TABLE 47.1 IMMUNE THROMBOCYTOPENIA | ||||
|---|---|---|---|---|
| ||||
suggesting that the anti-gpIIb/IIIa autoantibody impairs platelet production.25 Megakaryocyte colony formation (colony-forming unit megakaryocyte) is increased in acute ITP.26, 27 In chronic ITP, decreased megakaryocyte colony formation has been reported.28
TABLE 47.2 FEATURES OF ACUTE AND CHRONIC IMMUNE THROMBOCYTOPENIA | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 47.3 CHARACTERISTICS OF PLATELET AUTOANTIBODIES IN PRIMARY IMMUNE THROMBOCYTOPENIA | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
demonstrate phenotypic and functional abnormalities. Platelet reactive T-cell clones can be identified from the peripheral blood of adults and peripheral blood and spleens of children with chronic ITP, suggesting that autoreactive peripheral T lymphocytes may mediate or participate in disease pathophysiology.53, 78, 79 Adults with ITP often have increased numbers of HLA-DR+ T cells, increased numbers of soluble interleukin-2 receptors, and a cytokine profile suggesting the activation of precursor and mature helper T-cells.79 CD3+ T cells from ITP patients in one DNA microarray study had increased expression of genes involved in cell-mediated cytotoxicity and, in addition, cytotoxic cell-mediated lysis of autologous platelets was shown in active ITP.80
 FIGURE 47.4. Petechiae. Pinpoint, nonblanching erythematous capillary bleeding sites are most common in dependent body areas or pressure points. |
accelerated platelet production and the presence of many young forms.137, 138 The changes just summarized are similar to those found in most forms of thrombocytopenia caused by accelerated platelet destruction and are not characteristic or diagnostic of ITP.
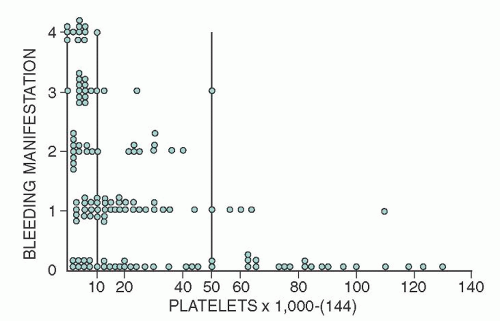
fear in the acute form is intracranial hemorrhage, several large studies show that even with low platelet counts (<30,000/µl) life-threatening bleeding and intracranial hemorrhage are rare (<0.5%).166, 167
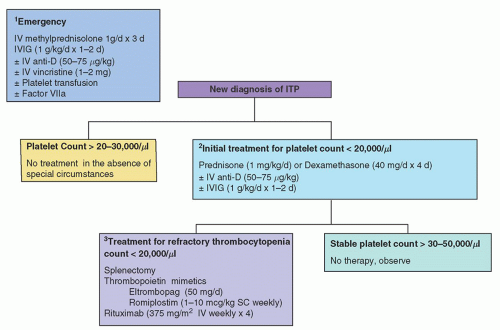
TABLE 47.4 RECOMMENDATIONS FOR INITIAL TREATMENT OF IMMUNE THROMBOCYTOPENIA (IVIG) PATIENTS WITH PLATELET COUNTS <20,000-30,000/µla | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
older than age 45 years.115 This risk of fatal bleeding in patients with platelet counts that are chronically <30,000/µl is estimated at 0.4% per year for patients <40 years of age and 13.0% per year for patients >60 years of age.175
TABLE 47.5 THERAPEUTIC AGENTS AND THEIR DOSING SCHEDULES | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree