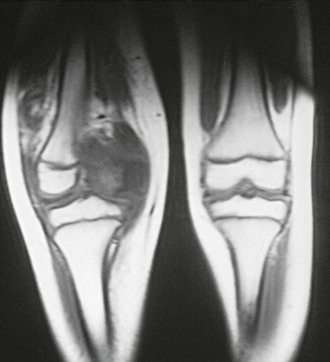
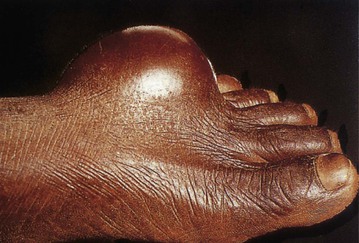
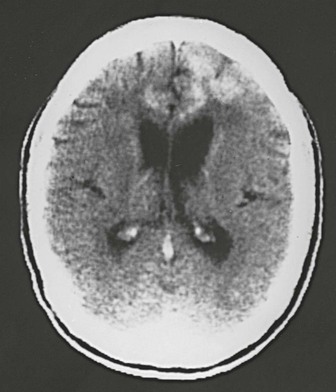
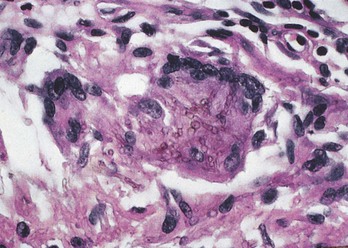
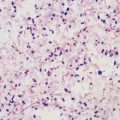
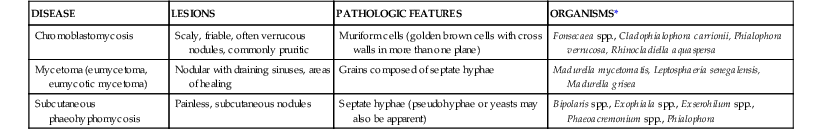
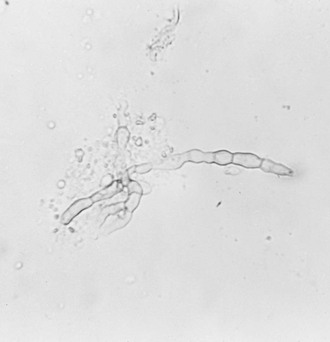
Duane R. Hospenthal In humans, infection with Pseudallescheria boydii* (Scedosporium apiospermum) can produce two distinct diseases: mycetoma and pseudallescheriasis (scedosporiosis). Mycetoma is a chronic subcutaneous infection characterized by the production of grains (see Chapter 263), whereas pseudallescheriasis includes all other infections caused by P. boydii. The most common sites of pseudallescheriasis are lung, bone, joints, and the central nervous system (CNS).2,3 Sinusitis, keratitis, endophthalmitis, skin and soft tissue infections, prostatitis, and endocarditis have also been described. The fungus is found in soil and fresh water, especially stagnant or polluted water, throughout the world. Disease is acquired after inhalation of this organism into the lungs or paranasal sinuses or after traumatic inoculation through the skin. There are more than a dozen reported cases of Pseudallescheria-related pneumonia after near-drowning in contaminated water. Although colonization is more common than infection with this organism, an invasive pulmonary disease similar to invasive pulmonary aspergillosis occurs, usually in immunocompromised patients. Local trauma is the most common cause of eye, soft tissue, and osteoarticular infections in previously healthy persons. CNS infection is seen in both immunocompromised and healthy individuals.4 Infections in immunocompetent patients usually have subacute to chronic courses, whereas those in immunocompromised patients are frequently acute and severe. P. boydii can colonize bronchiectatic lungs, including those of patients with cystic fibrosis, or intermittently obstructed paranasal sinuses. Masses of P. boydii hyphae (fungus balls) have been found in lung cavities.5 P. boydii has also been reported as a cause of allergic bronchopulmonary disease (similar to allergic bronchopulmonary aspergillosis),6 pleural space infection, lung abscess, pneumonia (including aspiration pneumonia), and invasive sinusitis.7 As with invasive pulmonary aspergillosis, invasive pulmonary pseudallescheriasis most commonly occurs in patients with prolonged neutropenia, those receiving prolonged high-dose corticosteroid therapy, or those who have undergone allogeneic bone marrow transplantation.8 Invasive pulmonary disease with associated dissemination appears common9 and has also occurred in patients with acquired immunodeficiency syndrome (AIDS) and after solid-organ transplantation.10 Pulmonary disease in severely immunocompromised patients usually manifests with fever, cough, pleuritic pain, and often hemoptysis. Chest radiography may show areas of nodularity, alveolar infiltrates, consolidation, or cavitation.5 The classic signs of invasive pulmonary aspergillosis, the halo or air crescent signs, may also be seen in invasive pulmonary pseudallescheriasis. Disseminated disease that manifests with only painful cutaneous nodules or endophthalmitis has also been described in immunocompromised patients.11,12 Invasive pulmonary disease with extension to the vertebrae has been described in a patient without apparent immunocompromise.13 Localized disease—including infections of the eye, bone, cutaneous tissue, subcutaneous tissue (Fig. 270-1), and osteoarticular tissue—may be seen both with and without immunocompromise. Infection is commonly initiated through traumatic implantation of the fungus from soil or water. Surgery, intravenous drug injection, and repeated corticosteroid injections have less frequently been associated with localized infections.14 Osteoarticular infection in immunocompetent patients often manifests as a painful, swollen joint with overlying erythema after penetrating injury. In occasional patients, weeks to even years may pass between antecedent trauma and the development of septic arthritis.15,16 Brain abscesses may result from a known or unsuspected lung lesion in immunocompromised patients, including those with AIDS.4,17 CNS infection appears to be disproportionately prevalent among patients with pseudallescheriasis, in comparison with many other mycoses. For example, of 23 solid-organ transplant recipients with pseudallescheriasis, 11 (48%) had CNS involvement.10 Cerebral abscesses are usually multiple; in the immunocompetent hosts, they are often reported in association with near-drownings in polluted water, such as ponds, pig troughs, and roadside ditches.4 CNS infection from contiguous spread of sinusitis18 and after penetrating trauma19 has also been described. Indolent, severe neutrophilic meningitis has been reported occasionally, usually in patients with intravenous drug abuse or human immunodeficiency virus (HIV) infection. Cerebrospinal fluid culture and smear have yielded negative results; the diagnosis was made at autopsy. The first described human case of pseudallescheriasis was meningitis that was probably iatrogenic after lumbar puncture for the administration of anesthesia.20 Isolation of P. boydii from normally sterile sites is diagnostic. Only rarely is P. boydii cultured from blood.2 Growth of the organism from sputum, bronchoalveolar lavage, draining wounds, or paranasal sinus aspirates is less convincing evidence of infection, unless it is accompanied by hyphae on smear or biopsy. Histologically, P. boydii resembles Aspergillus spp., with dichotomously branching septate hyphae seen in tissue. In neutropenic patients, blood vessel invasion and thrombosis are usual. The fungus grows well in standard mycologic media. After a few days, the mold colony takes on a tan color and has sporulating structures that are quite different from those of Aspergillus. Cultures that produce asexual conidia but do not produce the sexual reproductive structure, the cleistothecia, after 2 to 3 weeks are designated by the anamorph name S. apiospermum. No clinically useful serologic or other rapid identification tests are currently available, although sequencing and MALDI-TOF (matrix-assisted laser desorption/ionization time-of-flight) mass spectrometry are being used increasingly for identification of the mold. Effective therapy of pseudallescheriasis remains elusive. In vitro and clinical resistance to amphotericin B, as well as breakthrough infections, have been reported repeatedly. Surgical débridement has been an important adjunct in treatment of pseudallescheriasis of soft tissue, bone, joint, and pleural and paranasal sinuses, although it is not curative by itself. Intraarticular instillation of amphotericin B may have contributed to success of treatment in a few patients. The rate of mortality with brain abscess has traditionally been noted to exceed 75%.4 In the past, intravenous miconazole and surgery had been associated with most successful outcomes in CNS infection.19 Successes have been reported with ketoconazole and itraconazole, mostly in patients with localized infection, and in conjunction with débridement.15,21,22 Combination therapy with liposomal amphotericin B and itraconazole has been used successfully in at least one case of disseminated infection.23 The newer broad-spectrum azole antifungals (including voriconazole, posaconazole, isavuconazole, ravuconazole, and albaconazole) and the echinocandins (anidulafungin, caspofungin, and micafungin) have been shown to have activity against P. boydii in vitro.24,25 Clinical response to voriconazole therapy has been reported in growing numbers of patients,26–28 and response to posaconazole was achieved in a single reported case of brain abscess.29 Voriconazole is approved by the U.S. Food and Drug Administration (FDA) for patients with pseudallescheriasis refractory to other approved antifungal agents and for patients who cannot tolerate those agents. This indication was based on success reported in 15 of 24 patients treated with this agent (including 6 of 10 with CNS infection). Because of poor response to the only approved agent, amphotericin B, most experts believe that voriconazole is the drug of choice in the treatment of pseudallescheriasis. Scedosporium prolificans, a fungus found in soil, was first described in 1984 as an agent of human disease.30 Since that time at least 161 additional cases have been reported. Infection can occur in both immunocompromised and immunocompetent patients. Patients with intact immunity most frequently have focal infections (usually osteoarticular) associated with trauma, whereas immunocompromised persons most frequently have disseminated disease, associated with malignancy.31 In a recent review, only 34 of 162 (21%) patients were noted to have no underlying disease; 72 of the 162 (44%) had disseminated infection.31 In immunocompetent patients, infection is usually localized and associated with trauma including surgery.31–33 These