(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
The lymphatic system is embryologically related to the venous system, so lymphatic channels and nodal basins tend to follow the course of the veins. There is also a functional cooperation between the two systems, both of which are concerned with the elimination of waste products or extraneous materials from the tissues.
The cervical lymph nodes are classified into nodal groups according to anatomic location and into surgical levels of node dissection according to the roughly sequential involvement of nodal groups by a regionally metastasizing tumor arising in the head. Thus, the submental lymph nodes are located in the middle of the upper neck between the anterior bellies of the digastric muscles and the hyoid bone. The submandibular nodes are located on each side around the submandibular gland, in the space between the anterior and posterior bellies of the digastric muscle. The submandibular and submental lymph nodes constitute level I of node dissection. The lymph nodes along the internal jugular vein are distinguished into the upper group, located in the space between the skull and hyoid bone (level II or jugulodigastric nodes); the middle jugular group, between the hyoid bone and the omohyoid muscle (level III); and the lower jugular group (level IV), continuing to the level of the clavicle at the junction of the internal jugular and subclavian veins. The posterior triangle nodes (level V) are located in the space between the posterior border of the sternocleidomastoid, the anterior edge of the trapezius, and the middle third of the clavicle. The anterior triangle nodes (level VI) are bound by the hyoid superiorly, the jugular notch of the sternum inferiorly, and the sternocleidomastoid laterally (Fig. 12.1). Outside the usual boundaries of the neck are other nodal groups that sometimes become involved and are dissected, such as the parotid, preauricular, postauricular, and suboccipital nodes.
Fig. 12.1
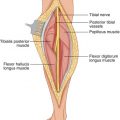
The sternocleidomastoid divides the neck into anterior and posterior triangle
Knowledge of the fascial layers of the neck is important in performing a neck dissection. The superficial cervical fascia is a layer that includes the subcutaneous fat and platysma muscle. More prominent in the lateral aspect of the neck, extending from the side of the mandible to below the clavicle, it is attenuated toward the midline of the neck and posteriorly (Fig. 12.2). The deep cervical fascia is divided into the investing layer and the pretracheal and prevertebral layers. The investing layer ensheathes the trapezius muscle and continues forward to enclose the sternocleidomastoid, extending to the midline; it is attached to the hyoid bone. The pretracheal layer encloses the trachea, thyroid, and esophagus. The prevertebral layer covers the prevertebral muscles medially, and more laterally covers the scaleni, levator scapulae, splenius, and semispinalis capitis, presenting a tubular extension encompassing the brachial plexus and the subclavian artery and vein behind the clavicle and into the axilla. The carotid sheath is a condensation of the three layers of the deep fascia enclosing the carotid artery and vagus nerve, with a lateral extension surrounding the internal jugular vein.
Fig. 12.2
The platysma muscle is thicker in the lateral side of the neck extending between the mandible and the clavicle
The classification of the nodal group into various levels has only relative value, determined from the perspective of the head and neck surgeon. Thus, level I nodes are affected in the submandibular group by primary lesions of the lips, buccal mucosa, tongue, anterior face; in the submental group, they are affected by lesions of the lips and chin. Oropharyngeal tumors present with metastases to the internal jugular groups (levels II, III, IV), whereas nasopharyngeal lesions involve the posterior triangle (level V). Thyroid cancer often involves the anterior compartment nodes (level VI), although it also can extend laterally.
Types of Neck Dissection
A radical neck dissection includes the removal of level I to level V nodes, en bloc with the sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve. It is performed in patients with large, palpable cervical nodes contiguous with these structures. A modified radical neck dissection (also called a functional neck dissection) is usually possible despite the presence of palpable nodes: a thorough dissection of the nodes is performed, and clean planes are used to skeletonize and preserve one or more of these three anatomical structures. In selective node dissection, one or more nodal groups are omitted from the procedure of a radical or modified radical neck dissection on the perception that the omitted nodal groups are out of the direction of spread of the particular primary lesion in the head and neck area, or they are too far from palpably involved nodal groups. The dissection of a whole nodal group that contains normal-appearing nodes may indicate that the dissection is complete, as it is uncommon for tumor cells to bypass a whole nodal group in the line of spread and metastasize to the next group. A supra-omohyoid dissection is limited to the removal of level I to level III nodes; a lateral dissection includes the dissection of level II to level V nodes.
Sentinel Node Biopsy
The theoretical basis of the sentinel node biopsy has been attributed to the orderly, sequential progression of the lymph flow through the regional nodes by tumor cells, but it is known that often the spread of a tumor within a nodal basin is not anatomically orderly, in the sense of involving successively all anatomically contiguous nodes. It is now considered a fact that cutaneous lymphatic vessels from a certain area of skin, as they approach the nodal basin, come together to form fewer, stouter lymphatic channels (usually one channel, or less often two or three), with each channel entering one lymph node—the sentinel node. By definition, then, a sentinel node is the first lymph node encountered by lymphatic channels draining a certain skin area, and therefore the first node to subject the lymphatic drainage from this particular area of skin to the filtering, clearing function of a lymph node—which includes the trapping of malignant cells. Lymph nodes are inefficient in destroying trapped malignant cells, however, often allowing their local growth and later passage into higher echelons of nodes and, at the base of the neck, into the bloodstream, although entry into the venous side of the bloodstream by tumor cells is also known to occur at the primary site. Removal of the sentinel node and careful pathologic examination should detect any focus of metastatic tumor if metastatic cells have lodged successfully in the regional nodal basin. Multiple sections through the sentinel node and the use of routine staining, immunohistochemistry, and the exquisitely sensitive method of reverse transcriptase polymerase chain reaction (RT-PCR) (though its clinical significance is disputed) should help to detect the presence of any tumor focus. In a large series dealing with all nodal basins, 72 % of patients had one sentinel node, 20 % had two sentinel nodes, and 8 % had three or more [1].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree