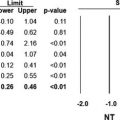
Fig. 3.1
Plots showing mean arterial pressure (MAP), heart rate (HR) and muscle sympathetic nerve activity (MSNA) in normotensive (NT), moderate hypertensive (MH), and severe essential hypertensive (EH) subjects. Data are shown as means ± SEM. Asterisks (** P < 0.01) refer to the statistical significance between groups (Unpublished figure drawn using data from Ref. [5])
Additional information on the sympathetic activation characterizing essential hypertension obtained in the past few years can be summarized as follows. First, the adrenergic overdrive of the essential hypertensive state is widespread to the whole cardiovascular system, an increase in norepinephrine spillover (a parameter reflecting the secretion of the neurotransmitter from adrenergic nerve terminals) being detectable at the level of the cerebral, coronary, and renal circulation as well [6]. Second, in the majority of the studies published so far, the hyperadrenergic state appears to be peculiar of essential hypertension, no sympathetic activation being detectable in secondary hypertensive states [1, 5]. Third, multiple and still largely undefined are the factors responsible for the onset of the sympathetic stimulation, although alterations in reflex cardiovascular control and metabolic influences (such as hyperinsulinemia and the related insulin resistance, renin-angiotensin-aldosterone activation, hyperleptinemia, etc.) are likely to play a role [1]. Finally, cross-sectional and longitudinal evidence indicate that sympathetic neural influences participate at the development and progression of the cardiovascular structural and functional changes associated with the high blood pressure state. This has been specifically shown for left ventricular hypertrophy and left ventricular diastolic dysfunction [7, 8]. This has been also shown for arterial stiffness and arterial and arteriolar vascular hypertrophy [9]. This has been finally shown for microalbuminuria and impaired renal function [10].
3.3 Neurogenic Mechanisms and the “White-Coat” Effect
As already mentioned in other chapters of the book, the term “white-coat” effect refers to the marked pressor and tachycardic responses that can be triggered in a consistent number of subjects by the doctor when assessing sphygmomanometric blood pressure values [11]. For several years, it was thought that these hemodynamic changes were dependent on an alerting reaction triggered by the doctor in the process of measuring clinic blood pressure values, resembling a stressful condition eliciting a sympathetic stimulation. Only in recent years, however, it became clear that the abovementioned hemodynamic alterations may be accompanied to, and presumably triggered by, profound changes in regional sympathetic neural drive. This demonstration came from a study carried out by our group in which we quantified in patients with newly discovered hypertension the “white-coat” effect not only on blood pressure and heart rate but also on sympathetic neural outflow to the muscle and the skin circulation as assessed by the microneurographic technique [12]. What we did was to examine whether and to what extent muscle and skin sympathetic nerve traffic, which are regulated as shown in Fig. 3.2 by different mechanisms, are affected by the sphygmomanometric assessment of clinic blood pressure by a doctor. Figures 3.3 and 3.4 show the main study results. As expected sphygmomanometric blood pressure measurement by a doctor elicited a sudden marked increase in blood pressure (recorded on a beat-to-beat basis via a Finapres device) which was associated with a tachycardic response. These hemodynamic changes were accompanied by a decrease in muscle sympathetic nerve traffic, amounting on average to 27 %, and by a marked increase (+73 %) in skin sympathetic nerve traffic. Interestingly, all the abovementioned hemodynamic and neural changes persisted throughout the 10 min doctor visit and showed, with the exception of the skin neural component, a slow rate of disappearance (Fig. 3.4). It thus appears that the emotional reaction known as “white-coat” effect is characterized by a behavior of the sympathetic nervous system that combines a skin sympathetic activation (and a resulting vasoconstriction ) with a muscle sympathetic deactivation leading to muscle vasodilation. This heterogeneous neural behavior appears to be a peculiar feature of the human responses to emotional stimuli , which are characterized by a generalized vasoconstriction in different vascular districts (including the cutaneous one) except the skeletal muscle, in which a profound vasodilation has been reported [13].
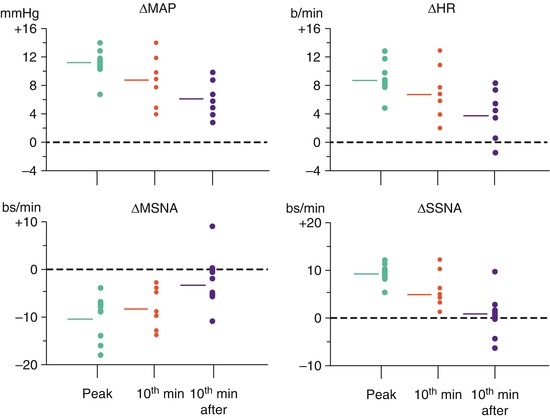
Fig. 3.2
Schematic drawing illustrating the factors modulating muscle and skin sympathetic activity. Reflex influences stemming from the carotid and aortic bodies, receptors located within the cardiac chambers, and muscle metaboreceptors as well as metabolic and humoral factors contribute to the regulation of muscle sympathetic nerve traffic (left panel), while emotional factors and thermal and respiratory stimuli modulate skin sympathetic nerve traffic (right panel). Ag II angiotensin II, ANP atrial natriuretic peptide, ADH vasopressin, ET endothelins
Fig. 3.3
Effects of sphygmomanometric blood pressure measurement by a doctor (doctor visit) on mean arterial pressure (MAP), muscle sympathetic nerve traffic (MSNA), and skin sympathetic nerve traffic (SSNA). Data are shown as mean ± SEM changes as compared to the pre-visit values. Note the marked pressor response associated with a sustained increase in SSNA and a pronounced reduction in MSNA. Asterisks (* P < 0.05) refer to the statistical significance between single values obtained during doctor visit and pre-visit values (Unpublished figure drawn using data from Ref. [12])
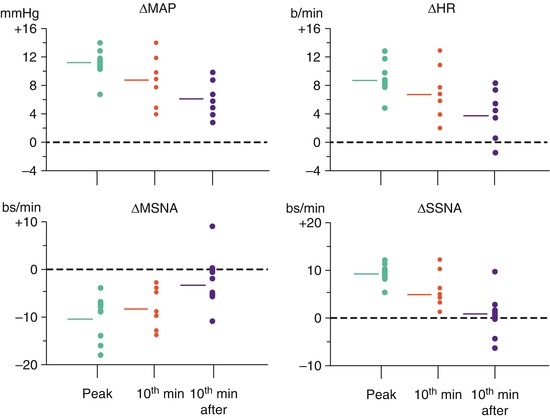
Fig. 3.4
Changes in mean arterial pressure (MAP), heart rate (HR), muscle sympathetic nerve activity (MSNA), and skin sympathetic nerve activity (SSNA) observed in the first 2 min (peak), at the 10th minute of the doctor visit (10th minute) and after 10th minute from the visit end (10th minute after). Data are shown as individual data (circles) and as average values (horizontal lines in each panel). B/min beats per minute, bs/min bursts per minute (Unpublished figure drawn using data from Ref. [12])
A further set of data our group has collected throughout the years on the involvement of sympathetic neural factors in the “white-coat” effect concerns the behavior of the hemodynamic and sympathetic nerve traffic responses to blood pressure measurements performed by a nurse. The hypothesis tested in these studies was that the alerting reaction should be markedly attenuated by a nurse as compared to a physician, given the greater emotional impact on the patients physicians have as compared to nurses. In the first study we compared the blood pressure and heart rate responses to the doctor’s and nurse’s sphygmomanometric blood pressure measurement in a group of 16 normotensive or hypertensive subjects who underwent intra-arterial recording of blood pressure via the Oxford technique [14]. By evaluating the intra-arterial blood pressure responses, we found that the nurse elicited a markedly less pronounced pressor response as compared to the one triggered by the doctor, with a parallel attenuation of the tachycardia observed during the doctor visit. In a recent study in which we made use of an experimental design similar to the one just mentioned, we were able to show that the attenuation of hemodynamic responses characterizing the alerting reaction by the nurse had as “neurogenic” counterpart a consistent reduction in the magnitude of the muscle sympathoinhibitory and skin sympathoexcitatory responses to the doctor’s blood pressure measurement (Fig. 3.5) [15]. This finding provides further support to the hypothesis that neurogenic mechanisms are responsible in large part for the hemodynamic responses characterizing the “white-coat” effect.
Fig. 3.5




Changes in mean arterial pressure (MAP), heart rate (HR), muscle sympathetic nerve activity (MSNA), and skin sympathetic nerve activity (SSNA) observed during doctor (white bars) or nurse (black bars) blood pressure measurement. Data are shown as mean ± SEM changes as compared to the pre-visit values. Asterisks (* P < 0.05) refer to the statistical significance between doctor and nurse responses. Note the marked attenuation of the responses during nurse blood pressure assessment. B/min beats per minute, bs/min bursts per minute (Unpublished figure drawn using data from Ref. [12])
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree