(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
The ischiorectal fossa, a roughly triangular space in the lower pelvis, is bound by a lateral wall from the obturator internus and its fascia, a medial wall from the lower surface of the levator ani and the anal canal, and an inferior wall from the urogenital diaphragm. The obturator internus arises from the inner (upper) surface of the obturator membrane and the surrounding edge of the obturator foramen. Draped around the ischial ramus, it exits the pelvis through the lesser foramen. A condensation of the obturator fascia, the tendinous arch extending from the obturator foramen anteriorly to the ischial spine posteriorly, provides the origin of the levator ani and splits the surface of the obturator fascia in two portions, the inferior forming the lateral wall of the ischiorectal fossa.
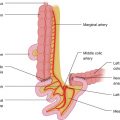
The pudendal nerve and vessels on the lower surface of the piriformis exit the pelvis through the greater sciatic foramen on the surface of the ischial spine (or sacrospinous ligament). They immediately reenter the pelvis, coursing around the spine and then on the surface of the fascia of the obturator internus in the ischiorectal fossa. The nerve gives off a branch, the inferior rectal nerve, which supplies the external anal sphincters, and two terminal branches, the perineal nerve and the dorsal nerve of the penis or clitoris. Upon entering the ischiorectal fossa, the nerve and vessels enter a fascial canal on the surface of the obturator internus (the pudendal or Alcock’s canal). The two fossae communicate with each other posteriorly behind the rectum.
A tumor in this area manifests itself with pressure symptoms in the left or right perianal area, a sense of fullness and/or palpation of a mass in the same site, and difficulty on defecation due to pressure on the rectum on the side of the growing mass.
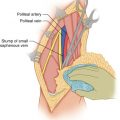
A posterior approach is recommended, with the patient in a prone position and the buttocks separated by the application of tapes on each side fastened on the edge of the operating table. The puncture point of a needle biopsy or previous biopsy incision is circumscribed with an elliptical incision extending laterally to the ischial tuberosity and medially to the coccyx. For large tumors, the incision is extended along the midline of the posterior surface of the sacrum to the approximate level of the S2 vertebra (Fig. 57.1). Flaps are developed on the surface of the gluteus maximus laterally to the ischial tuberosity and medially to the opposite sacral edge, guided also by the palpatory evidence of the tumor. One starts obliquely dividing the muscle fibers of the gluteus maximus (tending to stay away from the tumor) and then, upon reaching the sacrotuberous ligament, entering the ischiorectal fossa through the tendinous fibers of this ligament. Some blunt finger dissection is initially done, providing palpatory evidence of the lateral aspect of the tumor and guiding the dissection, usually with cautery, through the muscular origin of the maximus into the ischiorectal fossa. The medial flap is then developed to the contralateral edge of the coccyx, dividing the origin of the maximus from the coccygeal edge and cutting through the anococcygeal raphe (Fig. 57.2). If the tumor does not extend beyond the contralateral coccygeal edge, the coccyx may be divided across the sacrococcygeal joint and the dissection continued along the ipsilateral sacral edge (Fig. 57.3). Clamps are applied to the connective tissue on the exposed surface of the tumor, with care to avoid crushing tumor tissue and possibly contaminating the field with tumor cells. With Metzenbaum scissors, dissection continues around the tumor tissue leaving a layer of adipose-connective tissue on the tumor surface. The clamps are reapplied on the layer of normal-appearing tissue on the tumor surface close to the line of dissection, with malleable retractors providing adequate countertraction for accurate dissection with cautery or with Metzenbaum scissors, which are acceptable in such a case because of the roundness of the plane of dissection.