Survival estimates from diagnosis of primary myelofibrosis patients who become intermediate-2 and high-risk International Prognostic Score System (IPSS) with a blast cell count <10% at any time of their follow-up for the COMFORT-II (n = 100) and Dynamic IPSS (DIPSS) (n = 350) cohorts. HR, hazard ratio. (Source: Passamonti F, Maffioli M, Cervantes F, et al. Impact of ruxolitinib on the natural history of primary myelofibrosis: a comparison of the DIPSS and the COMFORT-II cohorts. Blood. 2014;123(12):1833–5. Reproduced with permission.)
It has been reported that ruxolitinib therapy may delay, arrest, or, in some cases, reverse BM fibrosis over the long term in patients with primary or secondary MF.16 Moreover, results from COMFORT-II showed that ruxolitinib can induce a significant reduction in the JAK2 V617F allele burden compared to BAT.17 Somewhat unsurprisingly, both phenomena were found in patients with greater spleen reduction and symptom improvement. Whether these parameters are also associated with improved survival remains to be defined.
Recently, mutations of the calreticulin gene (CALR) have been found in the majority of JAK2 and MPL mutation-negative MF and ET cases. Mutated CALR appears to activate signaling pathways similar to those activated by JAK2 (i.e., STAT5), further underscoring the role of JAK-STAT signaling in MF. The efficacy of JAK2 inhibitors in these patients has not yet been studied. However, because ruxolitinib has been shown to be equally effective in patients with and without JAK2 V617F, testing for mutations is not required before prescribing ruxolitinib.
In conclusion, treatment with ruxolitinib results in significant reduction of the spleen size and marked improvement in MF-related symptoms, leading to a significantly improved quality of life (Figure 10.2). Therefore, candidates for ruxolitinib therapy include MF patients with symptomatic splenomegaly and those with significant disease-related constitutional symptoms. Treating physicians should be mindful that these two clinical problems often coexist in the same patient. Also, it is important to remember that ruxolitinib has been developed in patients with advanced MF (intermediate-2 or high-risk, according to the IPSS), who have a median survival of 2–4 years. In that population, ruxolitinib has resulted in a consistent survival benefit. Studies of ruxolitinib in patients with MF at earlier stages (low and intermediate-1 risk by IPSS, median survival of 8–11 years) to potentially prevent disease progression are awaited.
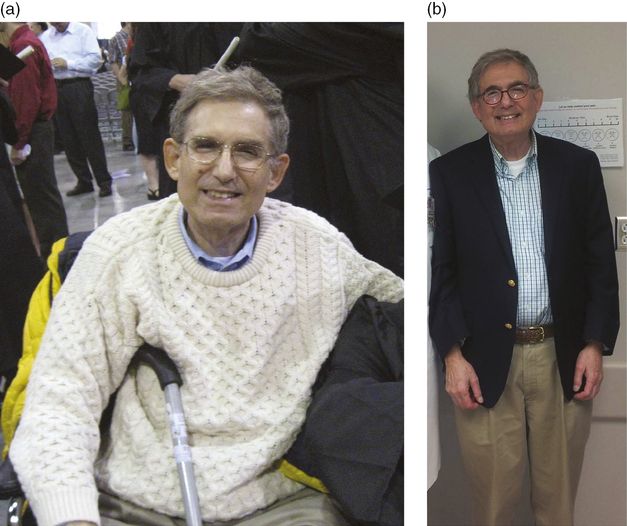
Patient with advanced myelofibrosis at the start of ruxolitinib therapy (a, April 2008) and currently on ruxolitinib therapy (b, January 2014). Before treatment, the patient had lost a significant amount of weight, had severe fatigue, and needed to use a cane to walk. Nearly 6 years later and still receiving ruxolitinib, the patient has gained weight, reports having more energy, and had a significantly improved quality of life. (Source: Verstovsek S. Changing myelofibrosis’s natural course at last. Blood. 2014;123(12):1776–7. © The American Society of Hematology. Reproduced with permission.)
