The Diabetic Foot: Strategies for Treatment and Prevention of Ulcerations
John M. Giurini
Diabetic foot disease affects nearly 2 million patients with diabetes in the United States annually (1). This places an inordinate social and economic burden not only on the United States healthcare system but also on the families of these patients. It is estimated that almost $200 million is spent annually strictly for the care of the diabetic foot (2). This represents only the direct costs of hospitalization, medications, and surgery. Indirect costs such as lost employment, disability, and stress on the family unit cannot even be estimated. More amputations are performed in patients with diabetes than any other group of patients.
The management of diabetic foot disease is focused primarily on avoiding amputation of lower extremities. This goal is carried out through three main strategies: identification of the “at-risk” foot, treatment of the acutely diseased foot, and prevention of further problems. Vital to the success of any program is education of the patient and family members. A comprehensive program of diabetic foot management must include each of these aspects for successful salvage of limbs.
These goals are best met by the establishment of a dedicated limb-salvage team. The members of this team must be dedicated to meeting the challenge of the patient with diabetes whose fears of limb loss are rivaled by fears of blindness and kidney failure (3,4). Members of this team most commonly include a podiatrist, an endocrinologist, a vascular surgeon, and a pedorthist. The team also may include plastic surgeons, infectious disease specialists, orthopedic surgeons, and diabetes teaching nurses. All players must know their role and be available in a timely fashion for consultation.
Several systems exist for grading the at-risk foot (5,6,7). The main purpose of any classification system is to standardize descriptions of lesions and to formulate algorithms for treatment. While each system claims to be complete, all have pitfalls. Identifying the patient with diabetes at risk for ulceration requires examination of the feet, including the vascular and neurologic systems, skin condition, and foot structure.
IDENTIFICATION OF RISK FACTORS
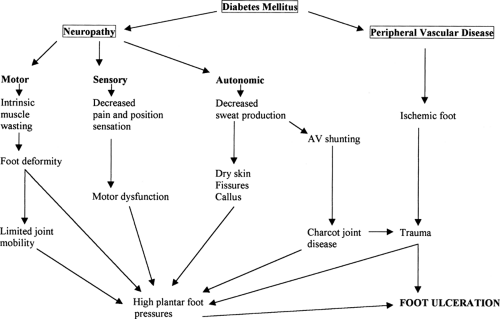
While certain clinical features are known to increase the risk for lower-extremity amputation, peripheral sensory neuropathy has been identified as the major risk for diabetic foot ulceration (8). Pecoraro et al. (9) placed peripheral sensory neuropathy in the face of unperceived trauma at the entrance to the pathway to ulceration and amputation (Fig. 66.1). The inability of a patient with diabetes to feel pain places him or her at significant risk for future foot problems. Knowledge of this condition and education on preventive measures are critical to the patient’s ability to avoid ulcerations. However, even with appropriate preventive measures, ulcerations will develop. Unperceived or unintentional trauma occurs that results in breaks in the skin and inoculation by bacteria.
Clinically significant peripheral sensory neuropathy can be detected by using a 128-millihertz (mHz) tuning fork and a 5.07 Semmes–Weinstein monofilament wire as screening tools to identify at-risk patients (10,11,12). While loss of vibratory sensation is the initial step in the development of clinically significant neuropathy, grading with a tuning fork is often a subjective exercise without scientifically established norms. A biothesiometer provides more objective documentation of a patient’s ability to perceive vibratory sensation. Clinical studies have determined a vibratory perception threshold of 25 mHz as identifying patients at risk for ulceration (13). This instrument, however,
is not readily available to the practicing clinician. It is used primarily in clinical trials where documentation of the degree of sensory neuropathy is important in stratifying groups.
is not readily available to the practicing clinician. It is used primarily in clinical trials where documentation of the degree of sensory neuropathy is important in stratifying groups.
The 5.07 (10 g) Semmes-Weinstein monofilament wire is an effective and inexpensive device to identify the patient at risk for foot ulceration. Several clinical trials have demonstrated that patients with diabetes who are unable to perceive this gauge of monofilament wire are at a statistically significant higher risk for development of ulceration than are patients who are able to detect the wire (12). Proper use of the wire requires application of the wire against the foot with enough force to gently bend the wire (Fig. 66.2). Inability to feel the wire implies lack of adequate protective sensation. By testing different sites on the foot, areas of insensitivity can be mapped and identified to the patient. These patients then must be educated on the significance of sensory neuropathy and the steps to preventing foot ulcerations. Regular evaluation by a foot care specialist is recommended for these individuals.
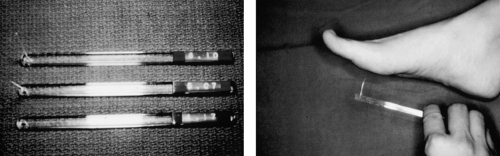 Figure 66.2. Proper use of the monofilament wire requires application of just enough pressure to bend the monofilament. |
Formal nerve conduction studies in patients with diabetes have not been shown to alter treatment planning. Nerve conduction studies are rarely helpful or necessary for the evaluation of neuropathy. Many patients with type 2 diabetes have clinically significant neuropathy at the time of diagnosis, and nerve conduction studies will be abnormal in the majority of these patients.
Motor neuropathy can produce foot deformities that put the foot at risk for ulceration (Fig. 66.3). Loss of innervation of the
intrinsic musculature of the foot can lead to common foot deformities such as hammer toes, claw toes, and plantar-flexed metatarsals. Plantarly prominent metatarsal heads result in areas of high focal pressures that have been shown to increase risk for foot ulceration. Digital deformities can be irritated dorsally by shoe gear, resulting in corns or even ulcerations.
intrinsic musculature of the foot can lead to common foot deformities such as hammer toes, claw toes, and plantar-flexed metatarsals. Plantarly prominent metatarsal heads result in areas of high focal pressures that have been shown to increase risk for foot ulceration. Digital deformities can be irritated dorsally by shoe gear, resulting in corns or even ulcerations.
 Figure 66.3. The intrinsic minus foot is particularly vulnerable to ulceration as a result of the digital and plantarflexion deformities that may occur. |
Autonomic neuropathy, although less common than peripheral sensory neuropathy, can also affect the feet. Most commonly, autonomic neuropathy affects local temperature regulation and the function of sweat glands. Loss of sweat production can lead to dry skin (14). Untreated this can lead to cracking and fissuring, especially in the heel, creating a portal of entry for bacteria.
Peripheral vascular disease by itself is responsible for only a small percentage of diabetic foot ulcerations. Only 15% of all diabetic foot ulcers are purely ischemic (15). However, arterial insufficiency can lead to nonhealing of ulcerations once they have developed. The single most important indicator of adequate perfusion is the presence of palpable pedal pulses. Additional clinical maneuvers to assess vascular status should include measurement of the venous filling time and evaluation for dependent rubor and pallor on elevation. The presence of a slowly or nonhealing ulceration in the face of absent pulses warrants further evaluation. This may be in the form of noninvasive arterial studies. Pulse volume recordings and the character of the distal pulses on Doppler evaluation (monophasic vs. triphasic) can provide valuable information on the patient’s ability to heal the ulceration. Although ankle-brachial indices (ABIs) are measured, they are of limited usefulness in the patient with diabetes. The ABIs often are artifactually elevated due to medial calcinosis of pedal vessels. Assessment of a patient’s ability to heal should not be based solely on this measurement. The presence of a nonhealing ulceration with clinical or objective evidence of arterial insufficiency warrants a prompt referral to a vascular surgeon (16).
The areas under the metatarsal heads are the most vulnerable areas for plantar ulcerations. These areas have been identified as having high focal pressures in patients with diabetes (17,18,19). A symptom of these high pressures is the presence of callus tissue under a metatarsal head. This most commonly results from plantarly prominent metatarsal heads, as occurs in the intrinsic minus foot and when the plantar fat pad atrophies (20,21). More recently, an association between limited joint mobility and high plantar foot pressures has been discussed as a risk factor for foot ulcerations (22,23). Other causes of high foot pressures include developmental foot deformities such as bunions, hammer toes, or rocker-bottom deformities from Charcot joint disease.
Quantitation of plantar foot pressures in the form of vertical load is possible with various computerized pressure-sensing equipment (24). These devices are expensive for most private practitioners and are most useful as a research tool. A Harris mat (ink-impregnated foil that demonstrates pressure points in static stance), however, is a simple, inexpensive tool that can be helpful in identifying areas of high plantar foot pressures.
CLASSIFICATION OF ULCERATIONS
As previously noted, several classification systems for grading ulcerations exist (6). Classification systems have two primary purposes: (a) to provide healthcare professionals with a common language to describe and understand common conditions, in this case diabetic ulcerations; and (b) to help direct the management and treatment of these conditions. While these are noble and useful purposes, there are also notable deficiencies in each of these grading systems. Some neglect the importance of ischemia, others are too complex to remember, and others are not completely applicable to diabetic ulcers but are more appropriate to pressure or decubitus ulcers. Nevertheless, for the purposes of this book, the Wagner classification has been selected for the discussion of ulcerations and their management, as it is the simplest, best known, and most widely used system. One should, however, by aware of its shortcomings. The Wagner classification system is based strictly on ulcer description and depth. It ignores the importance of ischemia and infection in determining the severity of the ulceration. In other words, although a Wagner grade 1 or 2 ulceration in a patient with adequate blood flow can often be managed with little to no complications, a similar condition in patients with poor perfusion can be a limb-threatening condition.
Grade 0 Foot
The Wagner grade 0 foot is the diabetic foot without ulceration but with one or more risk factors. Clinically significant sensory neuropathy as described above is one such risk factor. Other risk factors include bony deformities, atrophic fat pad, plantarflexed metatarsals, peripheral vascular disease, and Charcot joint disease. Dermatologic conditions also may pose risks to the grade 0 foot. Such conditions include dry, scaly skin with fissures, or thickened, discolored nail plates as seen in chronic onychomycosis. Although peripheral sensory neuropathy is the primary component cause for ulceration, the predictive index for ulceration increases significantly with each additional component cause identified (25). This constellation or grouping of risk factors is referred to as sufficient causes for ulceration (i.e., two or more component causes equal a sufficient cause for ulceration) (25).
Appropriate evaluation of this foot should include a careful neurologic examination using the 5.07 Semmes-Weinstein monofilament wire (26). Mapping of insensate areas helps the patient and the physician identify vulnerable areas. The foot should be closely inspected for corns or calluses, because these areas will identify focal pressures or irritation that may lead to ulceration. The vascular examination should include palpation of pedal pulses and observation for pallor with elevation or rubor on dependency. The physician should inspect for fissures either on the heels or in the interdigital spaces.
Management of the grade 0 foot centers on a program of education and prevention. Patients should be educated about the risks associated with the neuropathic foot and instructed on the early signs of inflammation, irritation, and infection and the initial treatment of these conditions. They should also be educated
on the importance of good glycemic control in the management of foot disease.
on the importance of good glycemic control in the management of foot disease.
Disease prevention in this patient population may include shoe-gear modification to decrease plantar foot pressures and to accommodate foot deformities and the use of orthotic devices and padded hosiery to further decrease plantar foot pressures (27,28). The simple habit of changing shoes every 4 hours can also help modify plantar foot pressures. This simple technique has several advantages in ulcer prevention: (a) it prevents the accumulation of pressure over any one area of the foot for extended periods; (b) it reduces loss of shock absorption and support functions of the outer soles and leather uppers, which occur the longer a shoe is worn; (c) it provides the patient with the opportunity to inspect his or feet frequently, allowing earlier detection of potential foot lesions (Table 66.1).
TABLE 66.1. Advantages of Changing Shoes | ||||
|---|---|---|---|---|
|
Regular visits to the foot specialist are recommended as part of a program of education and prevention. Depending on the patient’s risk category, these visits should be scheduled annually, semiannually, or more frequently. Pulses should be palpated and any lesion should be noted at each visit. Corns and calluses should be debrided (29,30,31). The patient should be instructed on the proper care of the nails and skin. Moisturizing creams should be prescribed for application to the bottom of the foot for dry, scaly skin to avoid fissures. The interdigital spaces should also be inspected for fissures or evidence of tinea pedis.
The single most important aspect of preventive self-care is for the patient to inspect his or her feet daily. In those situations in which patients are unable to perform this function themselves, a family member should receive instruction on how to do this properly. Proper inspection involves inspecting the bottom of the foot visually and feeling it for lesions such as blisters, loose skin, or open sores. Patients also should note any areas of unexplained swelling or redness. The interdigital spaces are particularly problematic areas. They should be inspected and kept dry to prevent maceration, which may lead to athlete’s foot and secondary bacterial infection.
Grade 1 Foot
The grade 1 ulceration implies the presence of two or more risk factors: peripheral sensory neuropathy and at least one other risk factor, such as bony deformities, plantarly prominent metatarsal heads with distally displaced fat pad, limited joint mobility, or ill-fitting shoes. The grade 1 ulceration extends to the dermis but not beyond (5). The evaluation of ulcerations should include a search for risk factors and an underlying cause. Ulcerations themselves should be evaluated for size, depth, and location. Knowledge of the anatomic structures involved, as well as the presence of any infection, will help direct treatment. The presence and type of drainage should also be noted. Cultures are of limited usefulness at this stage as the ulceration likely will be colonized with multiple organisms representing primarily skin flora (32).
Treatment most commonly requires soft-tissue debridement and elimination of all pressure from the site of ulcerations (8). Ulcerations most commonly will have some degree of hyperkeratosis surrounding the ulcer bed. In many cases, this callus tissue will overhang the margins of the ulcer, thus preventing ulcer healing from the “inside out.” Therefore, all exuberant hyperkeratotic tissue must be debrided to a healthy granular bed that will support further granulation. Debridement has the added advantage of promoting dependent drainage and perhaps stimulating growth factors. Studies have suggested that ulcers that have undergone aggressive debridement may heal faster (33).
The second important concept of wound healing is off-loading, the technique by which pressure at the site of the ulceration is eliminated or reduced. There are various means of accomplishing this. The most effective is total non-weight-bearing on the affected extremity by means of crutches or a walker. This is often impractical for most patients, making compliance a serious issue. Therefore, techniques such as the total-contact cast and felted foam dressings have been devised as a compromise to relieve pressure, increase compliance, and improve the chances for healing (34,35,36,37).
Dressings are changed daily to provide a moist wound environment, which has been shown to be conducive to wound healing. Normal saline, hydrogels, and growth factors are acceptable choices for superficial ulcerations without active drainage or infection. Harsh, undiluted chemicals should be avoided, as they can be toxic to granulation tissue (38). Topical antibiotics have limited usefulness in this setting (39). If an infection is suspected, it is best treated with systemic antibiotics. Oral antibiotics are recommended only when clinical signs of infection are present (i.e., erythema, purulent drainage). Overuse of oral antibiotics may lead to superinfection or development of resistant strains. Exceptions to this rule include patients with severe peripheral vascular disease, in whom development of infection may be limb-threatening, or in patients receiving immunosuppressive medications, as in kidney or kidney/pancreas transplant recipients.
Grade 2 Foot
Failure to adequately off-load grade 1 lesions likely will lead to deepening ulcerations beyond the level of the dermis (5). Deeper structures such as tendons or joint capsule may often be involved (grade 2). Appropriate management of these ulcerations depends on the accurate assessment of ulcer depth and the structures involved.
The most accurate and cost-effective method for assessing ulcer depth is to probe the ulcer base gently with a stainless-steel blunt probe. This technique can detect undermining of the ulceration, presence of any penetrating sinus tract, and involvement of deeper structures (Fig. 66.4). The ability to probe bone with this simple technique has an 89% specificity for the diagnosis of osteomyelitis. This compares favorably with more expensive and invasive tests such as labeled white blood cell (WBC) scans and magnetic resonance imaging (MRI) (46). Bone, joint, or tendon involvement should alert the clinician to the possible need for hospitalization, complete bed rest, surgical debridement, and broad-spectrum intravenous antibiotics (47).
 Figure 66.4. A blunt stainless steel probe is a clinically cost-effective tool for diagnosing osteomyelitis. |
Areas of undrained infection should be opened and drained dependently. Although most of these debridements can be performed at the bedside in severely neuropathic patients, if the infection is expected to be extensive, the patient should be brought to the operating room for a thorough debridement. The wound is then packed open (47). All nonviable, necrotic tissue
should be sharply debrided. This may often require the removal of infected tendon and/or bone. Antibiotics are adjusted to cover the offending organisms. The choice of antibiotics should be based on deep cultures taken at the time of surgery (48).
should be sharply debrided. This may often require the removal of infected tendon and/or bone. Antibiotics are adjusted to cover the offending organisms. The choice of antibiotics should be based on deep cultures taken at the time of surgery (48).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree