Key points
- •
Precise assessment of disease progression and adequate selection of initial therapeutic options should be performed through a multidisciplinary approach in the treatment of liver metastases.
- •
Selected patients with colorectal liver metastases are candidates for curative hepatic resection with 5-year survival up to 58%.
- •
Number, size, and bilobar distribution of liver metastases do not limit the indication of surgery when R0 resection is feasible.
- •
Surgical resection should be deferred in patients with significant progression of metastatic disease during treatment with optimal preoperative chemotherapy until achieving disease control with second-line systemic chemotherapy or regional therapies.
- •
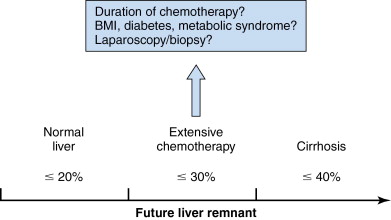
Minimal requirement of standardized future liver remnant is dependent on the status of the underlying liver (>20% in normal liver, >30% in damaged liver, and >40% in cirrhosis).
- •
Selected patients with advanced liver metastases benefit from reversed approach (resection of metastases prior to primary lesion) or staged hepatectomies.
- •
Radiologic complete response to chemotherapy does not signify complete pathologic response. Therefore, surgical resection should include all the original sites of metastases.
- •
Surgical resection of metastases from neuroendocrine tumor reduces symptoms and prolongs survival even after cytoreduction surgery. However, multidisciplinary approach is usually required in advanced disease.
- •
Significance of surgical resection of metastases of noncolorectal and nonneuroendocrine origin is still unclear.
Introduction
The liver is the most common site of hematogenous metastases from various malignancies, particularly those originating from the gastrointestinal tract. Although the patients having liver metastases are classified as stage 4 in TNM (tumor, node, metastasis) classifications, favorable long-term outcomes have been reported when curative resections are feasible especially in the patients with colorectal liver metastases (CLMs) , or neuroendocrine tumors (NETs). ,
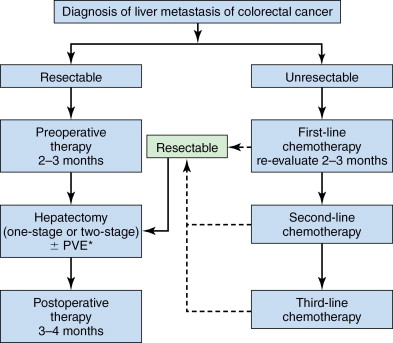
With recent advancements in chemotherapy and growing use of portal vein embolization (PVE), resectability of CLM has dramatically increased, and long-term survival after resection of CLM has significantly improved. The practical keys in initial clinical management of patients with CLM are (1) precise assessment of extension of disease and (2) adequate selection of therapeutic options. Surgical resection is potentially the most curative therapeutic strategy for liver metastases. However, to select the patients who would truly have prognostic advantages from surgery, a multidisciplinary approach by surgeons, medical oncologist, radiologist, and pathologist is essential ( Figure 13-1 ).
Colorectal liver metastases
Colorectal cancer is the second leading cause of cancer-related death in the United States. The 20%–25% of patients are found to have synchronous CLM, , and 35%–55% of patients develop CLM during the course of the disease. However, the 5-year survival after curative resection of CLM has been reported to be up to 58%, whereas median survival of CLM without any treatment is approximately 6 months. Therefore, adequate assessment and preoperative management are important to select the patient with resectable or potentially resectable CLM.
Preoperative assessment
Assessment of oncological resectability
In pretreatment assessment of oncological status of CLM, liver dynamic computed tomography (CT) is a standard imaging modality with an adequate sensitivity and specificity. Magnetic resonance imaging (MRI) and positron emission tomography (PET) can be added in selected cases to improve the diagnostic accuracy, especially for diagnosis of indeterminate lesions, detection of local recurrence, or screening of extrahepatic disease. However, the choice of imaging modalities should be based on the local expertise and the balance between the costs and benefits.
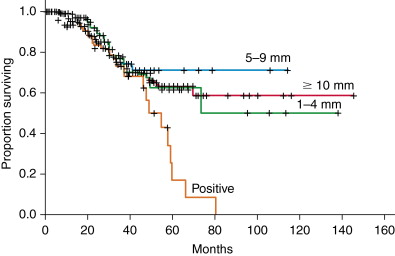
Previously, four or more tumors, size >5 cm, bilateral disease, and narrow surgical margin <1 cm were reported to be negative prognostic factors, and accordingly, they have been considered as contraindications for liver resection. In the era of effective systemic therapy and PVE, however, the oncologic criteria for liver resection is shifting toward complete resection of all viable disease because favorable outcomes would be expected in a selected patient amenable to curative resection even with extrahepatic diseases. Also, a multicenter study of 557 patients has reported that width of surgical margin does not affect the overall survival if negative margin can be obtained ( Figure 13-2 ). Therefore, large number, size, and bilobar distribution of tumor are no longer absolute contraindications for hepatic resection as long as R0 resections are feasible ( Table 13-1 ).
| Conventional Criteria | Current Consensus | |
|---|---|---|
| ONCOLOGIC CRITERIA | ||
| Number | ≤3 | No limitation if R0 resection is feasible |
| Size | ≤5 cm | No limitation if R0 resection is feasible |
| Distribution | Unilateral distribution | No limitation if R0 resection is feasible |
| Extrahepatic disease | Contraindication | If curatively resectable or long-term control can be expected |
| TECHNICAL CRITERIA | ||
| Surgical margin | ≥1 cm | Microscopic R0 resection |
| Future liver remnant (FLR) | Anticipated ability to preserve adequate FLR volume with intact blood flow and biliary drainage | Anticipated ability to preserve adequate FLR volume (>20% in normal liver, >30% in extensively treated liver) a with intact blood flow and biliary drainage |
Assessment of technical resectability
Technical resectability is determined by the balance between the feasibility of curative resection (R0 resection) and preservation of adequate inflow–outflow pathways for the liver remnant. Technical feasibility of liver resection basically depends on the distribution of tumors and vascular anatomy. Because the metabolic performance of the liver is highly dependent on both intact inflows (i.e., arterial and portal flows) and adequate outflows (i.e., venous flow and biliary drainage), patency of these four vessels is essential to expect a full performance of the future liver remnant (FLR).
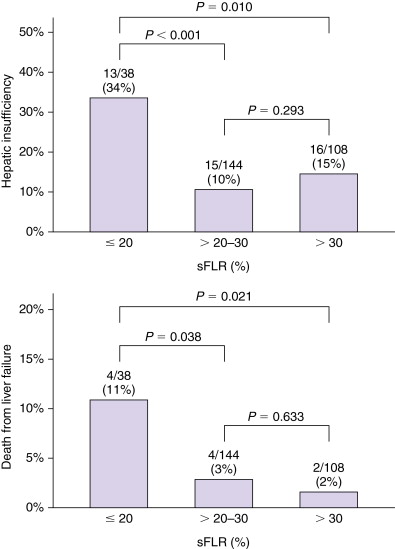
Currently, functional reserve of the liver is estimated by both static and dynamic measurements. The most reliable static variable is the FLR volume. Because absolute volume of FLR against standardized liver volume (SLV) (i.e., sFLR: standardized FLR) has strong correlation with the rates of postoperative morbidity and mortality ( Figure 13-3 ), , minimal requirements of sFLR has currently been set at >20% in normal liver, >30% in damaged liver after extensive treatment, and >40% in cirrhotic liver ( Figure 13-4 ). These cutoff values offer a good practical decision making in patients requiring major hepatectomy. Dynamic measurements such as degree of hypertrophy, indocyanine green clearance test, or hepatic scintigraphy have also been reported to be a sensitive variable to evaluate functional reserve of the liver. Because FLR volume itself is not correlated with functional reserve, dynamic measurements should be integrated to estimate the total functional reserve of FLR in individual patients.
Preoperative management
Neoadjuvant chemotherapy
Recent advancements in chemotherapeutic agents and delivery have changed the treatment of CLM dramatically. With introduction of oxaliplatin and irinotecan, the response rate of CLM has reached more than 50% and the conversion rates from unresectable to resectable metastases has been reported to be up to 38%. , Moreover, molecular target agents such as bevacizumab has further augmented these responses upward of 80%. , When patients are treated with preoperative systemic therapy, they benefit by observing the biological behavior of the tumor. Progression in the form of development of new lesions (growth in more than three existing liver metastases and/or the development of multiple new lesions) during treatment with optimal preoperative chemotherapy is strongly associated with poor hepatectomy outcomes. Therefore, surgical resection should be deferred until achieving disease control with second-line systemic or regional therapies.
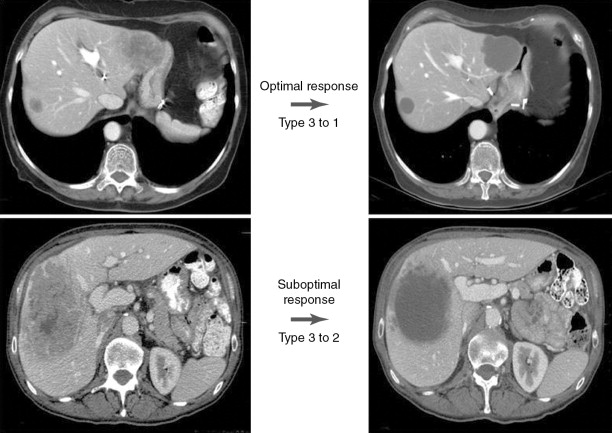
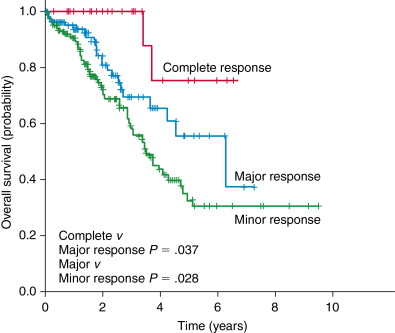
Conventionally, the Response Evaluation Criteria in Solid Tumors (RECIST) , have been utilized to assess the response rate of CLM to chemotherapy. However, there is an inconsistency between this unidimensional measurement and pathologic response, and also better predictive value of dynamic changes in tumor size compared to the established cutoff value in RECIST have been reported. , Recently, our group has reported a new morphologic criterion to assess the response to chemotherapy ( Figure 13-5 ). These criteria are well correlated with viability of tumor cells (pathologic response). Because the pathologic response is the strong predictor of survival ( Figure 13-6 ), morphologic classification is a better predictor of surgical outcomes after neoadjuvant chemotherapy.