Management of anemia
Case 2
A 68-year-old man with no significant comorbidities presents with a 6-month history of progressive fatigue. Over the past month he has also complained of night sweats and early satiety. He was previously a fairly active man and used to play golf twice a week with his friends. Now he cannot keep up with it and feels like he has lost some weight. On physical exam muscle wasting is noted. His spleen is palpable 18 cm below the costal margin and 1–2 cm across the midline. CBC shows WBC = 3.1 × 109/L, hemoglobin = 94 g/L, and platelets = 282 × 109/L. Schistocytes are noted in the PB smear. A BM biopsy is consistent with MF. The patient is therefore started on therapy for primary MF with the oral JAK2-inhibitor ruxolitinib at the initial dose of 20 mg twice daily. After 4 weeks of treatment his CBC shows WBC = 2.8 × 109/L, hemoglobin = 95 g/L, and platelets = 170 × 109/L. After 8 weeks, WBC = 3.8 × 109/L, hemoglobin = 88 g/L, and platelets = 143 × 109/L. The patient returns for follow-up after 12 weeks of treatment. He does not feel “that bump” in his abdomen any more and has had the best appetite in months. However, he still complains of fatigue, especially on exertion. His CBC at this point shows WBC = 5.1 × 109/L, hemoglobin = 82 g/L, and platelets = 123 × 109/L.
Given the central role of the JAK/STAT signaling pathway in normal hematopoiesis, cytopenias are expected side effects of ruxolitinib therapy. In particular, anemia is the most common adverse event associated with this treatment. The issue is further complicated by the fact that patients with advanced MF often present with transfusion-dependent anemia. Treating physicians should therefore expect to encounter and be familiar with the management of this complication.
In the initial phase I/II study of ruxolitinib in patients with MF, new-onset anemia occurred in nearly one-quarter of patients who were transfusion-independent at baseline and was dose-dependent.7 In COMFORT-I, among 155 patients treated with ruxolitinib, grade 3–4 anemia was observed in 45.2% of patients (vs. 19.2% in the placebo group).9 Mean hemoglobin levels and transfusion requirements reached a nadir at 8–12 weeks and recovered to levels close to baseline by week 24. The incidence of events was highest within the first 6 months, and decreased after 12 months.12 In that study, anemia was managed with dose adjustments and red blood cell (RBC) transfusions. Doses could be re-escalated in a step-wise fashion once blood counts had recovered. Although more than half of the patients in the ruxolitinib arm required dose reductions, only one discontinued therapy due to anemia.9 Moreover, patients who had their dose reduced to 10 mg twice daily had faster recovery to pretreatment hemoglobin levels while preserving the clinical benefits.12 A similar pattern of anemia was observed in COMFORT-II. However, thanks to an analogous policy of dose reductions and RBC transfusions, no patient was ultimately taken off study due to severe anemia.10 A recent postmarketing analysis of 28 patients with primary or post-PV/post-ET MF who were prescribed ruxolitinib confirmed the effects of ruxolitinib on anemia. Geyer et al. reported that 9 (32%) patients required RBC transfusions, and 2 of them (who had baseline anemia) ultimately discontinued ruxolitinib due to worsening cytopenias.18
Anemia is the most frequent side effect of ruxolitinib therapy. Close follow-up of patients during the first 2–3 months of treatment is mandatory and proactive dose adjustments should be implemented in order to maintain patients on therapy at effective dosages (≥10 mg twice daily; see below) and avoid interruptions. Interruption of therapy usually results in return of the patient’s symptoms to baseline within 10 days. Importantly, the development of transfusion-dependent anemia due to ruxolitinib does not offset its benefits provided that a final titrated dose of ruxolitinib ≥10 mg twice daily is achieved. Moreover, concomitant administration of agents to ameliorate anemia (danazol or low-dose thalidomide) could be considered. Finally, although ruxolitinib-related cytopenias are to be expected, there will be variability in the degree to which these occur in patients with similar baseline blood counts. Therefore, dose adjustments should always be weighed against the individual patient’s response and hematologic parameters.
Baseline thrombocytopenia
Case 3
A 64-year-old man presents with a history of primary MF that was first diagnosed 5 years ago. He had been observed for the first 3 years after his diagnosis. Subsequently, he developed significant fatigue, weight loss, and splenomegaly, and his CBC had shown progressive leukocytosis with a left shift. Therefore, he was started on hydroxyurea and supportive care in the form of periodic RBC transfusions. For the subsequent 2 years he failed to present at follow-up visits. However, over the past 12 months he has complained of recurrent, progressively worsening fatigue and, more recently, early satiety, night sweats, and pruritus. He became concerned and asked his primary care doctor to be referred to a hematologist. He has heard of a new drug that is specific for his MF and thinks he might benefit from it. A laboratory workup at the time of referral shows WBC = 22.1 × 109/L, hemoglobin = 107 g/L, platelets = 106 × 109/L, presence of leukoerythroblastosis, and 2% blasts. The patient is considered for treatment with ruxolitinib.
As previously mentioned, the dose-limiting toxicity of ruxolitinib in the treatment of MF is thrombocytopenia. Accordingly, a few key points have emerged regarding the management of patients who develop this side effect. First, baseline platelet counts should be used to determine patient eligibility for ruxolitinib treatment and which starting dose of ruxolitinib is more appropriate. Second, it is critical that patients started on ruxolitinib have their CBC monitored closely (ideally measured weekly) to allow for proactive dose adjustments and to avoid treatment interruptions during the first 8–12 weeks of therapy or until a stable regimen has been achieved.
In COMFORT-I, ruxolitinib was started at a dose of 15 mg twice daily for patients with a baseline platelet count of 100–200 × 109/L and 20 mg twice daily for those with a baseline platelet count greater than 200 × 109/L. In addition, mandatory dose reductions were implemented for decreasing platelet counts and treatment was interrupted for platelet counts <50 × 109/L. Ruxolitinib could be resumed and doses could be increased after the platelet count had recovered to acceptable levels as specified in the protocol. Blood count monitoring was therefore recommended at least weekly for platelet counts <100 × 109/L and at least twice weekly for platelet counts <50 × 109/L.9
As observed for anemia, thrombocytopenia was more common in the early phases of therapy. By week 8, patients with a baseline platelet count of 100–200 × 109/L had a 25% mean decrease in platelet counts, while those with a baseline platelet count >200 × 109/L had a 43% mean decrease. This decline was generally followed by stabilization of the platelet counts, and only 1 patient ultimately discontinued treatment due to thrombocytopenia.19 Overall, about three-quarters of patients with a baseline platelet count of 100–200 × 109/L and nearly 40% of those with a platelet count >200 × 109/L required dose reductions due to thrombocytopenia.
The median final titrated dose at week 24 was 10 and 20 mg twice daily for patients starting at 15 and 20 mg twice daily, respectively. Importantly, final titrated ruxolitinib doses ≥10 mg twice daily were associated with greater median reductions in spleen volume at week 24 than final titrated doses of 5 mg twice daily. Similarly, the median improvement in TSS was significantly higher at titrated doses ≥10 mg twice daily than at ≤5 mg twice daily.9 Based on these results, the currently recommended ruxolitinib starting doses are 20 mg twice daily for patients with baseline platelet counts ≥200 × 109/L and 15 mg twice daily for those with baseline platelet counts between 100 and 200 × 109/L. A similar approach to the management of thrombocytopenia was adopted in COMFORT-II, resulting in analogous dosing recommendations outside the USA.10 Finally, in their postmarketing analysis, Geyer et al. reported that the reduction in platelet counts was mild in the majority of patients and only 1 patient discontinued ruxolitinib due to thrombocytopenia.18
A validated strategy for ruxolitinib dosing in patients with MF and baseline platelet counts of ≤100 × 109/L had not been established until recently, as neither COMFORT-I nor COMFORT-II had included such patients. The first analysis of a study of ruxolitinib in patients with MF and baseline platelet counts of 50–100 × 109/L showed that, when treatment is initiated at 5 mg twice daily and carefully escalated according to the patient’s cell counts, reduction in spleen volume and improvements in TSS at week 24 compared favorably with those seen in patients with platelet counts of 100–200 × 109/L enrolled in COMFORT-I.20 Based on these findings, the ruxolitinib prescribing information in the USA has been amended to include patients with a baseline platelet count of 50–100 × 109/L at a starting dose of 5 mg twice daily with subsequent dose modifications based on the clinical response and changes in platelet count, up to a maximum dose of 10 mg twice daily.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree