Fig. 1.1
Original intra-arterial blood pressure recording performed in a patient before, during, and after a 15 min visit by a physician unknown to the patient. Arrows indicate the beginning and the end of a 15 min doctor’s visit. ABP pulsatile arterial BP, MAP mean BP, ABP* BP values integrated every 10 min, HR heart rate (Taken from Mancia et al. [54] with permission)
Remarkably, the increase in BP levels during the clinical visit was shown to be of considerable magnitude amounting on average to +27/+14 mmHg for SBP/DBP in a group of 48 hypertensive patients within the first 2–4 min of the visit and being accompanied by a parallel increase in heart rate as shown in (Fig. 1.2) [1–3].
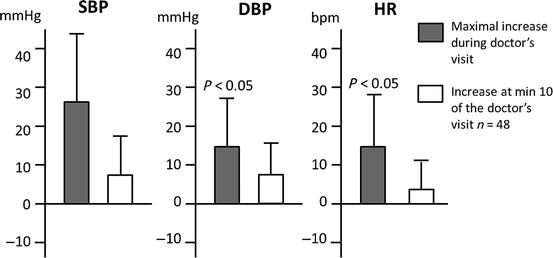
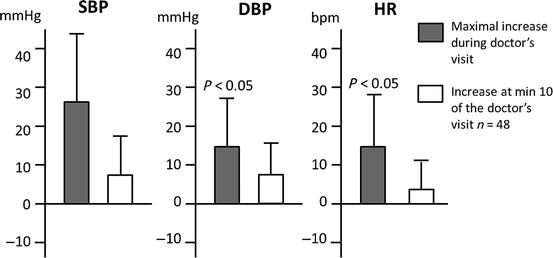
Fig. 1.2
Peak increases in systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) during the doctor’s visit. Data are shown as average values for a group of 48 hypertensive patients (Taken from Mancia et al. [3] with permission)
This phenomenon was correctly interpreted as the hemodynamic response associated with patients’ alerting reaction to the physician’s visit. These findings were further confirmed by means of noninvasive continuous BP monitoring at the finger level showing that WCE, rather than being a research artifact, corresponds to a reproducible phenomenon [10, 11].
These studies also provided evidence that the WCE may characterize not only the period when the patient actually sees the physician but also the entire period spent in a clinic setting.
1.3 Clinic-Ambulatory BP Difference: An Indirect Estimate of the White Coat Effect?
A direct and precise quantification of the pressor reaction to the medical visit is only possible through implementation of beat-to-beat BP recordings in a clinic environment. However, the ethical concerns associated with the invasive nature of intra-arterial BP monitoring and the costs and technical difficulties of noninvasive systems for continuous BP recording at the finger level have prevented their routine use either in a clinical setting or in epidemiological studies.
The introduction of noninvasive techniques for intermittent ambulatory or home BP monitoring in clinical practice and the observation that, in general, office BP levels are higher than BP measured out of the office [1] led to the suggestion that the difference between clinic and mean daytime ambulatory or home blood pressure values might provide an easier, although indirect, assessment of the pressor reaction to the medical visit [4]. This concept was also based on the assumption that out-of-office BP is not influenced by the stressful conditions present in the medical environment and on the evidence provided by previous studies showing that intermittent automated cuff inflations during noninvasive ambulatory BP monitoring do not trigger the alerting reaction and pressure rise induced by a physician’s visit and thus do not overestimate daytime BP values [6]. The difference between clinic and ambulatory BP values was later taken by some authors as a measure of the “white coat effect” (WCE) [4]. This difference was regarded as a possible explanation for the finding of persistently elevated BP levels in the medical environment associated with normal ambulatory BP during daily life, a condition which was thus defined as “white coat hypertension” [4, 8].
Although the use of the clinic-ambulatory BP difference as a measure of the so-called WCE gained popularity in clinical practice, studies comparing direct measures of the “real” WCE (i.e., as assessed by means of continuous, noninvasive BP recordings during a doctor’s visit) with the clinic-ambulatory BP difference have shown limited [12] or even lack of correlation between these measures [10, 13]. Significant discrepancies between these measures were shown in one of these studies, in which clinic-ambulatory BP difference corresponded to less than 30 % of the peak finger beat-by-beat blood pressure increases during the physician’s visit [10], which is in line with the finding of an inverse relationship between [14] the clinic-ambulatory BP difference and the real white coat effect. These reports have raised important concerns regarding the ability of the clinic-ambulatory BP difference to reasonably reflect the patient’s pressor response associated with the alerting reaction during the clinical visit. It is likely that the clinic-ambulatory BP difference may represent a different physiological phenomenon, influenced also by mechanisms other than the alarm reaction to the medical environment. In support of this, the observations from several studies have raised the possibility that variables known to affect daytime BP levels, such as psychosocial, behavioral factors, varying degrees of physical activity, variable wake and sleep time periods, and stressful conditions occurring in daily life, may be more important determinants of the clinic-ambulatory daytime BP difference than the office BP rise due to an alerting reaction triggered by the medical visit [10, 15, 16].
Even from a technical point of view, the discrepancies between direct (real WCE) and indirect (surrogate WCE) measures of the WCE are not at all surprising if we consider that, at variance from continuous BP recordings in a clinic setting, intermittent ambulatory BP measures are not performed in concomitance with the medical visit. Indeed, when the WCE is directly assessed by measures taken before, during, and after the visit of a doctor or a nurse in charge of measuring the BP, the WCE appears to be characterized not only by an increase in BP levels but also by a tachycardic response [1, 3, 17]. In contrast, the clinic-daytime ambulatory BP difference is often not accompanied by any similar difference in heart rate [18]. Furthermore, the real (i.e., directly assessed) WCE has been shown to be independent of the patients age and average clinic BP values [1, 19]; in contrast, the clinic-daytime ambulatory BP difference increases progressively with age and clinic BP values [18, 20] (Fig. 1.3).
Fig. 1.3
Clinic, home, and 24-h average blood pressure and heart rate values in normotensive and untreated hypertensive subjects included in the PAMELA study. Data are shown as average values ± SEM separately for different age decades. S systolic blood pressure, D diastolic blood pressure (Taken from Mancia et al. [18] with permission)
The considerations mentioned above and the poor correlation between measures of the “real” white coat effect (i.e., the BP increase in response to the alerting reaction triggered by the presence of a physician) and its surrogate assessment (i.e., the clinic-ambulatory BP difference) make the term “WCE” inappropriate when referring to the clinic-daytime average BP difference. However, even despite the lack of consistent evidence to support the use of the difference between clinic and daytime blood pressure as a reliable quantitative index of the “real” white coat effect, this difference is currently the most commonly used approach to indirectly quantify the WCE, largely because of the simplicity and feasibility of this approach in clinical practice. Another proposed approach to the indirect assessment of the white coat effect is the quantification of BP levels during the so-called white coat window during 24-h ABPM, i.e., the BP levels recorded during the first and/or last hour of a 24-h ABPM when a subject is in the clinic environment to have to ABPM device applied or removed, respectively [21].
Use of the difference between office and ambulatory BP as an indirect measure of the white coat effect, however, should be considered on the background of its important limitations, mentioned above. The same caution should also apply to the interpretation of the difference between clinic and home BP levels [8].
1.4 White Coat Hypertension (Isolated Clinic Hypertension): Its Assessment from Intermittent ABPM Recordings
The widespread, although somehow improper, adoption of the difference between clinic and mean daytime ambulatory or home blood pressure values as an indirect measure of the “white coat effect” [4] has led to consider the condition characterized by a persistently high BP in the clinic environment associated with a persistently normal BP in daily life as to reflect the persistence over time of an alerting reaction to the physician’s visit. This condition was therefore referred to as “white coat hypertension” [4, 22].
The term WCH was coined under the assumption that the difference between the higher BP values measured in the clinic and the lower values monitored automatically during daytime reflects a pronounced pressor response to the clinic visit and BP measurement procedure in individuals with a normal BP during daily life activities [4, 23]. Indeed, while clinic BP is often affected by the alerting reaction to its measurement by a doctor or a nurse, ambulatory BP data are not influenced by any substantial alerting component in response to automatic or semiautomatic cuff inflations [6]. An exception is represented by the abovementioned reports showing a pronounced rise in BP occurring during the first and/or the last hour of a 24-h ambulatory BP monitoring, when patients are in the hospital environment for fitting or removal of the BP recorder [21, 24].
More in general, use of the term WCH to describe the finding of persistently elevated clinic BP and normal out-of-office BP is inaccurate, because a difference between clinic and ambulatory BP does not necessarily reflect only a white coat effect (as suggested by the reported limited relationship between clinic-ambulatory BP difference and the “real” WCE). It is likely that a high clinic and a normal out-of-office BP may also be generated by factors that lower ambulatory or home BP, such as physical activity or orthostatic hypotension, and not necessarily only by the increase in-office BP due to an alerting reaction to the medical environment.
Besides, the increase in BP levels in response to the medical environment may not be high enough to reach the hypertensive range, so that a given subject may present considerable increase in BP levels during the medical visit without yet being in the hypertensive range. Conversely, hypertensive patients may continue to present a WCE at the time of a doctor’s visit, even if their BP levels are persistently elevated.
The occurrence of the WCE regardless of the presence of hypertension is the reason why WCH should be clearly distinguished from the WCE. While the WCE represents an increase in BP levels during the doctor’s visit, regardless of the usual BP levels of subjects and the administration of antihypertensive treatment, the term “white coat hypertension” should be used to address the condition characterized by persistently elevated BP in the medical environment and by persistently normal daytime ambulatory BP values during daily life in a patient not yet receiving antihypertensive medication [4], although office BP values higher than ambulatory BP may occur independently of a white coat effect [10].
In consideration of all the conceptual concerns mentioned above, the World Health Organization/International Society of Hypertension (WHO/ISH) Guidelines [25, 26] recommended that the condition characterized by persistently elevated clinic or office BP and by persistently normal daytime ambulatory or home BP values should be named “isolated office hypertension” (IOH) or “isolated clinic hypertension” instead of using the appealing, but sometimes misleading, term “white coat hypertension” (Table 1.1).
Table 1.1
Definitions
Alerting reaction | A complex, stereotypical reaction to an emotional, potentially threatening stimulus, characterized in the circulatory system by an increase in blood pressure and heart rate accompanied by vasoconstriction in the skin, splanchnic, and renal circulation and by vasodilation in the skeletal muscle |
White coat effect, direct, “real” (=white coat phenomenon) | Alerting reaction and pressor response of the patient to the measurement of blood pressure in the clinic environment; can be quantified by continuous blood pressure monitoring (invasive or noninvasive) before and during the physician’s visit |
White coat effect, surrogate | Difference between cuff blood pressure measured in physician’s office (clinic blood pressure) and a measurement of blood pressure outside the physician’s office (daytime ambulatory blood pressure, home blood pressure); see the text for its relationship with the direct white coat effect |
Isolated office hypertension (also known as white coat hypertension) | A condition characterized by persistently elevated clinic blood pressure in a patient with normal daytime ambulatory or home blood pressure values; the 1999 WHO/ISH Guidelines suggest using the term “isolated office hypertension” instead of “white coat hypertension” because of a limited or absent correlation of office-daytime or office-home blood pressure differences with the “real” white coat effect |
Despite of this, the term WCH has become the most commonly used term for describing patients with elevated BP in the clinic or office but not in other settings [4, 27]. Moreover, current hypertension guidelines recommend that the term “white coat hypertension” should be reserved to define untreated individuals [9, 27].
When using ABPM or home BP monitoring, white coat hypertension has traditionally been defined as BP levels measured in the office, clinic, or surgery persistently ≥140 mmHg systolic and/or ≥90 mmHg diastolic and persistently normal mean daytime BP levels (i.e., <135/85 mmHg), either on ambulatory or in home BP monitoring [28] (Fig. 1.4).
Fig. 1.4
Schematic relationship between office and home or daytime ambulatory BP in untreated subjects (Adapted from Parati et al. [52] with permission). *Recent ABPM guidelines [9] recommend to compare office BP with 24h rather than with daytime ambulatory blood pressure, when considering these different BP phenotypes, in order not to exclude the role of differences in night-time BP
In consideration of the prevailing prognostic relevance of nighttime blood pressure levels over other components of ABPM, current ESH/ESC guidelines for hypertension management [27] and guidelines for ABPM [9] have expanded the definition of white coat hypertension, requiring normality not only in awake BP values but also in 24-h (i.e., <130/80 mmHg) and sleep BP levels (i.e., <120/70 mmHg) (see Box 1.1).
Box 1.1. Defining Criteria for White Coat Hypertension
Untreated patients with elevated office blood pressure ≥140/90 mmHga |
24-h ambulatory blood pressure measurement <130/80 mmHg |
Awake ambulatory blood pressure measurement <135/85 mmHg |
Sleep measurement <120/70 mmHg or |
Home blood pressure <135/85 mmHg |
1.5 Prevalence of WCH
Although WCH (or IOH) has been shown to be reasonably reproducible when properly studied with OBP measurements along with real-life ABPM [29], the prevalence reported in literature for WCH has been widely variable and inconsistent, ranging from less than 10 % [18] to more than 60 % [30] with several intermediate values [9, 31, 32].
These important discrepancies might have been the result of the varying demographic features of the populations being surveyed as well as the different threshold values employed for the definition of white coat hypertension in these studies [9, 31, 32]. The first reports on the frequency of white coat hypertension, considering a threshold value of 140/90 mmHg as the upper limit of normality for both office and daytime ambulatory BP levels, found WCH to be present in as much as 60 % of the overall hypertensive population [30, 33]. However, after the evidence provided by the PAMELA study [18] and other population studies [34, 35] and meta-analyses [36] supporting a threshold value <130/85 mmHg as the upper limit of daytime ambulatory BP normality, the frequency of this phenomenon was found to be significantly lower. Indeed, the prevalence of white coat hypertension in subsequent studies was reported to range from 9 to 16 % in the general population (average 13 %) and from 25 to 46 % (average about 32 %) among hypertensive subjects [9, 18, 31, 32, 37].
Although the prevalence of WCH continues to be widely variable in different studies, available reports strongly emphasize that this condition is rather common, irrespective of whether out-of-office BP is measured by home or ambulatory BP criteria [38].
Many of the studies addressing the prevalence of WCH have also comparatively explored demographic and clinical characteristics of patients with WCH vs. those of patients with sustained hypertension and of normotensive controls, in an attempt to identify potential predictive factors for this condition.
In these studies, the frequency of WCH has been shown to increase in the presence of certain clinical characteristics, such as office systolic (S)BP in the range of 140–159 mmHg or diastolic (D)BP in the range of 90–99 mmHg, female sex, increasing age, non-smoking status, hypertension of recent diagnosis, limited number of BP measurements in the doctor’s office, and normal left ventricular mass at echocardiography [4, 32, 39]. The prevalence has been shown to be lower in the case of documented target organ damage or when office BP is based on repeated measurements or when measured by a nurse or another healthcare provider [32].
Regarding demographic variables, age has been shown to be a stronger predictor of WCH than either gender or ethnicity, based on the fact that the relationship of age with clinic BP is much steeper than with ambulatory or home readings [40].
In relation to BP levels, the prevalence of WCH has been shown to be more common among patients with the mildest hypertension (i.e., SBP/DBP 140/90–159/99 mmHg) and virtually nonexistent among those with the most severe hypertension (i.e., above 210/120 mmHg) [22, 23, 41–43]. The analysis of a large international database including performance of ABPM in 7,069 subjects who were initially diagnosed as either normotensive or hypertensive based on conventional office BP measurements showed the prevalence of WCH to be inversely correlated to the level of office BP. While the percentage of white coat hypertension amounted to about 55 % in grade 1 hypertension, it may correspond to only 10 % in grade 3 hypertensive subjects [43]. Similar results were reported in an analysis of the Progetto Ipertensione Umbria Monitoraggio Ambulatoriale (PIUMA) study in 1,333 untreated subjects with essential hypertension in whom the prevalence of WCH markedly decreased with increasing severity of hypertension. When classifying subjects according to the Joint National Committee V classification criteria, the prevalence of white coat hypertension was 33.3 % in stage I (systolic 140–159 mmHg or diastolic BP 90–99 mmHg), 11.8 % in stage II (systolic 160–179 mmHg or diastolic BP 100–109 mmHg), and 3 % in stage III hypertension (systolic ≥180 mmHg or diastolic BP ≥110 mmHg) [22] (Fig. 1.5).