Despite the oncologic advantages of preoperative chemotherapy, longer duration of chemotherapy has not been shown to improve survival over shorter courses, but it has been associated with liver toxicity, posthepatectomy liver insufficiency, and mortality. , In the recent EORTC (European Organization for Research and Treatment of Cancer) trial, the use of perioperative chemotherapy decreased the rate of nontherapeutic laparotomy but was associated with an increase in posthepatectomy complications. Therefore, the risk and benefit should be balanced in preoperative chemotherapy.
Portal vein embolization
PVE is a safe, minimally invasive procedure that leads to an atrophy in the side of the liver to be resected and compensatory hypertrophy of FLR. Our previous studies have shown that sFLR >20% is a minimal requirement in patients with a normal underlying liver and the extended right hepatectomy can be performed safely in patients who have achieved an sFLR >20% after PVE for insufficient initial FLR. , Based on the criteria according to baseline status of liver parenchyma (see Figure 13-4 ), PVE should be considered if a patient is found to have insufficient volume in pretreatment measurement of FLR.
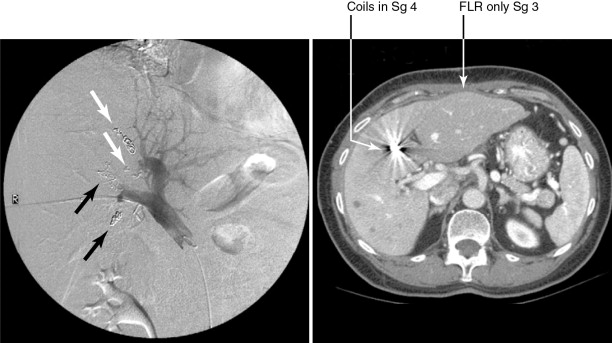
To maximize the regeneration of FLR in PVE, optimal selection of embolic materials and concurrent embolization of segment 4 portal vein , has been recommended. Our previous work comparing right PVE with and without segment 4 embolization revealed significant difference in volume increase rates in segment 2+3 (median, 26% vs. 54%; P = .021) ( Figure 13-7 ).
Contraindications of PVE include portal hypertension, tumor extension to the FLR or portal vein, coagulopathy that cannot be corrected, biliary dilation in the FLR, and renal failure.
Surgical approach
Basic concepts
The surgical strategy for CLM is determined by its safety and oncological efficacy. When the tumor burden is limited with anatomically favorable distribution, a one-stage surgery involving one or more simultaneous partial to lobar liver resection is safe and effective. , Type of liver resection (anatomic resection vs. nonanatomic resection) has no significant impact on the outcome in patients with CLM. ,
Also, width of surgical margin does not affect the overall survival if R0 resection is feasible. For the cases with extensive bilobar metastases, several strategies are still available in selected patients. With the use of preoperative chemotherapy and PVE, these patients would benefit from surgical resection. Therefore, surgery should actively be considered in possibly resectable patients through a multidisciplinary approach.
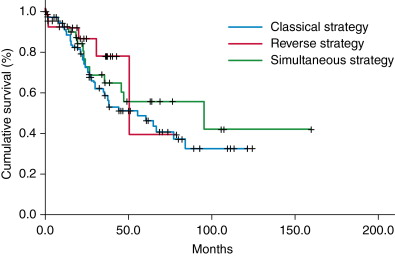
Strategy for synchronous metastases
In patients with synchronous presentation of CLM at the diagnosis of colorectal cancer, liver resection was conventionally performed after resection of primary lesion followed by adjuvant chemotherapy (Classic approach). A combination strategy, with simultaneous resection of the primary lesion and CLM (Combined approach) has also been used to avoid delaying surgical resection of metastatic disease. However, this strategy is associated with an increased risk of postoperative complications when major liver resection is combined with the resection of primary lesion. A “Reverse approach” is another option that has been proposed recently, where liver resection precedes resection of the primary tumor. A study that compared these three different surgical approaches revealed no difference among these groups in survival rates ( Figure 13-8 ). Therefore, the optimal approach should be selected according to the status of both the primary lesion (symptoms, invasiveness, node status, etc.) and CLM.