Fig. 5.1
Manifestations of subclinical cardiac organ damage related to hypertension: the association between left ventricular hypertrophy (LVH, upper panel) and diastolic dysfunction (lower panel)
Several methods characterized by different diagnostic sensitivity and specificity, namely, electrocardiography, chest X-ray, echocardiography, and magnetic resonance imaging, are available for LVH detection. Standard ECG at rest is largely available in clinical practice due to its simplicity and low cost; its sensitivity, however, is relatively low [19]. Among noninvasive methods evaluating cardiac anatomy and function in hypertensive patients, echocardiography is the most widely used. The advantages of this procedure include high sensitivity/specificity, large availability, absence of biological harmful effects, excellent tolerability, and lower cost compared with techniques of similar accuracy. Echocardiographic prevalence of LVH in hypertension depends mostly on demographic and clinical variables and partly on cutoff values applied. Although the pathogenesis of hypertensive LVH is not fully understood, a consistent body of evidence indicates that the severity of pressure overload, as better reflected by out-of-office than in-office BP levels, in combination with non-hemodynamic variables, including genetic, ethnical, and humoral factors, plays a pivotal role in its development [20]. A number of echocardiographic studies performed in different clinical settings (i.e., hypertension clinics, primary care, pediatric setting, and population-based cohorts) explored the association between ICH and subclinical cardiac damage in terms of LVH and/or LV concentric remodeling. Most studies focused their attention on untreated subjects with ICH, but other reports investigated the impact of this condition in patients on antihypertensive drugs.
In a pioneering investigation by Haegholm et al. including a total of 143 patients with newly diagnosed mild-to-moderate hypertension (53 with ICH as defined by daytime ambulatory DBP <90 mmHg), LV mass index was higher in the group with established hypertension compared to ICH group (102 ± 27 g/m2 versus 94 ± 23 g/m2, p = 0.04) [21]. This was also the case for LV relative wall thickness, an index of LV concentric geometry (0.36 ± 0.07 versus 0.33 ± 0.06, p = 0.004). Of note, LV geometry and structure was normal in up to 83 % ICH patients as compared to 61 % established hypertensives. Left atrial dimensions were not different between the groups. In a multiple regression model, ambulatory BP values but not office BP values were significantly associated with the extent of cardiac hypertrophy. In a subsequent study conducted at the New York Hospital-Cornell Medical Center by Devereux’s group, the authors compared echocardiographic data of LV structure and function in 24 untreated individuals with ICH (i.e., ambulatory awake BP <134/90 mmHg) with those of sustained hypertensive and normotensive subjects matched for age and gender [22]. Absolute LV mass, LV mass indexed either to body surface area or height2.7, and wall thicknesses were higher in sustained hypertensives than in ICH and normotensive subjects. Prevalence of LVH (i.e., LV mass index >125/110 g/m2) was higher in sustained hypertensives than in normotensives (25 % versus 0 %, p < 0.01); the difference with ICH group (4 %) did not reach the statistical significance. LV systolic function and hemodynamic parameters including cardiac output were similar in the three groups. Ourselves, examining a group of 82 untreated patients with mild essential hypertension, 51 of them with established hypertension and 31 with ICH (average 24-h BP <132/85 mmHg), we found that the prevalence of LVH (LV mass index ≥125/110 g/m2) and/or LV concentric remodeling was higher in the former (51 %) compared to the latter (19 %) group [23]. In the Hypertension and Ambulatory Recording Venetia Study (HARVEST) carried out in 942 young participants with untreated borderline or mild hypertension who underwent 24-h ambulatory BP monitoring, early cardiac involvement was detected in 722 subjects with reliable echocardiographic data [24]. Ninety-five normotensive subjects with similar age and sex distribution were studied as controls; ICH was defined on the basis of two thresholds of daytime BP (i.e., <130/80 mmHg and <135/85 mmHg): LV mass index and LV wall thickness in ICH subjects (irrespective of the ambulatory BP criteria used to define this condition) turned out to be smaller than in sustained hypertensives but greater than in normotensive subjects. Relative wall thickness in normotensive subjects was lower than in both hypertensive groups, and this parameter was not different between sustained hypertensives and ICH subjects. Of note, LV systolic function and diastolic filling parameters were similar among the three groups either for unadjusted or adjusted data. Among 345 adult patients with untreated mild hypertension (39 % with ICH) attending a primary care setting, LV mass index was higher in women with sustained hypertension as compared to the ICH counterparts (108 ± 19 g/m2 versus 99 ± 19 g/m2, p < 0.05); the same was not true for male gender (125 ± 27 g/m2 versus 122 ± 28 g/m2 p = ns, respectively) [25]. As for LV relative wall thickness, no difference was found between genders. In the Pressioni Arteriose Monitorate E Loro Associazioni (PAMELA) study, ICH prevalence in a population subsample of untreated adult and elderly individuals ranged from 9 to 12 %, depending on whether out-of-office BP was defined by ambulatory (24-h <125/80 mmHg) or home (<135/85 mmHg) BP values [3]. In subjects with ICH, LV mass index and wall thickness were on average lower than in hypertensives with both office and ambulatory or home monitoring but higher than in normotensives with normal office, ambulatory, or home BP values. Similar findings were obtained when data were separately analyzed in men and women and adjusted for age. Furthermore, in these individuals LVH was less frequent (15–18 %) than in subjects with both office and daytime hypertension (23–26 %) but more frequent than in sustained normotensives (4 %) (Fig. 5.2).
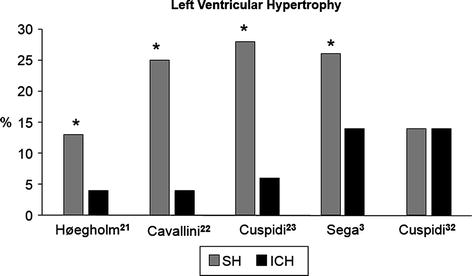
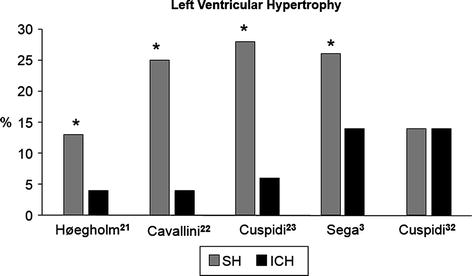
Fig. 5.2
Prevalence rates of echocardiographic left ventricular hypertrophy (LVH) in subjects with isolated clinic hypertension (ICH) and in subjects with sustained hypertension (SH) as reported in five studies (* means P at least <0.05)
Less information is available regarding the relevance of ICH (the white coat effect) in terms of extent of organ damage in treated hypertensives compared to hypertensives with sustained controlled office and ambulatory BP. In a previous study, we assessed LV structure in 33 treated hypertensives with good BP control at home or during ambulatory BP monitoring but elevated office BP values and in 35 age- and sex-matched hypertensives with good BP control in- and out-office [26]. As compared to patients with fully controlled hypertension, those with BP control only at home (<132/82 mmHg) or during ambulatory monitoring (average 24-h BP <125/80 mmHg) exhibited a higher prevalence of LVH, as defined by LV mass index >134/110 m2 (15.1 % versus 2.8 %). Salles et al. investigated the role of uncontrolled ICH as an independent risk factor for LVH in a cohort of treated hypertensives with type 2 diabetes by comparing echocardiographic findings in 172 patients with ICH (average 24-h BP <130/80 mmHg) and in 152 patients with controlled office and ambulatory hypertension [27]. The authors found that LV mass index was higher (62 ± 22 g/m2.7 versus 53 ± 17 g/m2.7, p < 0.001) and LVH (LV mass index >48/44 g/m2.7) was more prevalent (77 % versus 60 %, p = 0.02) in ICH than controlled group. A study including both untreated and treated (72 %) subjects compared echocardiographic indices of LV structure in three groups characterized by masked ICH (mean daytime BP <135/85 mmHg) and sustained hypertension and showed that LV mass index was significantly lower in ICH than in the other two groups [28]. In particular, prevalence rates of LVH (i.e., LV mass index >125/110 g/ m2) were 33 % in ICH, 48 % in masked, and 67 % in sustained hypertension.
Little is known about the clinical significance and natural history of ICH in children. In a study aimed to evaluate target organ damage in children with ICH, Lande et al. assessed LV mass index in 27 subjects with ICH, in 27 matched normotensive and 27 hypertensive controls [29]. Each ICH subject was matched by body mass index (±10 %), age (±1 year), and sex to a normotensive and hypertensive control. Mean LV mass index was 29 g/m2.7, 32 g/m2.7, and 35 g/m2.7 in normotensive, ICH, and sustained hypertensive children, respectively (normotensives versus ICH, p = 0.03; ICH versus sustained hypertensives, p = 0.07). LVH (defined as LV mass index ≥ the 95th percentile, namely, 39.4 g/m2.7 for boys and 36.9 g/m2.7 for girls) was absent in all subjects of the normotensive and ICH group, but was present in 26 % of sustained hypertensives (p < 0.001). No difference in LV structure was observed by Pall et al. when echocardiographic data were compared in 59 normotensive and 50 ICH adolescents (LV mass index 35 g/m and 38 g/m respectively, p = 0.87).
It is worth noting that in the abovementioned studies ICH was defined according to a single ambulatory BP monitoring session. Unfortunately, this approach has relevant limitations: first, ambulatory BP although more reproducible than clinic BP may vary from one recording session to another due to variations in environmental stimuli, physical activity, and duration and quality of sleep. Secondly, ICH patients may have different degrees of organ damage, thereby accounting for the conflicting data published in the literature. These limitations have been recognized by the 2013 European Society Hypertension/European Society Cardiology (ESH/ESC) guidelines which recommend that subjects with ICH should have the diagnosis confirmed by periodical out-of-office measurements [9]. Unfortunately, the reproducibility of the ICH classification has been evaluated in a limited number of studies.
In the HARVEST study, this issue and its relationship with cardiac organ damage has been investigated by Palatini et al. in 565 subjects aged 18–45 years with grade 1 hypertension and in 95 normotensive individuals by repeating an ambulatory BP monitoring within a 3-month interval [31]. From the first ambulatory BP monitoring, 90 hypertensive subjects were classified as having ICH (mean daytime <130/80 mmHg): in these subjects, 24-h BP was similar as in normotensives, but LV mass index was greater than in the normotensive group. After the second ambulatory BP monitoring, only 38 out of 90 subjects (42.2 %) had a reproducible ICH pattern, the remaining 52 subjects having only a minor increase in 24-h BP above the normal limits. LVMI in the 38 subjects with ICH on both recordings was greater than in normotensive subjects and similar as in 52 subjects with not reproducible ICH. These results show that ICH is not a stable condition and that more than 50 % of ICH subjects identified by the first BP monitoring have sustained hypertension after a second ambulatory BP monitoring. It should be pointed out that these findings pertain to a selected sample of young subjects (mean age 32 years) with recently diagnosed hypertension and should not be generalized to the hypertensive population.
In order to overcome these limitations, our group examined the reproducibility of ICH by performing two 24-h ambulatory BP monitoring at 1–4 week interval and evaluated its impact on cardiac organ damage in a population with a broader range of age (17–79 years, mean age 46 years) and hypertension values (40 % with grade 2 hypertension) than previous studies [32]. As many as 46 % of patients labeled as having ICH after the first ambulatory BP monitoring had mean daytime BP >135 mmHg systolic or 85 mmHg diastolic at the second ambulatory BP monitoring, thereby showing a not reproducible ICH pattern. When ICH was identified by lower ambulatory cutoff values, i.e., mean 24-h BP <125 mmHg systolic or 80 mmHg diastolic or daytime BP <130 mmHg systolic or 80 mmHg diastolic, even higher portions of patients shifted to sustained hypertension after the second ABPM (54 and 66 %, respectively). LV mass index was higher in patients with not reproducible than in those with reproducible ICH. These findings show that (1) classification of ICH on the basis of a single ambulatory BP monitoring has a limited short-term reproducibility and (2) a reproducible and not reproducible ICH pattern may have different cardiovascular risk profiles.
Figure 5.3 reports the results of the meta-analysis from six studies [3, 21–24, 32] providing data on average LV mass indexed to body surface area and SD in sustained hypertensive and ICH subjects. The standardized difference in means (SMD) was positive in favor of sustained hypertensives (0.38, 95 % CI 0.27–0.50, p < 0.01). The findings of the meta-analysis from six studies in ICH and normotensive controls are shown in Fig. 5.4. In this comparison the SMD was positive in favor of ICH subjects (0.43, 95 % CI 0.11–0.74, p < 0.01).
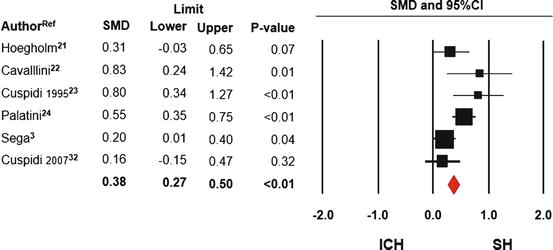
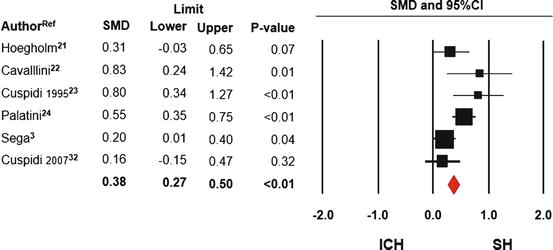
Fig. 5.3
Forest plot for standardized mean difference (SMD) and 95 % confidence intervals (CI) of left ventricular mass index (gr/m2) between patients with sustained hypertension (SH) and isolated clinic hypertension (ICH). Meta-analysis from six studies, fixed model
Fig. 5.4
Forest plot for standardized mean difference (SMD) and 95 % confidence intervals (CI) of left ventricular mass index (gr/m2) between normotensive subjects (NT) and patients with isolated clinic hypertension (ICH). Meta-analysis of six studies, random model (I 2 = 84.1)
5.3 ICH and Carotid Damage
The noninvasive evaluation of carotid artery structure is increasingly implemented in epidemiologic studies and interventional trials. The measurement of intima-media thickness (IMT) and the assessment of the presence of plaques and stenosis provide a reliable, quantitative index of atherosclerotic damage. As a consequence, ultrasonic assessment of the carotid artery structure has attracted considerable interest and is currently applied either in the clinical as in the research field. Since the mid-1980s when the pioneering studies by Pignoli et al. [33] investigated the correlation of ultrasonic interfaces with anatomical components of the carotid wall, hundreds of cross-sectional and longitudinal studies have assessed the prevalence of carotid atherosclerosis, its association with risk factors and incident cardiovascular disease [34, 35]. Numerous studies have consistently shown an association between carotid IMT and traditional risk factors, subclinical organ damage such as LVH, cerebral white matter lesions, peripheral arterial atherosclerosis, microalbuminuria, coronary calcifications, and, more importantly, overt CV diseases [36–38]. In particular, hypertension has been demonstrated to be the major risk factor for carotid IM thickening and plaque progression, due to the synergistic effect of mechanical stress on the arterial wall and the growth/inflammatory factors operating in hypertension [39]. Since the mid-1990s, a number of prospective trials performed in population-based samples and selected cohorts of individuals at high risk, such as the Atherosclerotic Risk in Communities (ARIC) [40], the Rotterdam Study [41], the Cardiovascular Health Study (CHS) [7], the European Lacidipine Study on Atherosclerosis (ELSA) [42], and the Carotid Atherosclerosis Progression Study (CAPS) [43], reported that carotid IMT and/or plaques are strong predictors of coronary events and stroke. These findings have been recently reinforced by larger prospective studies. Among 6,257 people aged 25–84 years who participated in a population-based study, the Tromsø study, the risk of myocardial infarction during a mean 15-year follow-up period was found to increase significantly across the quartiles of mean IMT (P for trend <0.001) and total plaque area (P for trend <0.001) [44]. The results of the IMPROVE study, a multicenter observational European trial carried out in 4,482 subjects with 3 or more vascular risk factors, showed that progression of carotid IMT over a median follow-up period of 21.5 months was an independent predictor of subsequent vascular events [45]. Thus, available information supports the view that carotid IMT is a valuable surrogate end point for assessing subclinical organ damage in different clinical conditions. A significant increase in IMT has been reported by several studies in patients with various degrees of hypertension compared with age-matched normotensive controls, after adjustment for confounding variables. Relatively few reports, however, addressed this issue in ICH. The first study providing some evidence on the carotid artery structure in ICH was published in the early 1990s by Cavallini et al. who compared echocardiographic and carotid ultrasonographic findings in true normotensive (n = 24, mean age 58 ± 8 years), in ICH (n = 24, mean age 61 ± 9 years), and in sustained hypertensive patients (mean age 61 ± 10 years) [22]. Common IMT was greater in sustained hypertensives (0.98 mm) than in ICH (0.84 mm, p < 0.05) and normotensive group (0.76 mm, p < 0.001). The prevalence of atherosclerotic plaques (defined as presence of discrete plaques at least greater than the surrounding wall in any segment of the arteries) was similar in ICH (25 %) as in normotensive (21 %) group and higher in sustained hypertensives (58 %, p < 0.05) (Fig. 5.5). According to these results, the authors concluded that sustained rather than episodic BP elevation is important in producing preclinical disease of the arterial tree; thus, ICH may be regarded as a benign condition. A significant difference in terms of carotid IMT and plaques area between sustained hypertensives and ICH patients was also reported in an early study by our group carried out in a sample of 82 untreated individuals (mean age 44 ± 11 years) [23]. Common carotid artery IMT (average of both the right and left side) was higher in sustained hypertensives (0.68 mm) than in ICH subjects (0.58 mm, p < 0.001). At difference from data provided by Cavallini et al., carotid plaques were similarly prevalent among ICH (11 %) and sustained hypertensive (13 %). Pierdomenico et al. assessed carotid structural parameters in 50 sustained hypertensives, 25 ICH and 25 normotensive controls [46]. Compared with sustained hypertensives, ICH group had lower values of IMT (0.85 ± 0.18 versus 0.71 ± 0.15 mm, p < 0.05) and IM thickening (28 % versus 4 %, p < 0.01); no significant difference in these parameters was observed between ICH patients and normotensive controls.
