in benign lesions as small, oval, bare nuclei, single or in pairs, in the background of the smear [Fig. 7.12]) – loss of cohesiveness of the epithelial cells (compare Figs. 7.13 and 7.14), and – cellular atypia (compare Figs. 7.15 and 7.16). Fig. 7.17 The goals of FNAB are not to rule out, but to verify a malignancy, if possible, and to categorize the cytologic picture rather than to type and grade the lesions. FNAB categorizes the cytologic picture as follows: II: unsatisfactory sample (Fig. 7.17) III: benign, no cytologic signs of malignancy (Fig. 7.18) IV: suspicious for malignancy (Fig. 7.19), or V: malignant (Fig. 7.20). Fig. 7.18 Fig. 7.19 Category I is reserved for cases without preoperative FNAB (see Fig. 7.23). Fig. 7.20 Fig. 7.21 Fig. 7.22 Fig. 7.23 Figures 7.21 and 7.22 show our data on the accuracy of FNAB according to tumor grade and type. While grade III carcinomas and medullary and mucinous carcinomas are easy to sample and interpret, the opposite is true for invasive lobular carcinomas, tubular carcinomas, and ductal carcinoma in situ (DCIS). The cytologist has to continuously follow up the results of preoperative FNAB comparing them to the postoperative histologic outcome. A simple method of comparison uses the table shown in Figure 7.23. On the basis of these data, statistical parameters such as sensitivity, specificity, accuracy, and false negative and false-positive rates can be calculated. An unsatisfactory rate less than 20%, absolute sensitivity over 60%, and complete sensitivity (malignant + suspicious FNABs/malignant outcome) over 80% are the suggested minimum standards. Most importantly, the false-positive rate must be as near to zero as possible. Fig. 7.24

Fine-needle Aspiration or Core Biopsy: A Preoperative Diagnostic Algorithm
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree