“Bacteria, just like any other life form, need energy
to survive, multiply, and colonize. Patients with uncontrolled diabetes have high sugar content in their sweat and connective tissues, which can become a perfect energy source for bacterial colonization and subsequent infection. To make matters worse, diabetic patients also frequently have immunosuppression and microvasculopathy.”
8.1 Infection and Sepsis
Systemic infection with any microbe can present with nonspecific features of fever, tachycardia, leukocytosis, altered mental status, etc. As infection progresses, patients can start looking sicker, and develop decompensation in various organ systems, as following:
8.2 A Simplified Approach to Antibiotics for Empiric Therapy
| ||||
| ||||
| ||||
| ||||
aOther penicillins (such as Penicillin V or G, amoxicillin, ampicillin) are good against the Streptococcus group (S. viridans, S. pneumoniae, S. pyogenes) but not against staph, as staph usually have B-lactamases which deactivate penicillins. | ||||
bFor example, oral cephalexin, IV cefazolin. 1 Cephalosporins can be given in patients with mild penicillin allergy (e.g., rash), but are contraindicated in patients with severe penicillin allergy (e.g., anaphylaxis, Stevens-Johnson syndrome, allergic interstitial nephritis). | ||||
cIV forms are ceftriaxone, cefotaxime, and ceftazidime. Oral forms are cefpodoxime and cefdinir. These drugs have good Streptococcus/Staphylococcus coverage as well, but not as good as 1st generation cephalosporins or B-lactamase resistant narrow-spectrum penicillins.1 | ||||
dAminoglycosides for pseudomonas is usually not used as monotherapy, but as an adjunctive treatment for serious infections. | ||||
eUnlike piperacillin-tazobactam, carbapenems cover extended spectrum beta-lactamase (ESBL)-producing superbugs, such as Acinetobacter baumannii or ESBL E. coli/Klebsiella. 2 Meropenem or imipenem may be the right answer in a patient with prolonged hospitalization and evidence of active gram-negative infection who does not improve despite adequate antibiotic therapy. The only difference of coverage in between (meropenem, doripenem, imipenem) and ertapenem, is that ertapenem does not cover Pseudomonas. | ||||
fThe old dictum of treating above-diaphragm infection (e.g., lung abscess) with clindamycin and below-diaphragm infection (e.g., intestinal infection or perforation) with metronidazole no longer applies. Clindamycin is no longer preferred due to increased risk of C. difficile. The preferred antibiotics for treatment of aspiration pneumonia now are amoxicillin-clavulanate, or third-generation cephalosporin + metronidazole. | ||||
Abbreviations: IV, intravenous; MRSA, methicillin-resistant Staphylococcus aureus | ||||
8.2.1 Other Bacteria and Their Antibiotic Coverage
8.2.2 Example Clinical Cases
Cellulitis without MRSA risk factorsa | ||
Ceftriaxoneb + metronidazole | ||
Infections with risk factor for Pseudomonasc | ||
Streptococcus spp., gram negatives (Moraxella catarrhalis, Haemophilus influenzae), and atypicals. | ||
a MRSA risk factors: IVDA (intravenous drug abuse), human immunodeficiency virus (HIV) positive, recent prior antimicrobial therapy, hemodialysis, recent hospitalization, residence in long-term care facility such as nursing homes, etc. | ||
bNowadays third-generation cephalosporins are preferred over quinolones (e.g., ciprofloxacin), because quinolones are associated with higher risk of C. difficile and other side effects. | ||
cRisk factors for Pseudomonas infection include the following: | ||
Abbreviations: GI, gastrointestinal; IV, intravenous; MRSA, methicillin-resistant Staphylococcus aureus. | ||
Neutropenic fever (always look at WBC count in a question about empiric antibiotic therapy)
Hospital-acquired pneumonia, especially in intubated patient
Severe pulmonary infection in a patient with cystic fibrosis
Diabetes mellitus with certain infections such as malignant otitis externa
Cellulitis and osteomyelitis associated with a punctured sole wound
8.2.4 Notable Side Effects of Antibiotics
8.3 Skin Infections
Potential autoimmune complication of strep infection (e.g., erysipelas, cellulitis, strep throat) is Rheumatic fever and postinfectious glomerulonephritis (glomerulonephritis can also occur with staph infection).
Cellulitis management depends on the type of cellulitis:
1. Management of non-purulent cellulitis
MRSA risk factora | ||
Cellulitis with signs of severe infection (e.g., fever, tachycardia) | IV vancomycin or ceftaroline | |
IV cefazolin | ||
| ||
aRisk factors for MRSA include – IVDA (intravenous drug abuse), HIV positive status, recent prior antimicrobial therapy, hemodialysis, recent hospitalization, residence in long-term facilities such as nursing homes, etc. | ||
bUnlike clindamycin or trimethoprim-sulfamethoxazole, doxycycline doesn’t have good streptococcus coverage (hence it is combined with amoxicillin or cephalexin). | ||
2. Management of – Purulent Cellulitis or – abscess with significant cellulitis, systemic symptoms or immunosuppression
These cases are almost always due to Staph and MRSA coverage is needed.
High risk population for Infective endocarditisa | |
Severe infection: IV Vancomycin or Daptomycin | |
aExamples of high risk conditions include prosthetic cardiac valve (including bioprosthetic heart valve), previous infective endocarditis, unrepaired cyanotic congenital heart disease, etc. Please refer to infective endocarditis section discussed later in this chapter. | |
Clinical tip : Note in all the above situations if Cellulitis is associated with periodontal disease, perirectal location, pressure ulcer or with prominent necrosis , it warrants anaerobic coverage.
8.3.1 Necrotizing Fasciitis and Differential Diagnoses
The following severe soft tissue infections usually have signs of systemic toxicity (Toxic shock syndrome is included in this table as sometimes cellulitis can lead to toxic shock syndrome and cause severe systemic toxicity).
Polymicrobial (gram positive, gram negative, anaerobes, MRSA, etc.) | Clostridium perfringens or Clostridium histolyticum | Staph, aureus a | |
May not have bacterial point of entry at all, or may have coexistent groin ulcer or colonic fistula. | More likely to have hx of trauma. Trauma can be as minor as intramuscular injection, or as major as surgery. | Look for foreign body in situ (tampons or prosthesis), or an active site of Staph. infection, (e.g., osteomyelitis, or even cellulitis) | |
They do have overlapping features | |||
Surgical exploration. Surgical specimens’ wound gram stain/ culture can differentiate in between them. | |||
Adjunctive empiric antibiotic treatment (Intravenous immunoglobulin, which neutralizes toxins, can be tried in severe cases.) | One broad spectrum antibiotic (meropenem or piperacillin/tazobactam or ampicillin-sulbactam) + | Penicillin | Clindamycinb |
aThis is due to colonization or infection with Staph. aureus that produces toxic-shock-syndrome-toxin (TSST). This toxin is unique in that it non-specifically activates T-helper cells, which release excess inflammatory mediators into the bloodstream causing SIRS, sepsis and even death. | |||
8.3.2 Diabetic Foot Ulcer Infection
In patients with diabetic foot ulcer infection, workup for osteomyelitis is recommended if one or more of the following are present:
8.4 CNS Infections
In a nutshell: clinical presentation and likely Dx
+ Stiff neck or other signs of meningismusa | |
+ Focal neurological deficit (e.g., right lower extremity weakness) | |
Encephalitisb | |
aSigns of meningeal inflammation include photophobia, Kernig’s sign (inability to straighten the leg when hip is flexed), and Brudzinski’s sign (neck flexion causes reflexive flexion of hips and knees). 4 Remember that subarachnoid hemorrhage can present similarly with signs of meningeal infl ammation and fever. | |
bViral causes of encephalitis include:
Encephalitis can also be associated with Systemic Lupus Erythematosus (SLE), acute disseminated encephalomyelitis, etc. | |
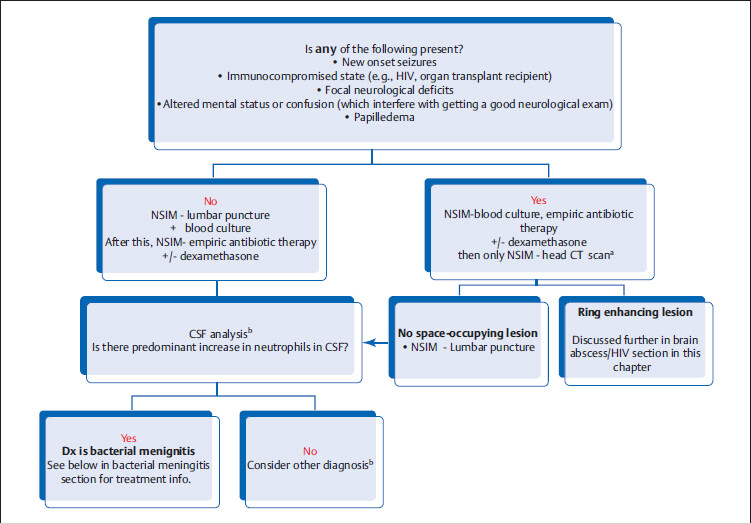
8.4.1 General Management of Suspected CNS Infection
aIf there is a suspicion for space-occupying lesion, perform computed tomography (CT) scan prior to lumbar puncture as lumbar puncture can precipitate brainstem herniation in patients with elevated intracranial pressure (ICP). Also give antibiotics, as diagnostic workup should not delay life-saving antibiotic therapy.
Normala | ||||
aAs opposed to viruses, organisms like bacteria, fungi, and mycobacteria directly use glucose for energy production. | ||||
8.4.2 Bacterial Meningitis
:
Empiric Treatment of Bacterial Meningitis
Empiric IV antibiotics of choicea | |
Gentamicin (or some-other aminoglycoside). Ampicillin b + Cefotaximec | |
Community-acquired Meningitis | |
If neonate never left the hospital, consider this hospital acquired – vancomycin + aminoglycoside+ cefotaximec | |
Vancomycin b + Ceftriaxone or cefotaxime | |
> 50 years of age, or | |
Community-acquired meningitis with risk factor for Pseudomonas, such as neutropenia, severe immunocompromised state (e.g., lymphoma, high-dose steroids, chemotherapy | Vancomycin d + ampicillin b + antipseudomonal cephalosporin |
Hospital acquired meningitis (penetrating trauma or postsurgery meningitis) | |
aConsider adding dexamethasone (except in neonates < 6 weeks old). In children, the greatest benefit of dexamethasone is in suspected H. influenzae meningitis; in adults in pneumococcal meningitis. It should be given concurrently with or immediately before the first dose of antibiotics, there’s probably no benefit if the corticosteroid is given after antibiotics are initiated. It reduces inflammation and decreases risk of neurologic complications, such as hearing loss. | |
cCeftriaxone is contraindicated in this age group because of increased risk of biliary stasis. | |
dVancomycin is added in countries where pneumococcal resistance rate to ceftriaxone is > 1% e.g., USA, Canada. | |
The first exposure of a baby is to maternal vaginal flora, which may include S. agalactiae and E. coli.
In infants, community-acquired Streptococcus is most prevalent.
When a child starts attending day care, kindergarten and then school, there is increased crowding and hence increased risk of Neisseria.
As one becomes an adult and is no longer living in dorms or exposed to classmates, the incidence of Neisseria decreases, and community-acquired Streptococcus again becomes more prevalent.
GAC= Gentamicin + Ampicillin+ Cefotaxime
Coverage for vancomycin-resistant S. pneumoniae is not needed.
Age > 50, or with risk factors, give VACS therapy: Vancomycin, Ampicillin, Cephalosporin, and Steroids (dexamethasone)
Additional unique clinical features include:
It can also cause hemorrhagic infarction of adrenal glands leading to acute adrenal crisis (severe hypotension).
N. meningitis prophylaxis is indicated (with either rifampin or ciprofloxacin) in the following situations:
Close contacts of N. meningitis patients—all household members, childcare center, military recruits in training center, and roommates/dorm mates. (Note: classmates or coworkers are not automatically considered as close contact.)
Health care providers who were exposed to respiratory secretions of patients with N. meningitis, e.g., a clinician who performed endotracheal intubation.
8.4.3 Lymphocytic Meningitis
Rickettsia causing Rocky Mountain spotted fever (RMSF)a | |||
If India ink test is negative in a HIV-positive patient with lymphocytic meningitis, NSIDx is cryptococcal antigen test in CSF | |||
AFB stain of spinal fluid obtained daily for 3 days, and CSF nucleic acid testing. | |||
Viral meningitis | |||
Early bacterial meningitis or partially treated bacterial meningitis | Consider empiric antibiotics, especially in very young, elderly, or immunocompromised patients, or who have received antibiotics prior to presentation. | ||
aUnlike lyme meningitis, RMSF may have neutrophilic predominant CSF, but cell count is usually below <100 cells/μL. Differential diagnosis of RMSF is N. meningitis: | |||
Abbreviations: CSF, cerebrospinal fluid; HSV, herpes simplex virus; NSAIDs, nonsteroidal anti-inflammatory drugs; PCR, polymerized chain reaction. | |||
8.4.4 HSV-1 Meningoencephalitis
Background: This can be due to primary infection or latent reactivation of HSV-1. (This is the same virus that causes cold sores)
Presentation: Affects predominantly temporal lobes, hence patients may present with symptoms of visual, auditory, or olfactory hallucinations or even seizures.
Usually presents with acute confusion and personality changes, thus CT scan is done prior to lumbar puncture. CT scan may reveal unilateral or bitemporal lobe abnormalities or hemorrhage. With clinical and/or CT findings suggestive of HSV-1; NSIM is IV acyclovir.
8 This can be life-saving; do not wait for further diagnostic procedures if HSV CNS infection is suspected.
NSIM is lumbar puncture with HSV-1 PCR (most accurate test). CSF fluid typically shows increased lymphocytes + increased RBCs. After that, brain magnetic resonance imaging (MRI) is recommended to assess temporal lobe involvement.
A 25-year-old male presents to the hospital with fever and seizures. Patient is diagnosed with herpes viral encephalitis. After few days, patient develops hypersexuality and is seemingly very apathetic to other issues. He is also found to be putting things in his mouth a lot (hyperorality, which is tendency to examine objects by mouth).
8.5 Upper Respiratory Tract Infection (URTI)
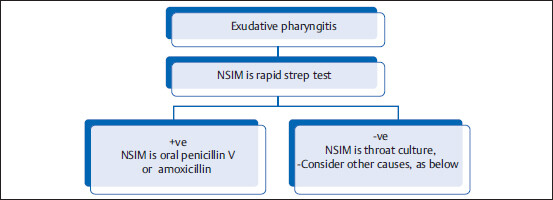
8.5.1 Acute Exudative Pharyngitis or Tonsillitis
Background: Two most common causes of exudative pharyngitis/tonsillitis are Epstein–Barr virus (EBV) and strep.
Ruling out S. pyogenes infection is important because if not treated promptly, it carries an increased risk of rheumatic fever or glomerulonephritis.
Usually absenta | ||||
Presentb | ||||
-vec | ||||
May be presentd | May be presente | |||
aHowever, adenovirus or herpes virus pharyngitis may have exudates. | ||||
bCoexistent symptoms such as nasal congestion, dry cough, conjunctivitis pointing toward viral origin. | ||||
cUsually associated with local cervical lymphadenopathy, but not generalized. | ||||
dMaculopapular rash, if present, signifies that patient might have been exposed to antibiotics (e.g., amoxicillin) prior to presentation. | ||||
ePatients with acute retroviral syndrome may have painful mucocutaneous ulcerations (oral, esophageal, penile, etc.) and generalized well-circumscribed salmon-colored macules or papules. | ||||
8.5.2 Infectious Mononucleosis
Background: EBV is transmitted by salivary secretions, e.g., during kissing (hence, especially prevalent in college students) .
NSIM/NSIDx is rapid strep throat test. If negative, NSIDx is CBC with peripheral blood smear, and heterophile antibody test (a.k.a. monospot test).
11 Monospot test detects the presence of antibody against RBC antigen of sheep and horse. This test is both very sensitive and specific; however, it can be negative in early infection.
If monospot test is negative, NSIDx is either repeating monospot test or serologic testing for antibodies against EBV-specific proteins (viral-capsid antigen or early nuclear antigen).
12 If both monospot test and antibodies against EBV-specific proteins are negative, then consider the following causes:
• CMV: Known as heterophile-negative infectious mononucleosis
• HIV: Acute retroviral syndrome
Treatment: Supportive (acetaminophen ± NSAIDs).
Consider steroids if any of the following is present:
Complication: Splenic rupture (patients are advised to avoid non-contact sports for 3 weeks and contact sports for at least 4 weeks).
A 24 y/o college-going male patient presents with exudative pharyngitis, posterior cervical lymphadenopathy, and fatigue for the last 10 days.
8.5.3 Influenza
Presentation: Fever, myalgias (generalized muscle pain), headache, and upper respiratory symptoms, such as runny nose and nonproductive cough (due to the postnasal drip). Chest X-ray (CXR) may show increased interstitial marking due to viral bronchitis.
Workup: Rapid molecular DNA-based testing is preferred (e.g., RT-PCR). Antigen-based detection has lower sensitivity, but can also be used.
Rx: Antivirals (Oseltamivir or Zanamivir). Indication for antiviral treatment has been broadened. The only group that might not be treated is healthy patients < 65 years of age with uncomplicated influenza who present after >48 hours of symptoms, or who are already feeling better or pediatric population.
Complications: Adult respiratory distress syndrome, severe necrotizing pneumonia due to S. Aureus.
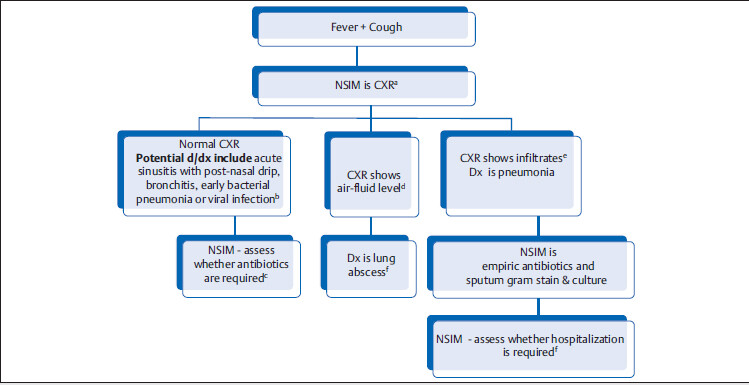
8.6 Lower Respiratory Tract Infection
Common differential dignosis of “fever + cough” are acute bacterial sinusitis with postnasal drip, bronchitis, pneumonia, and lung abscess.
aDo not choose CBC as the NSIM, because it does not help to make diagnosis.
bIn hospitalized patients with hx of sick contacts or coexistent upper respiratory tract symptoms, a PCR testing that detects common viruses (e.g., RSV, parainfluenza, influenza) can be done.
cYoung patients without comorbid conditions and low-grade fever may not need antibiotics.
Empiric antibiotics used for treatment of bronchitis are similar to sinusitis (same microbiologic cause): amoxicillin-clavulanate or doxycycline.
eLobar pneumonia with multiple air bronchograms and absence of significant tracheal deviation (If there was lung opacity similar to this but with tracheal deviation to the same side and no air bronchogram, the diagnosis would be more likely atelectasis).
Source: Imaging. In: Gunderman R, ed. Essential Radiology. Clinical Presentation, Pathophysiology, Imaging. 2nd ed. Thieme; 2000.
fLung abscess is commonly a sequelae of aspiration (look for risk factors of aspiration, e.g., advanced dementia, alcoholism). NSIM is sputum gram stain/culture and CT thorax to rule out obstructive pathology. Empiric antibiotics should cover anaerobes (e.g., amoxicilin-clavulanate). Antibiotics is continued until chest imaging is clear (might take weeks).
gIf you think the patient is sick (e.g., septic, hypoxemic, and/or immunocompromised), then NSIM is to hospitalize the patient and give IV antibiotics (after taking blood cultures). There is a CURB-65 criteria to help you make that decision too.
If any of the following present, consider hospitalization:
• Blood pressure—systolic BP < 90 mmHg
• 65 or older aged patient (particularly if patient lives alone).
8.6.1 Pneumonia
Patient living in community and with no risk factor for infection with multidrug-resistant organisms | Streptococcus, H. influenzae, mycoplasma, etc. (see table below for empiric therapy) | |
Hospital-acquired pneumoniaa | Patient develops pneumonia after more than 48 hours of hospitalization |
|
Intubated patient develops new-onset fever and has increased secretions, more than 48 hours after intubation. | ||
aHealth care-associated pneumonia (HCAP) is no longer included in recent guidelines. Treatment depends upon individual risk factors. | ||
bConsider double pseudomonal coverage in very sick patients (e.g., Tobramycin + cefepime). | ||
Empiric Antibiotic Treatment for Community-Acquired Pneumonia
No recent antibiotic use, CURB-65 is absent, AND patient has no comorbidities | Hospitalized patient, recent antibiotic use, OR presence of comorbidities (e.g., diabetes, alcoholism, chronic liver disease, immunosuppression) |
| |
aOlder generation quinolones like ciprofloxacin, norfloxacin, or ofloxacin do not cover Streptococcus. | |
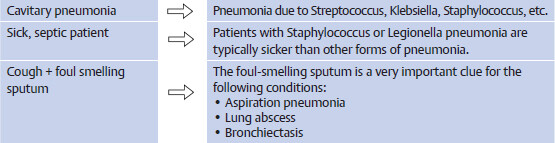
Specific Clinical Situations Involving Pneumonia
10. A 65-year-old alcoholic, active smoker patient who recently went to a convention has pneumonia. What is the likely cause?
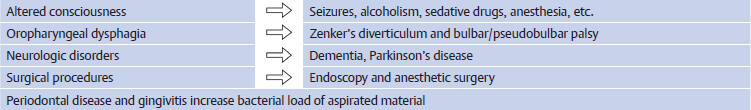
8.6.2 Aspiration Pneumonia/Pneumonitis
Conditions that can predispose to aspiration:
Impaired swallowing and epiglottic reflex lead to increased risk of aspiration of oropharyngeal and gastric contents into the lung