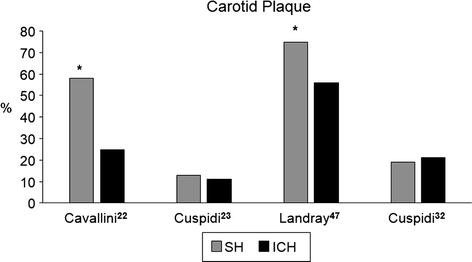
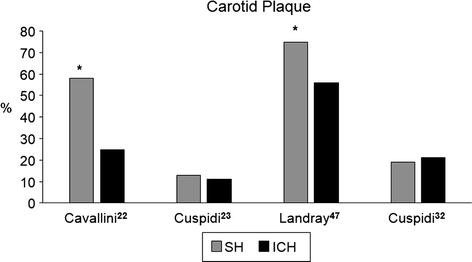
Fig. 5.5
Prevalence rates of carotid plaque in subjects with isolated clinic hypertension (ICH) and in subjects with sustained hypertension (SH) as reported in four studies (* means p at least <0.05)
Landray et al. analyzed the relationship between office and out-of office BP (assessed by ambulatory BP monitoring) and atherosclerotic vascular disease in a sample of 79 individuals categorized as true normotensive, ICH, and sustained hypertensives [47]. The authors found that the prevalence of carotid plaque was lower in normotensive (53 %) and ICH subjects (56 %) as compared to sustained hypertensives (75 %). In contrast, significantly greater IMT values were documented by Zakopoulos et al. in 22 ICH (0.68 ± 0.14 mm) and 41 sustained hypertensive subjects (0.67 ± 0.18 mm) compared to 17 normotensive controls (0.50 ± 0.09 mm, p < 0.001) [48]. Nakashima et al. compared IMT values in 30 ICH, 30 untreated sustained hypertensives, and 30 normotensive subjects without evidence of carotid plaque matched for age/gender. IMT and carotid cross-sectional areas were similar in patients with ICH and sustained hypertension and significantly higher than in normotensive subjects [49]. Among 74 never-treated grade I hypertensive subjects and 20 normotensive control subjects, Puato et al. measured carotid wall as mean IMT and maximum IMT at baseline and after a 5-year follow-up in order to define the rate of IMT increment and the potential role of various risk factors, including office and ambulatory BP [50]. During the follow-up, mean IMT and mean of maximum IMT increased to a greater degree in ICH subjects (n = 35) and sustained hypertensives (n = 39) than in normotensive controls. No differences were found between ICH and sustained hypertensive subjects for both mean IMT and maximum IMT. These findings indicate that IMT in ICH subjects grows faster than in normotensives and to a similar extent as in sustained hypertensive patients. Among 274 subjects with ICH attending an outpatient hypertension clinic in Greece, average carotid IMT value tended to be higher than in sustained normotensive controls, although the difference was not significant (0.67 ± 0.15 versus 0.63 ± 0.15 mm) [51]. A cross-sectional survey of 2,915 community-dwelling Japanese aged ≥40 years investigated the relationship between carotid atherosclerosis and BP patterns defined on the basis of combined measurements of office blood pressure and home blood BP [52]. Geometric average of mean IMT was higher among subjects with ICH (0.73 mm), masked hypertension (0.77 mm), and sustained hypertension (0.77 mm) compared to normotensives (0.67 mm; p < 0.001 for all). All types of hypertension were also associated with an increased likelihood of carotid stenosis as compared with normotensives (age- and sex-adjusted odds ratio, 2.36, 95%CI: 1.27–4.37 for ICH; 1.95, 95%CI: 1.25–3.03 for masked hypertension; and 3.02, 95%CI: 2.01–4.54 for sustained hypertension). These associations remained significant even after adjustment for other cardiovascular risk factors.
Conflicting results have been also reported in the pediatric setting. Pall et al. showed that IMT was higher both in ICH and sustained hypertensives compared with healthy normotensive individuals (controls: 0.48 ± 0.1 mm, ICH: 0.56 ± 0.1 mm, sustained hypertension: 0.54 ± 0.1 mm, both p < 0.001 compared with controls) [30]. No significant difference was found between the hypertensive groups. On the contrary, similar average IMT values were reported by Stabouli et al. in true normotensive, ICH, masked, and sustained hypertensive children [53].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree