Abstract
Breast cancer can rarely present as isolated axillary adenopathy without any evidence of a primary breast mass creating many diagnostic and therapeutic challenges. Occult breast cancer is defined as isolated axillary adenocarcinoma without detectable tumor in the breast by either physical examination or with imaging such as mammogram, ultrasound, or MRI. Occult breast cancer, although rare, has been acknowledged for more than 100 years. It was first described by Halsted in the Annuals of Surgery in 1906.
Keywords
occult breast cancer, axillary lymph node, PET, MRI, chemotherapy
Breast cancer can rarely present as isolated axillary adenopathy without any evidence of a primary breast mass creating many diagnostic and therapeutic challenges. Occult breast cancer is defined as isolated axillary adenocarcinoma without detectable tumor in the breast by either physical examination or with imaging such as mammogram, ultrasound, or magnetic resonance imaging (MRI). Occult breast cancer, although rare, has been acknowledged for more than 100 years. It was first described by Halsted in the Annuals of Surgery in 1906.
Incidence
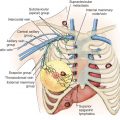
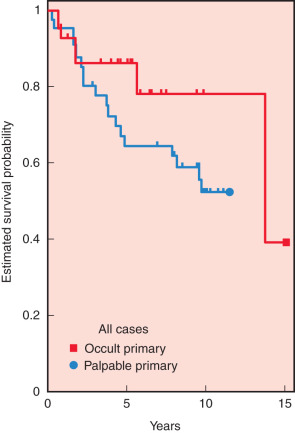
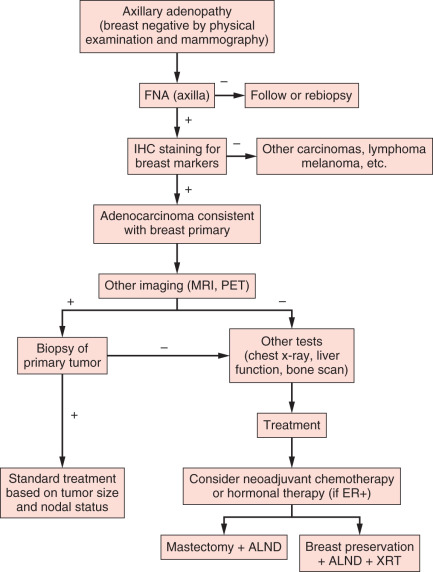
Occult breast cancer with axillary metastasis is rare and likely accounts for less than 1% of all newly diagnosed breast cancers ( Fig. 79.1 ). It is difficult to determine the exact incidence because the case series are small and imaging techniques have improved. With improving sensitivity of breast imaging, including the addition of MRI imaging, it is a reasonable assumption that more primary breast lesions will be identified before surgery.
Diagnosis
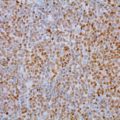
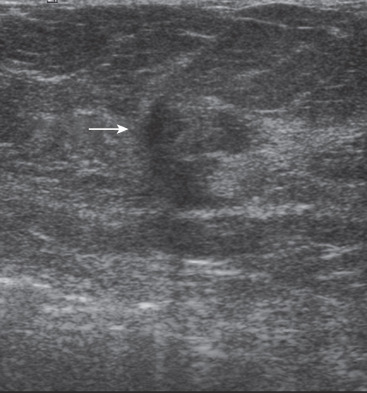
The majority of patients presenting with isolated axillary adenopathy will subsequently be diagnosed with benign reactive adenopathy ( Fig. 79.2 ). Within the setting of malignancy, lymphoma is a more common cause of isolated axillary adenopathy than an occult breast cancer. Other cancers that can present as occult metastatic disease include lung, colon, gastric, and melanoma. In one recent study, the pathology was reviewed for 65 patients who presented with isolated axillary lymph node swelling between 2005 and 2011 and subsequently had an axillary lymph node excisional biopsy. Only 24% (16) of the biopsies were malignant, and of the malignant biopsies, 10 were consistent with a breast primary.
Selected Imaging
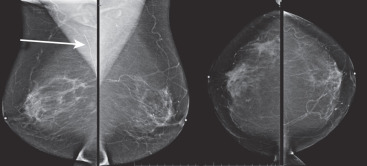
Diagnostic workup generally starts with a core needle biopsy of the axillary node consistent with adenocarcinoma or carcinoma not otherwise specified ( Fig. 79.3 ). On the basis of current National Comprehensive Cancer Network (NCCN) guidelines, mammography should be the first imaging study ( Fig. 79.4 ). A nonpalpable breast mass may be successfully identified with mammography in approximately 10% to 20% of cases. However, small tumor size and high breast density can lead to false-negative findings on mammography. In one small case series, mammogram was able to detect a primary breast mass in 10 of 17 patients presenting with axillary adenopathy and a clinically normal breast examination. If mammography is nondiagnostic, then ultrasound and MRI of the breast are indicated ( Fig. 79.5 ). Systemic imaging should include computed tomography (CT) scans of the neck, chest, and abdomen. A bone scan should be considered in patients with elevated alkaline phosphatase or if they have symptoms concerning for bone lesions.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree