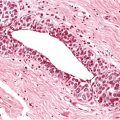
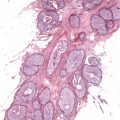
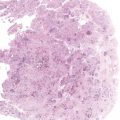
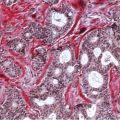
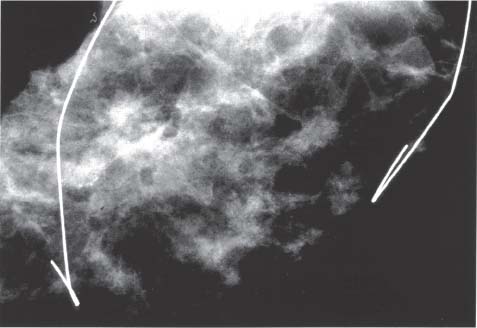
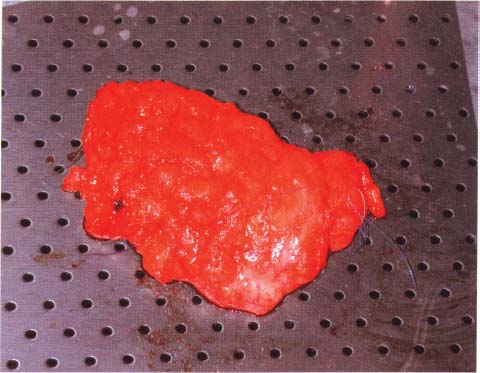
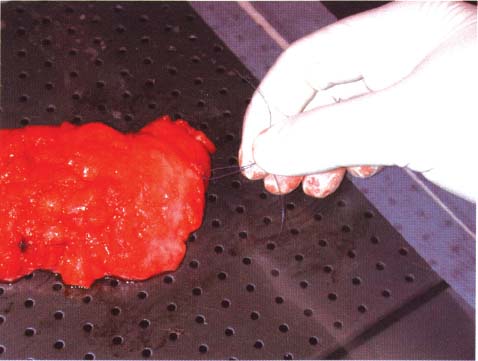
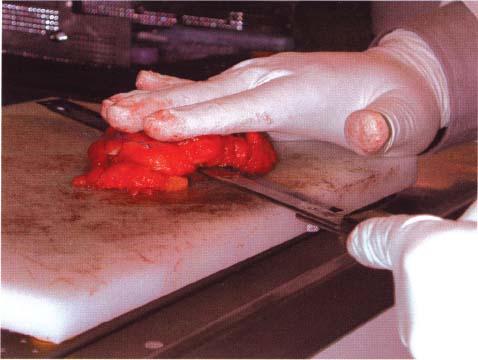
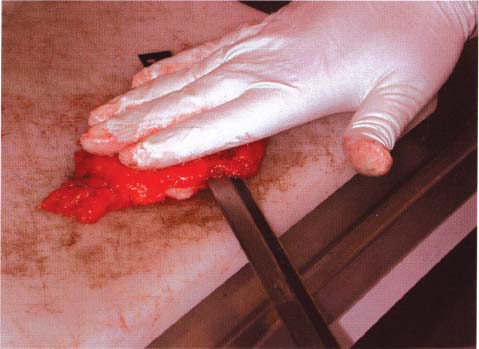
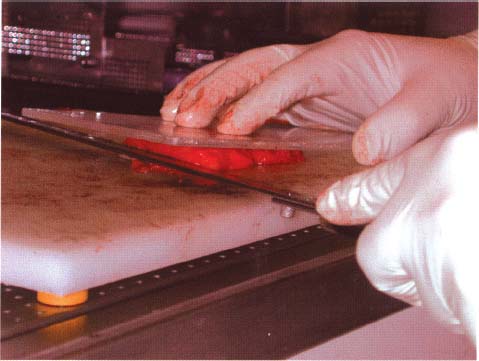
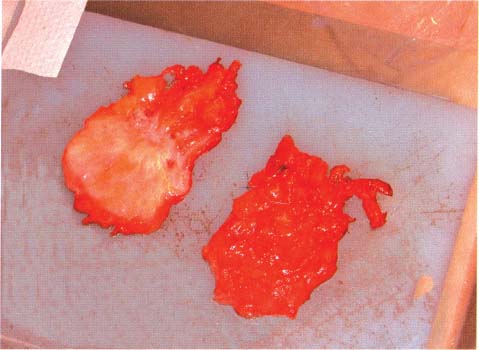
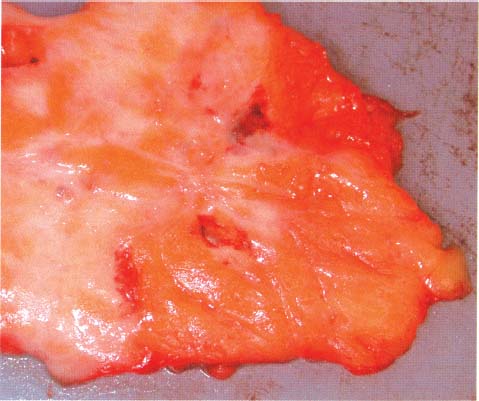
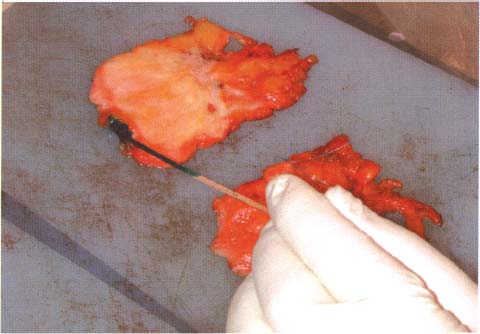
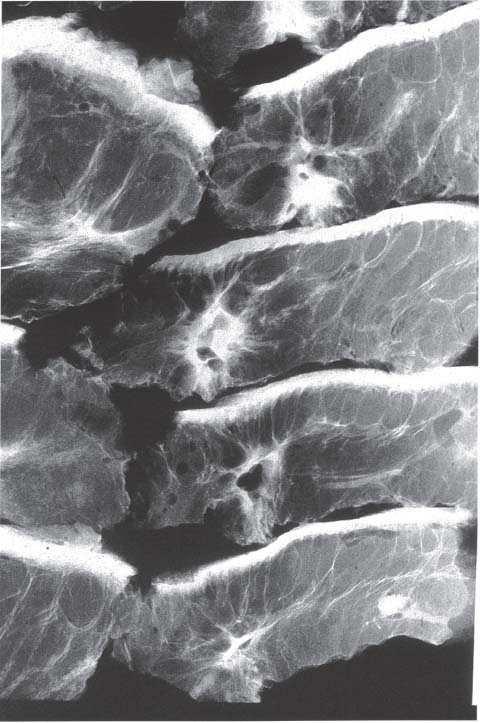
Chapter 8 The Postoperative Work-up To determine the real extent, size, and distribution of the lesions in the excised breast tissue, the histologic findings need to be directly correlated with the clinical, mammographic, and macroscopic findings. To accomplish this correlation, the pathologist should prepare and examine sections of tissue that are as large and as continuous as possible. To this end, the technique of large histologic sections is unquestionably superior to the traditional small-block technique. The production of a two-dimensional large-section image needs to be carefully planned. The method of the cut up of the specimen differs according to the type of the operation (mastectomy or segmentectomy/quadrantectomy) and lesion (microcalcifications, solitary or multiple tumors). The specimen is received in a fresh state after specimen radiography is performed to confirm the presence of the preoperatively diagnosed radiologic abnormality within it. The specimen radiogram (Fig. 8.1) assists the pathologist in planning the cut-up to include a transsection of the entire abnormality in a single large section. Thorough macroscopic examination of the specimen is also important. The size of the specimen should be measured in three dimensions, and the number and type of the marking sutures (Fig. 8.3) and the number and position of the guide wires should be recorded. Because the specimen consists of soft breast tissue atop a firm base (radiograph film, table), it usually takes the form of a relatively flat piece of tissue (Figs. 8.2 and 8.3). The larger tumors are firmer and are usually easily located by inspection and palpation. The smaller tumors are not directly seen on macroscopic examination of the unsliced specimen, but are often palpable and are usually easily seen on the specimen radiograph. If the specimen contains only radiologically detected microcalcifications or a small nonpalpable tumor, finding the appropriate plane for slicing is totally dependent upon careful mammographic guidance. In the latter situation, it is best to slice the specimen horizontally (parallel with the table) in the plane of the specimen radiograph (Figs. 8.4 and 8.5). This is recommended even in the presence of a solitary well-defined tumor mass. Multiple tumors are more difficult to demonstrate in a single large section. In these cases, the plane for the slicing should be chosen on the basis of palpation of the entire specimen and on evaluation of the specimen radiograph. Fig. 8.1 Fig. 8.2 Fig. 8.3 Fig. 8.4 For adequate slicing of a fresh breast specimen, a special knife with a very sharp disposable blade is needed. The blade must be changed after every two or three breast specimens are cut, more often when very hard or calcified tissue is encountered. It is more dangerous for the pathologist to use a dull blade than to use a very sharp one. Inexperienced pathologists are advised to use a translucent plastic plate to push the specimen against the table instead of holding it directly with their hand (Fig. 8.6). The slices should be 3 to 4-mm thick (Figs. 8.7 and 8.8). A considerable variation in thickness within the same slice or among slices can markedly reduce the technical quality of the specimen mammograms and histologic sections. The slices need to be thoroughly examined macroscopically. The well-formed tumor masses should be described and measured in millimeters. The relation of the tumors to the resection margins must be described in terms of the minimum number of millimeters of tumor-free margins. A lengthy macroscopic description is unnecessary because the cut surface of the entire specimen is demonstrated on the large histologic sections. Fig. 8.5 Fig. 8.6 Fig. 8.7 Fig. 8.8 Fig. 8.9 Inking of the surface of the specimen is not necessary with this technique, but colored inks should be used to mark the position of the marking sutures (Fig. 8.9). The 3 to 4-mm slices then undergo repeat specimen radiography. The radiographic examination of the slices (Fig. 8.10) is always a useful procedure and is absolutely necessary in cases with mammographically detected microcalcifications, those with multifocal tumors, and those with nonpalpable lesions. The radiologist compares the mammographic findings and the findings on specimen radiography with the radiologic images of the macroslices, and then marks the slices that have radiologic abnormalities. The pathologist must correlate the macroscopic findings in the marked slices with the radiologic abnormalities. The most representative slices are selected for imbedding and processing: the slices with the largest tumor diameter, those containing the largest number of tumor foci in the cases with multifocal tumors, those containing macroscopically and/or radiologically discernible non-malignant lesions, and those containing microcalcifications. It is worth mentioning that pathologists are fully responsible for tissue sampling, even with radiologic assistance. Therefore, they are encouraged to sample all suspicious macroscopic abnormalities, even those that have not been marked by the radiologist. The recommended average number of selected slices per case is two to four. At this step, small tissue blocks may be taken for immunohistology, image analysis, flow cytometry, and molecular biologic examinations, but the most representative slices must be left intact. Because the reliability of the histologic diagnosis of mammographically detected and macroscopically poorly defined lesions depends upon mammographic-pathologic correlation, one adequate large section is more important than the additional examinations. In these cases, especially if the lesion is smaller than 10 mm in the largest dimension, sampling of the tumor tissue for special examinations or taking intraoperative frozen sections is contraindicated. Fig. 8.10
The Postoperative Work-up
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree