+8, –7/7q–, –5/5q–, i17q, 12p–, 11q23 rearr.
DIPSS int-2: 2 points
DIPPS high: 3 points
Platelets < 100 × 109/L, unfavorable karyotype, transfusion need: 1 point each
IPSS, International Prognostic Scoring System. Low risk: 0 points; intermediate-1 risk: 1 point; intermediate-2 risk: 2 points; high risk: 3–5 points.
DIPPS, Dynamic IPSS. Low risk: 0 points; intermediate-1 risk: 1–2 points; intermediate-2 risk: 3–4 points; high risk: 5–6 points.
DIPPS-Plus is based on the DIPSS, to which other three risk factors are added. Low risk: 0 points; intermediate-1 risk: 1 point; intermediate-2 risk: 2–3 points; high risk: 4–6 points.
The IPSS for PMF is based on five easily obtained clinicohematological features that allow shorter survival to be predicted: age >65 years, presence of constitutional symptoms, Hb <10 g/dL, WBC count >25 × 109/L, and the existence (≥1%) of blasts in blood. Based on the presence of none (low-risk), one (intermediate risk-1), two (intermediate risk-2), or three or more of these prognostic factors (high-risk), four risk groups with clear-cut different and non-overlapping survival curves are defined (median survival: 11.3, 7.9, 4.0, and 2.2 years, respectively; Figure 5.1).16 The IPSS demonstrated higher discriminating power than that seen in previous scoring systems and showed a high degree of replicability and predictive accuracy. The four prognostic groups could be reproduced in terms of relative survival (after adjusting for expected survival in the general population of the country of origin), thereby showing a predictive power independent of demographic or geographic factors.
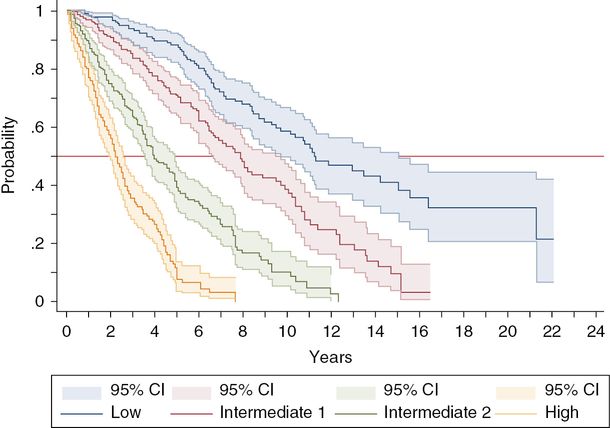
Actuarial survival curves (± 95% confidence interval (CI)) of the four prognostic groups defined by the International Prognostic Scoring System (IPSS) for primary myelofibrosis.
The IPSS is based on prognostic factors recorded at diagnosis of PMF that are not necessarily stable over the course of the disease. For instance, patients younger than 65 years at diagnosis may pass that age threshold if they survive long enough, and anemia, blasts in blood, leukocytosis, or constitutional symptoms that were absent at diagnosis may appear later on as the disease progresses. The DIPSS deals with this shortcoming and can prognosticate the remaining life expectancy at any time after diagnosis, which is important because many therapeutic decisions are not taken at diagnosis but later on. Moreover, many patients enrolled in clinical trials of new investigational drugs have usually a long disease history.
With regard to the dynamics of acquisition of new risk factors not present at diagnosis, in the original DIPSS series 26% of patients passed the 65-year threshold during the follow-up, 47% developed marked anemia (Hb <10 g/dL), 15% developed leukocytosis > 25 × 109/L, 14% had constitutional symptoms, and blood blasts appeared in 27% of them.19 The DIPSS defines the same four IPSS risk categories but increases the relative weight of developing severe anemia (Hb <10 g/dL) and upgrades the score assigned to some categories: low risk (score: 0), intermediate risk-1 (score: 1–2); intermediate risk-2 (score: 3–4), and high risk (score: 5–6). Because the upper age limit for allogeneic HSCT is set at 65 years, an age-adjusted DIPSS was also developed for younger patients, based on the DIPPS prognostic factors after excluding age.19
The DIPSS-Plus consists of a re-scored DIPSS in which three new prognostic factors were inserted: thrombocytopenia below 100 × 109/L, need for RBC transfusion, and unfavorable cytogenetics (i.e., complex karyotype or one or two abnormalities that include +8, –7/7q–, i(17q), –5/5q–, 12p–, inv(3) or 11q23 rearrangement).20
The patient herein reported did not show any of the poor risk factors included in the IPSS and had, therefore, “low-risk” PMF, which means a 50% probability of living more than 11 years (the median survival for the low-risk IPSS category). Consequently, and because she was asymptomatic, a “wait-and-see” approach was initially decided on. The patient was young enough to be considered as a candidate for a reduced-intensity allogeneic HSCT, but the high mortality of this procedure implied a poorer prognosis than the one associated with the PMF itself. Five years later, severe anemia appeared and the IPSS (now DIPSS) category increased to the “intermediate-1 risk.” Transfusion dependence, which developed 2 years later, bears a poor prognostic significance but it is not considered by the DIPSS. Ten years after PMF diagnosis, the patient reached the age of 65 and constitutional symptoms appeared. Two features increased the DISPSS score to 4, which corresponds to the “intermediate-2 risk” category and means a probability below 40% of surviving the next 5 years. Concerning the response to the JAK inhibitor ruxolitinib, the patient had marked spleen reduction, a fact that has been associated with better outcome with this drug phase III studies. Moreover, there was a rapid disappearance of the patient’s constitutional symptoms. At the time of writing, the patient is alive, nearly 20 years after being diagnosed with PMF. It must be noted that her likelihood of achieving such long survival would have been estimated at 33% according to the IPSS at time of diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree