(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
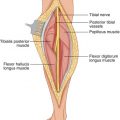
The inferior epigastric artery arises just above the inguinal ligament from the medial side of the external iliac artery and then runs upwards and medially along the medial side of the deep inguinal ring to the deep surface of the rectus abdominis. In its course, it raises a peritoneal fold, when viewed from inside, called the lateral umbilical fold, which should not be confused with the medial umbilical fold raised by the obliterated continuation of the umbilical artery after the takeoff of the superior vesical artery. The inferior epigastric artery pierces the transversalis fascia in the attenuated part of the posterior rectus sheath and ascends between the muscle and the posterior lamina of its sheath, supplying the muscle and anastomosing behind the middle of the length of the rectus with the superior epigastric artery (the terminal branch of the internal mammary) and lower posterior intercostal arteries. At the deep inguinal ring, the ductus deferens in the male or the round ligament of the uterus in the female lies lateral to and hooks around the inferior epigastric artery. Muscular and cutaneous branches from the inferior epigastric arteries, such as the cremasteric artery in the male or the artery of the round ligament of the uterus in the female, supply the anterior abdominal wall near the origin of this artery. A pubic branch descends from either the lateral or the medial side of the femoral ring, to anastomose with the pubic branch of the obturator artery. The deep iliac circumflex artery, a separate branch of the external iliac artery, arises a little below the inferior epigastric, immediately above the inguinal ligament from the lateral aspect of the external iliac artery. It turns to the anterior superior iliac spine, lying just above the inguinal ligament within a fascial canal formed by the iliac and transversalis fasciae. The inferior epigastric vein, a tributary to the external iliac vein on its medial side just above the level of the inguinal ligament, collects the venous blood from the inferior half of the ipsilateral rectus abdominis muscle. The pubic vein links the obturator vein and the posteromedial side of the external iliac vein. The external iliac vein receives the deep circumflex iliac vein on its lateral side, just above the level of the inguinal ligament. The inferior epigastric vessels are important in a wide range of procedures in the lower abdomen, as discussed below.
Ilioinguinal (Radical Groin) Dissection
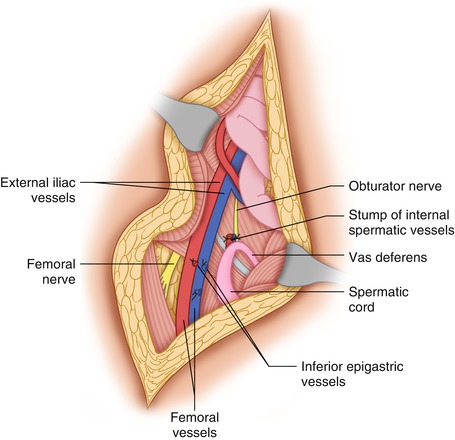
For in-continuity exposure and dissection of the femoral, iliac, and obturator nodes following the mobilization of the inguinal lymph nodes in the superficial groin dissection part of ilioinguinal dissection, the external oblique aponeurosis is divided from a point about two to three fingerbreadths superomedial to the anterior superior iliac spine down to the inguinal ligament about 1–2 cm lateral to the femoral artery. The inguinal ligament itself is also divided, along with the internal oblique, the transversus abdominis, and the transversalis fascia. After division of the inguinal ligament and mobilization of the peritoneum in a superomedial direction, while the lymph nodes over the external iliac vessels are exposed, the inferior epigastric artery is exposed, ligated, and divided at its origin, and the inferior epigastric vein is also ligated and divided close to its entry into the external iliac vein (Figs. 44.1 and 44.2). It is then possible to retract the medial portion of the abdominal wall musculature and expose the external iliac lymph nodes, which are dissected off the peritoneum anteriorly and medially and off the surface of the external iliac artery and vein posteriorly. The peritoneum is displaced superiorly to the point that the ureter is exposed as it courses over the bifurcation of the common iliac artery into the external iliac and internal iliac arteries. The peritoneum and bladder are medially displaced, thus exposing the obturator lymph nodes located between the external iliac vein anteriorly and the obturator nerve and vessels posteriorly. The obturator nerve follows a course from a position lateral to the internal iliac vessels on the obturator internus fascia to the obturator foramen; the obturator vessels are located immediately posterior to the obturator nerve. The obturator lymph nodes are found between the external iliac vein anteriorly and the obturator nerve and vessels posteriorly, and between the internal iliac vessels superiorly and the obturator foramen inferiorly. As the obturator nodes are mobilized in the plane between their medial side and the urinary bladder, one exposes again the inferior epigastric vessels as they are about to start a course on the posterior aspect of the ipsilateral rectus abdominis. These vessels are again ligated and divided. Therefore, to obtain in continuity exposure of the inguinal, external, and common iliac and obturator lymph nodes, it is crucial to ligate and divide the inferior epigastric vessels close to their origin from the external iliac vessels and also at the point where they enter the posterior aspect of the ipsilateral rectus abdominis. In effect, a segment of these vessels is removed en bloc with the external iliac and obturator lymph nodes. There should be no concern for an incisional postoperative hernia after this type of in continuity ilioinguinal dissection, because the muscular layers of the internal oblique and transversus abdominis are approximated in layers with a continuous suture of an absorbable material, and the external oblique aponeurosis with a continuous suture of nonabsorbable material such as Prolene (in recent years we have used absorbable material more often without ill effects). The inguinal ligament is reconstructed as the external oblique aponeurosis is approximated. The portion of the inguinal ligament lateral to the femoral artery is sutured to the iliac fascia, taking care to avoid the femoral nerve, which lies immediately behind the iliac fascia. It is therefore desirable to define the edge of the iliac fascia at a point just below the inguinal ligament, where it actually becomes attenuated, and to clearly expose and protect the femoral nerve behind it. On the medial side of the femoral vessels, the inguinal ligament is approximated to Cooper’s (pectineal) ligament with interrupted sutures of nonabsorbable material, which are first placed and then tied. Thus the repair of this incision for the in continuity exposure and removal of the inguinal and deep (iliac-obturator) nodes is in effect a Cooper’s ligament repair, which is unlikely to give rise to a postoperative incisional inguinal hernia in this area. In several hundred cases of radical groin dissection using this approach, we have seen no patients with postoperative incisional hernia in the groin.
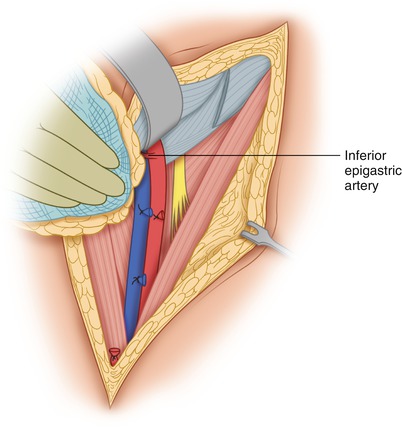
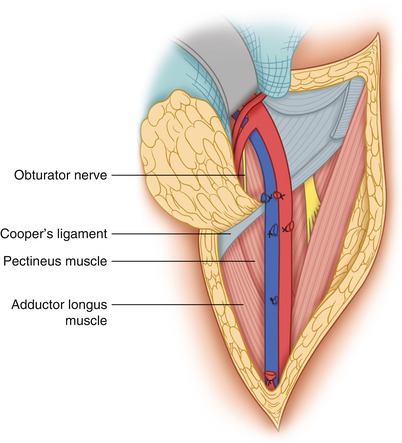
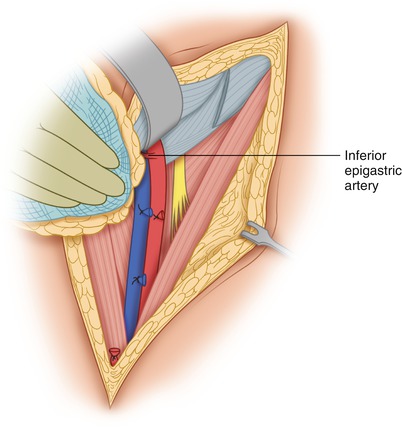
Fig. 44.1
The inferior epigastric artery is exposed
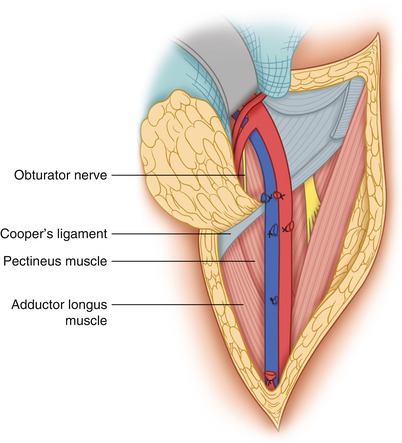
Fig. 44.2
The inferior epigastric artery and vein have been ligated and divided
The Abdominoinguinal Incision
Resection is possible (and usually easy) with an abdominoinguinal incision in surgery for tumors with fixation to the wall of the lesser pelvis, tumors occupying the iliac fossa, tumors involving the iliac vessels with possible extension behind the inguinal ligament, or those involving the pubic bone and the adductor muscles. This incision involves a lower midline incision from just above the umbilicus to the pubic symphysis, which then is extended to the right or left side transversely, according to the location of the tumor (i.e., from the pubic symphysis to the mid-inguinal point and then vertically into the femoral triangle). The subcutaneous tissue is divided in the transverse part of this incision, exposing the attachment of the anterior rectus sheath and muscle to the pubic crest. The anterior rectus sheath and ipsilateral rectus abdominis muscle are divided off the pubic crest. The inguinal ligament is divided at the pubic tubercle. The spermatic cord in the male can be extricated from the inguinal canal by dividing from inside the floor of the inguinal canal, mobilizing medially the spermatic vessels and the ductus deferens. The dissection behind the inguinal ligament is carried laterally. First, the inferior epigastric vein is ligated and divided at its entry into the external iliac vein and the inferior epigastric artery is then ligated and divided at its origin from the external iliac artery (Fig. 44.3). More laterally, the inguinal ligament is detached off, at its lateral third, from the iliac fascia to which it is fused. The deep iliac circumflex vessels are ligated and divided at their origin only in the presence of tumor in the iliac fossa descending behind the inguinal ligament. This incision allows the in-continuity exposure of the common iliac, external iliac, and femoral vessels and a continuous exposure of the iliac fossa and the iliopsoas muscle to the insertion of the iliopsoas in the lesser trochanter. Therefore, in the abdominoinguinal incision, the ligation and division of the inferior epigastric vessels is also crucial. The difference between this procedure and that of the ilioinguinal (radical) groin dissection is that in the ilioinguinal dissection, the division of the inferior epigastric vessels is from lateral to medial, whereas in the abdominoinguinal incision, the direction is from medial to lateral. The abdominoinguinal incision includes a lower midline abdominal incision and provides far greater exposure through a transverse division of the ipsilateral rectus abdominis and its sheath off the pubic crest.