cases have included infections of bone and joints (Fig. 270-2), eye, or wounds and onychomycosis. Immunocompromised patients, commonly those undergoing cytoreductive chemotherapy or bone marrow transplantation, present with fungemia and fever with neutropenia.8,9,34,35 Skin lesions, myalgia, endophthalmitis, and pulmonary infiltrates have been described in this setting.31,36 Skin lesions have been described as a papular rash, later becoming necrotic. Disseminated disease without neutropenia has been described in patients who have undergone lung and kidney transplantation.37 Fatal localized CNS infection was reported in a child with acute leukemia who had received six intrathecal chemotherapeutic injections.38 S. prolificans has also been recovered from the external ear and sputum of patients without apparent disease. Sputum colonization has been observed in patients with AIDS and cystic fibrosis and in those who have undergone liver or lung transplantation.33,39,40 Diagnosis is most commonly established by the recovery of the organism from culture of infected sites, including skin biopsy samples. Disseminated disease in immunocompromised patients is usually diagnosed through blood culture.31,35 Identification of S. prolificans is based chiefly on the morphologic characteristics of the asexual structures produced by the mold in culture.41 No antifungal therapy currently available is effective in treating these infections. S. prolificans appears to be intrinsically resistant to most antifungals.1,3,25 Successful therapy of joint infections has, however, been reported with the use of surgical débridement with or without intraarticular amphotericin B. Disseminated infection is usually resistant to antifungal agents and carries a high mortality rate.31,34 Survival was reported in one patient with disseminated disease and neutropenia who received granulocyte colony-stimulating factor (G-CSF) and amphotericin B, followed by itraconazole.35 In one animal model, liposomal amphotericin B with the addition of G-CSF improved survival.42 Of the currently available antifungal agents, voriconazole appears most promising in vitro, with better activity than amphotericin B, itraconazole, or posaconazole.3,25 Unfortunately, current dosing regimens of voriconazole are not associated with serum concentrations at which the drug appears to be effective in vitro. One report described a 44% response rate (16 of 36 patients) with voriconazole.26 The investigational azole, albaconazole (UR-9825), appears more active than voriconazole in vitro and has shown potential in one animal model.25,43 Because of the in vitro and in vivo resistance of S. prolificans to currently available agents, the effect of combining agents has been examined. In laboratory studies, synergy has been shown through the use of combinations of amphotericin B with pentamidine44 and of terbinafine with voriconazole, itraconazole, or miconazole.45,46 Clinical support for this in vitro synergy is limited, although anecdotal experiences have been reported with voriconazole and terbinafine.47,48 Phaeohyphomycosis is a loosely defined term used to group infections caused by molds (and a few yeasts) that produce dark cell walls. Also described as dematiaceous, these are a diverse group of fungi found in the soil and air and growing on plants and in organic debris. The number of genera and species of fungi causing phaeohyphomycosis is quite large.49 Frequent changes in species names have compounded the difficulty in comparing similar cases from the literature. Chromoblastomycosis (see Chapter 262) and mycetoma (see Chapter 263) are distinct infections that include dark-walled fungi as etiologic agents that are generally not included in this loose classification (Table 270-1). The syndromes most commonly produced by the dark-walled fungi include cutaneous and subcutaneous disease (other than chromomycosis or mycetoma), brain abscesses, and sinusitis. Fungemia50 and disseminated disease51 have more commonly been described in immunocompromised individuals. Meningitis, pneumonia, prosthetic valve endocarditis, contamination of saline-filled breast implants, infections in peritoneal dialysis and central venous catheters, osteomyelitis, and septic arthritis have also been reported. For most clinical purposes, it is preferable to describe disease by the type of infection and species name, such as “Cladophialophora bantiana brain abscess,” and to reserve the term phaeohyphomycosis for cases in which no culture data exist or in which recovered fungi have not yet been identified. TABLE 270-1 Cutaneous and Subcutaneous Infections Caused by Dark-Walled Fungi * The most common causes are listed. See individual chapters for more complete listings (Chapters 262 and 263). Subcutaneous phaeohyphomycosis typically begins as a single red nodule, usually on the extremities. In an immunocompetent person, an indolent, painless expansion in the skin and subcutaneous tissue occurs, sometimes with cyst formation (Fig. 270-3). More rapid local progression and, in rare cases, extension to the brain can occur in immunosuppressed patients. A history of minor trauma is often present, or a splinter is found in the resected lesion. The fungi causing subcutaneous phaeohyphomycosis are extraordinarily diverse, but species of Bipolaris, Exophiala, Exserohilum, Phialophora, and Curvularia are particularly common. Brain abscess is one of the best-described syndromes produced by the dark-walled fungi.52,53 Disease manifests with headache of indolent onset, low-grade or no fever, and development of focal neurologic signs. There is rarely a history of exposure to dust or mold, no obvious pulmonary portal, and no evidence of dissemination outside the CNS. Affected male patients have outnumbered female patients 3 : 1, the median age of diagnosis is 38 years, and most patients have been immunocompetent.53–55 Abscesses may be single or multiple and, on computed tomography or magnetic resonance imaging, are well localized within the cerebral cortex (Fig. 270-4).56 Purulent meningitis, with or without brain abscess, may also be observed (Fig. 270-5).57 Hematoxylin and eosin (H&E) staining reveals abscesses to have purulent centers with surrounding granulomatous reaction, and organisms appear as septate hyphae with golden brown cell walls. As in other forms of infections with the dark-walled fungi, hyphae are commonly irregular in diameter, and yeastlike cells are seen with some species. The species most commonly causing these infections is C. bantiana (previously named Xylohypha bantiana, Cladosporium bantianum, and Cladosporium trichoides), but disease is also caused by Ramichloridium mackenziei, Ochroconis gallopava (formerly known as Dactylaria constricta var. gallopava), Exophiala (Wangiella) dermatitidis, Bipolaris spicifera, Bipolaris hawaiiensis, Chaetomium species, and, even more rarely, other phaeohyphomycetes.53,55,58 R. mackenziei infections are reported chiefly from the Middle East and India,59,60 and E. dermatitidis cases predominate in the Far East. Fonsecaea monophora (formerly classified with Fonsecaea pedrosoi) has been recognized as an etiologic agent of CNS phaehyphomycosis.61 Iatrogenic meningitis and other infections related to epidural injections of corticosteroids have been reported in two recent outbreaks traced to environmental contamination at compounding pharmacies. The first report that involved infection with Exophiala dermatitidis resulted in 4 cases of meningitis and 1 case of sacroiliitis in 2002.62 The second and more recent outbreak included meningitis due to Exserohilum rostratum. Between September and December of 2012, 590 cases of infection and 37 deaths were confirmed among the 13,534 people potentially exposed to the contaminated lots of methylprednisolone.63 Early cases usually presented with meningitis, some with stroke from invasion of arteries in the basilar meninges.64 Later cases more often presented as more localized disease, depending on the site injected with steroid. Lumbar injections were most common, leading to epidural abscess with increased lumbar pain and some with a cauda equina syndrome. Indolent septic arthritis occurred in the sacroiliac joint or rarely in injected peripheral joints. Although hyphae were commonly found in surgical specimens, cultures were only positive for E. rostratum in 14% and polymerase chain reaction (PCR) in 29%.65 Amphotericin B seemed the most effective treatment but was followed by several months of voriconazole therapy. The optimal course of treatment and prevention of relapse is not yet known. Allergic fungal sinusitis may be caused by a wide variety of fungi, although the dark-walled fungi (usually Bipolaris, Exserohilum, Curvularia, or Alternaria spp.) and Aspergillus spp. are the most common causes.66 By definition, disease is allergic and confined to the lumen of the paranasal sinuses. Patients present with an indolent onset of sinus pain or painless proptosis. A history of seasonal or allergic rhinitis is common, and there may be a history of nasal polyps. On computed tomography or magnetic resonance imaging, one or more paranasal sinuses appear full of fluid, with outward pressure on the thinner bony sinus walls, such as the lamina papyracea, medial maxillary wall, or midline sphenoidal septum. Maxillary and ethmoid sinuses are usually involved, but sphenoid and frontal sinuses may be diseased (Fig. 270-6). Surgical débridement of the paranasal sinus removes dark, inspissated mucus; histopathologic examination reveals that this mucus has eosinophils with Charcot-Leyden crystals (degenerated eosinophils) and scattered septate hyphae.67 The walls of the hyphae may not appear as dark as those seen in brain abscess. Irregular diameter and bulbous swellings may help distinguish these hyphae from Aspergillus, but culture is essential for diagnosis. The most serious sequela of allergic fungal sinusitis is brain invasion, which, when it occurs, usually does so in immunocompromised hosts (Fig. 270-7). Extension from the ethmoid or frontal sinus into the frontal lobe of the brain can be clinically silent. Erosion into the frontal lobe, clivus, pterygoid space, or middle fossa occurs but is rare. Sudden blindness can result from compression of the optic nerve posterior to the orbital fissure. Compression of the orbit by lateral bulging of the lamina papyracea does not decrease visual acuity but does cause proptosis. Diagnosis of these infections requires observation of the fungi invading tissue or recovery of the fungi in culture from an otherwise sterile site. Typical pathology is necessary for the diagnosis of allergic fungal sinusitis. In disease outside the CNS, these organisms may not always appear dark walled on standard histopathologic stains. Cell wall melanin may be visible as a brownish-yellow color on H&E stain (Fig. 270-8). If melanin is not evident on fresh preparations of H&E stain, it can be stained by the Fontana-Masson method, which better enables diagnosis, especially if culture results are negative or if culture is not performed.68 Fontana-Masson stain is, however, not 100% specific for the dark-walled fungi because the cell walls of some Aspergillus and other fungi with hyaline hyphae have been shown to stain dark with this method.69 Surgical débridement is essential to the cure of most of the infections caused by the dark-walled fungi. Good surgical curettage often suffices in treating allergic sinusitis if the cranial cavity has not been invaded. Amphotericin B is probably the drug of choice for life-threatening infection including CNS infection. Itraconazole has been used frequently with success in infections that are not life-threatening.70,71 To help prevent further recurrence in patients who have recurrent allergic fungal sinusitis, long-term itraconazole therapy may be used after repeated surgical drainage. In vitro, in response to most of these fungi, voriconazole commonly produces minimal inhibitory concentrations (MICs) that are similar to or lower than those seen with itraconazole, which makes this new drug a potentially useful therapeutic agent. Posaconazole and caspofungin have also been shown to have in vitro activity against many of these fungi. Posaconazole has been reported to produce a good clinical response in single cases of CNS and disseminated infection caused by R. mackenziei and Exophiala spinifera, respectively.72,73 Response of a skin and soft tissue infection to terbinafine, after poor response to amphotericin B and itraconazole, has also been reported.74
Uncommon Fungi and Related Species
Pseudallescheria Boydii
Scedosporium Prolificans
Dark-Walled Fungi and Agents of Phaeohyphomycosis
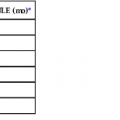
DISEASE
LESIONS
PATHOLOGIC FEATURES
ORGANISMS*
Chromoblastomycosis
Scaly, friable, often verrucous nodules, commonly pruritic
Muriform cells (golden brown cells with cross walls in more than one plane)
Fonsecaea spp., Cladophialophora carrionii, Phialophora verrucosa, Rhinocladiella aquaspersa
Mycetoma (eumycetoma, eumycotic mycetoma)
Nodular with draining sinuses, areas of healing
Grains composed of septate hyphae
Madurella mycetomatis, Leptosphaeria senegalensis, Madurella grisea
Subcutaneous phaeohyphomycosis
Painless, subcutaneous nodules
Septate hyphae (pseudohyphae or yeasts may also be apparent)
Bipolaris spp., Exophiala spp., Exserohilum spp., Phaeoacremonium spp., Phialophora
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree