Hand Washing
The simple act of hand washing with soap has been associated with significant decreases in the prevalence of many common infections, in both low- and highincome countries. The most common infections averted globally by the introduction of hand hygiene practices are diarrheal diseases, primarily among young children, and acute respiratory infections (
Table 4-1). An estimated 1.5 million children die due to diarrhea annually,
2 and pneumoniaassociated diseases lead to the premature deaths of approximately 1.4 million children each year.
3 Other important sources of morbidity prevented by hand washing include helminth infections in sub-Saharan Africa and other tropical locales, and conjunctivitis, which is highly transmissible.
A person’s hands can become contaminated with pathogens after coming into contact with human or animal feces, bodily fluids (e.g., nasal excretions), or foods and liquids. These pathogens can then be transmitted from person to person, through either direct contact (e.g., touching other people) or indirect contact (e.g., touching surfaces or fomites).
4 Hand washing works by removing pathogens
from the hands and preventing disease transmission, but how it works depends on the techniques and products used. Hand washing with water dislodges visible dirt from the hands through rubbing and friction but does not break down the grease and oils on the hands that carry many pathogens; thus this technique is not recommended.
4,
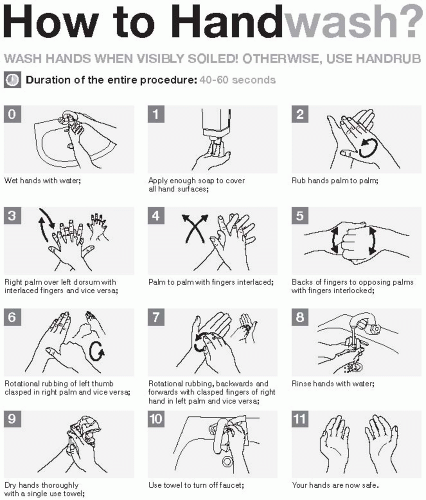
5 Using soap to wash hands is more effective, as it increases the time spent washing hands; in addition, most soaps are detergents and will actively break down grease, oils, and other organic matter. When hands are washed properly (
Figure 4-1), all soaps are equally effective at removing pathogens.
4 Antimicrobial soaps, alcohol-based rubs, and other specialized products, including chlorhexadine, chloroxylenol, and triclosan, have direct antimicrobial activity and have been developed to increase the effectiveness of hand washing, particularly in healthcare settings, but are not widely available to the general population in many settings.
5 Critical times for hand washing to prevent the spread of infections include after using the toilet, after changing dirty diapers or cleaning a child, and before handling any food.
4Additional components of hand washing include the quality of the water used and the methods for drying hands after hand washing. The efficacy of hand washing with soap in decontaminating hands can be reduced if clean water is not used. Waterborne pathogens may readily be found in available water supplies, including bacteria
(Campylobacter jejuni and
coli, Escherichia coli, Legionella species,
Shigella typhi, and
Vibrio cholerae, among others), viruses (e.g., adenoviruses, enteroviruses, hepatitis A, rotaviruses), protozoa
(Giardia lamblia, Toxoplasma gondii, Cryptosporidium parvum), and helminths
(Dracunculus medinensis, Schistosoma species).
6 Thus, even if soap is used, contamination of hands may result from contaminated water supplies. A particular problem is the use of communal bowls of water for hand washing prior to eating, which may promote contamination and infection rather than prevent it. In these cases, washing hands under running water would be preferable. A second source of contamination is hand drying. Hand drying may be a problem in settings where clean towels or other wiping materials are not available, and touch-contact may undo the effects of hand washing. In these cases, air drying would be preferable to using dirty or communal towels.
A number of studies have demonstrated that hand washing with soap reduces the quantity of microbes on the hands far more than rinsing with water alone.
7,
8 In one study, the prevalence of bacteria of fecal origin (primarily
Enterococcus and
Enterobacter spp.) was significantly reduced from 44% to 23% after washing with water alone, and to 8% after washing with plain soap and water.
9 The length of time spent hand washing is also important. In one study, bacterial counts on the skin were reduced by 0.6-1.1 log
10 after hand washing with soap and water for 15 seconds and by 1.8-2.8 log
10 after hand washing for 30 seconds.
10The importance and effectiveness of hand washing in reducing infection and disease were first recognized by Ignaz Semmelweiss and Oliver Wendell Holmes in the mid-19th century, when they hypothesized that puerperal fever acquired in maternity wards was transmitted directly by the hands of healthcare workers.
1 The solution was hand washing with a chlorinated lime solution before each patient encounter; upon initiation of this practice among healthcare providers, mortality rates dropped precipitously. Since then, many studies have evaluated the effectiveness of hand washing in preventing
disease. The most extensive and strongest evidence comes from studies of diarrhea prevention.
11,
12,
13,
14,
15,
16,
17,
18 and
19 These community-based studies suggest that hand washing reduces the incidence of diarrhea by 32-47%.
11,
13,
18 In addition, significant evidence shows that hand washing is effective in reducing acute respiratory infections by an estimated 24%.
20 The evidence for other infections is not as extensive or robust, but does suggest that hand washing is effective in reducing the incidence of helminth infections,
21,
22,
23 and
24 particularly ascariasis and trichuriasis, and eye infections.
25The importance of hand washing has also been recognized and extensively studied in healthcare settings, where acquisition and transmission of nosocomial infections represent a significant source of patient morbidity and mortality.
26 Poor hand hygiene among healthcare workers has been associated with many outbreaks in healthcare settings, and most studies have shown a transient improvement in infection rates associated with better adherence to hand washing recommendations.
5 Consequently, hand washing is the cornerstone of infection control in healthcare settings. Hand hygiene guidelines for healthcare settings were first promulgated in the United States by the Centers for Disease Control and Prevention in the 1980s,
27 and updated in 1996
28 and 2002.
29In addition to being an effective method for reducing the incidence of disease, hand washing has been found to be the most cost-effective intervention for diarrheal diseases. To avert a single disability-adjusted life year (DALY) with hand washing costs $3.35, compared with $11.15 for
latrine promotion, $527-2001 for breastfeeding promotion programs, and $1658-8274 for cholera immunizations.
4Despite the demonstrated efficacy of proper hand hygiene measures in decreasing infection in both community and healthcare settings, hand washing with soap has not been widely adopted. Observed rates of hand washing with soap around the world range from zero to 34%.
4 The availability of soap is not the issue, as it is widely available worldwide—in one study, 95% of households in Uganda, 97% of households in Kenya, and 100% of households in Peru were found to have soap.
4 In many areas, however, soap is primarily used for laundry, bathing, and dishwashing, and less often for hand washing. Lack of knowledge, the cost of soap for additional uses, and the availability of water may all influence hand washing practices. Increasing initiation and sustained adoption of proper hand hygiene will require an increase in the awareness of the necessity of hand washing with soap and motivation to change individual behaviors and community norms. In an effort to promote proper hand hygiene, the United Nations declared October 15 to be Global Handwashing Day.
4 In 2008, the inaugural Global Handwashing Day focused on young children and activities to mobilize community support for childhood education on the utility and effectiveness of routine hand washing.
4,
30The success of hand hygiene requires constant and continuous dedication on the part of individuals to implement proper techniques at all critical times. Health education campaigns promoting hand hygiene will require the same level of vigilance and commitment to maintain awareness of the risks in a community and improve health outcomes. Hand hygiene has been shown to be one of the simplest, yet most difficult human behaviors to affect.
Food Safety
Measures to ensure food safety are implemented to protect against foodborne or waterborne infections. Foodborne or waterborne infections are some of the most common infections, causing an estimated 2.2 million deaths annually, with the majority of the mortality occurring among children.
31 Infections occur through ingestion of food or water that is contaminated with pathogenic microorganisms. Contamination may occur either naturally or from fecal-oral transmission from an infected individual who is handling the water source or preparing the food. Infections can be caused by bacteria, parasites, or viruses (
Table 4-2) and generally result in diarrhea, fever, and vomiting. Food safety has increasingly been recognized as an essential measure in public health. To protect the world’s population from foodborne or waterborne infections, the World Health Organization has developed the Five Keys to Safer Food, which include: (1) keeping foods clean, (2) separating foods, (3) cooking food thoroughly, (4) keeping food at safe temperatures, and (5) using safe water and raw materials.
32 These prevention measures are intended to prevent contamination of food and water and to kill microorganisms or inhibit their growth if contamination does occur.
Keep Clean
Some food or water may naturally contain microorganisms; other food and water may become contaminated during the process of preparation. Microorganisms can reside in human or animal feces or on the feet, mouths, or skin of animals and pests (e.g., rats, mice, birds, cockroaches). Food or water can become contaminated with these microorganisms if they come into contact with surfaces containing infected fecal matter or animals and pests. Keeping the preparation process clean ensures that food or water does not become contaminated or, if already contaminated, ensures that cross-contamination to other food or water does not occur. Consequently, the individual and others in the household consuming the food or water will not become infected.
Keeping clean encompasses two components: the individual preparing the food and the surfaces and equipment being used. Keeping the individual clean involves washing hands before handling food, during food preparation, and anytime after going to the toilet, handling garbage, changing diapers, or playing with pets. Hands should especially be washed after slaughtering animals and after handling raw meat or poultry. Hands should be washed with soap and water (refer to the earlier section on hand washing for proper techniques) or, if soap is not available, with coal ash. Studies of hand washing interventions have estimated that increasing the frequency of hand washing can reduce the incidence of diarrheal episodes by approximately 32-47%.
11,
13,
18Keeping surfaces and equipment clean involves washing and sanitizing them before preparing food and after they have any contact with raw meat or seafood. Sanitizing is distinct from cleaning, in that the former implies the process of disinfecting or killing microorganisms rather than simply clearing debris.
To sanitize a surface or piece of equipment, it can be washed in boiling water or with a sanitizing solution (mix 5 mL of household bleach with 750 mL of water). Keeping surfaces and equipment clean also involves protecting them from insects, pests, and other pets or domestic animals.
Separate Raw and Cooked Foods
Raw food—especially meat, poultry, and seafood—can contain microorganisms that can be transferred onto other foods during food preparation and storage. Cross-contamination of other types of food can be prevented by keeping them separate while shopping for, refrigerating, preparing, and storing food. While preparing food, crosscontamination can be prevented by using separate equipment and utensils for meat, poultry, seafood, and other types of food, and for raw and cooked food.
Cook Thoroughly
Most microorganisms do not survive at high temperatures; therefore cooking to temperatures greater than 70°C (160°F) can render contaminated food safe for consumption. At these temperatures, almost all dangerous microorganisms are killed within 30 seconds. Microorganisms generally reside on the outer surfaces of food, particularly intact pieces of meat, so cooking foods thoroughly to these temperatures is not necessary and eating meat with a red center can be safe. Minced meat, rolled roasts, and poultry are exceptions: they need to be cooked thoroughly, as microorganisms can be found on the surfaces as well as in the center. To ensure proper
cooking temperatures, liquids should be brought to a boil and a thermometer should be used for meats (see
Table 4-3 for instructions on how to use a thermometer and proper cooking temperatures).
Keep Food at Safe Temperatures
Microorganisms require the right environment to thrive, and this generally occurs at temperatures between 5°C and 60°C. Keeping temperatures below 5°C or above 60°C can slow and even stop microorganisms from multiplying; therefore keeping food at room temperature for longer than 2 hours should be avoided. Food should be thawed in the refrigerator, kept hot before serving, and refrigerated as soon as possible after eating to keep it at a safe temperature. If no refrigerator is available, a hole can be dug in the ground for storage or cold water can be used. To decrease the cooling time of cooked food, it should be stored in smaller quantities. As microorganisms can still grow at low temperatures, food should not be stored in the refrigerator for longer than 3 days and should not be reheated more than once.
Use Safe Water and Raw Materials
Raw materials may be contaminated with microorganisms and, therefore, may contaminate any food that they are prepared with. Purchasing fresh foods and clean water or sanitizing food and water in the home can minimize this risk of contamination. For example, purchasing foods that have been processed, such as pasteurized milk and cheeses, can reduce the risk of purchasing contaminated products. In addition, washing fruits and vegetables with clean water, especially if they will be consumed raw, can reduce the risk of consuming contaminated products.
Water is used in many steps of food preparation and consumption: it is used for washing foods, as an additive to many liquid-based foods, for cleaning hands and cooking equipment, and to make up drinks or ice. Consequently, it is important to use safe water in all steps of food preparation and consumption. If safe water is not available in the household and cannot be purchased, individuals can inactivate microorganisms by boiling the water or using chlorine (3-5 drops of chlorine to 1 liter of water), or can physically remove these organisms by filtering the water.
33 Studies have found that use of improved water sanitation procedures by individuals can significantly reduce contamination of water sources
34,
35 and
36 and decrease the risk of diarrheal disease in the household by as much as 35%.
13By following these procedures, individuals can effectively remove significant sources of microorganisms and protect themselves against foodborne and waterborne infections. However, these procedures must be followed every day to be effective, as any lapse can result in infection.
Male Condoms
Male condoms have been used for more than 400 years
37 and remain a highly effective means of protection against sexually transmitted infections (STIs).
38 STIs can be transmitted through either vaginal or anal sex and may be caused by viruses, bacteria, and parasites (
Table 4-4). STIs mainly fall into two categories: discharge diseases and genital ulcer diseases. The infectious agents of discharge diseases, including human immunodeficiency virus (HIV), gonorrhea, chlamydia, and trichomoniasis, are present in genital secretions (semen or vaginal fluids) and are transmitted through contact of infected secretions with a partner’s mucosal surfaces (i.e., urethra, rectum, vagina, or cervix). The infectious agents of genital ulcer diseases, including genital
herpes (HSV), syphilis, and chancroid, are present in sores and ulcers or may be shed into secretions and are transmitted through contact with infected lesions. Another STI, human papillomavirus (HPV), which is the cause of cervical cancer and genital warts, is transmitted through contact with infected cell surfaces, even in the absence of fluid or tissue exchange.
Male condoms provide protection against STIs by putting a physical barrier between surfaces (i.e., between penis and vagina or between penis and rectum). They are typically made of latex and are impermeable to the smallest STI pathogen.
38 Condoms can provide different levels of protection depending on the mode of transmission. These products protect against discharge diseases by preventing infected bodily fluids from coming into contact with mucosal surfaces. When used properly (
Box 4-1) and in the absence of breakage or leakage, condoms completely contain male pre-ejaculate and ejaculate and completely cover the male urethra. As a consequence, they provide a high level of protection against discharge diseases for uninfected male and female partners.
38 Condoms protect against genital ulcer diseases and HPV by preventing contact between infected and uninfected skin and mucosal surfaces.
38 As sores or infected cells may be present outside of the area protected by the condom, however, condoms may provide less protection against genital ulcer diseases or HPV for uninfected partners.
38Efficacy—that is, the protection afforded by condoms under ideal conditions—cannot be measured and evaluated using randomized controlled trials, as it would be unethical to discourage their use in one group. Instead, effectiveness—that is, the protection afforded under actual conditions of use—must be assessed through self-report in observational studies. Under these circumstances, the degree to which condoms protect against STIs depends not only on the properties of the condom but also on how properly and consistently condoms are used by the individuals in the study.
38 In such studies, because of the difficulty in quantifying partial condom use, effectiveness is typically measured by comparing the incidence
of STIs among individuals who report never using a condom with the incidence among individuals who report always using a condom. Many studies are conducted among discordant couples, where one partner is infected and one partner is not, or among individuals with high exposure to STIs.
The effectiveness of condoms has been best evaluated for heterosexual transmission of HIV, for which estimates indicate that consistent and correct use of condoms can reduce the risk by approximately 80%.
39 Estimates of effectiveness for anal sex among heterosexual and homosexual partners are limited, but may be lower given the potentially greater risk of breakage and slippage during anal sex as compared to vaginal sex.
40 Studies have also demonstrated that condoms are effective in reducing the risk of gonorrhea (49-90%)
38,
41,
42 and HSV-2 (30%).
43 Studies of HPV have generally found that condoms do not result in a reduced risk of HPV infection; however, condom use has been found to reduce the risk of genital warts in men and cervical neoplasia in women.
38,
44 Studies for chlamydia, trichomoniasis, chancroid, and syphilis have produced inconclusive results or have been insufficiently rigorous to draw conclusions.
38Condoms are most effective when used correctly and consistently with all types of sexual partners, including both casual and long-term partners. For infections that are easily transmitted, such as gonorrhea, failure to use a condom during even one sexual act may result in exposure and infection.
38 Incorrect use and behaviors that compromise the integrity of the condom may increase the risk of breakage, thereby decreasing its effectiveness. In the United States, studies of condom slippage and breakage during use have estimated the frequency of breakage to range from 0.4% to 2.3% and the frequency of slippage to range from 0.6% to 1.3%. Combined estimates of failure (breakage and slippage) range from 1.6% to 3.6%.
38 Instruction on how to correctly put on a condom and other practical issues related to their correct use—including the need to protect condoms from sharp objects such as jewelry, fingernails, or teeth; the need to avoid oil-based lubricants; and the ability to choose a condom that is the right size—can improve an individual’s ability to use condoms effectively.
45,
46Consistent condom use with both heterosexual and same-sex partners can be a challenge in many settings. A national survey in the United States in 2002 reported that among heterosexual men and women aged 15-44 years, only 28.6% of men and 27.2% of women used condoms some or all of the time in the past 4 weeks,
47 although use has been increasing over the past two decades.
38 A review of surveys of men who have sex with men (MSM) in 44 low- and middle-income countries revealed that slightly more than half of MSM reported using a condom in their last sexual encounter with a man.
48 Rates of condom use vary with cultural setting, with the lowest rates reported in South and Southeast Asia (38%), intermediate rates reported in sub-Saharan Africa (57%) and Eastern Europe and Central Asia (58%), and the highest rates reported in Latin America (73%).
48Practical, individual, social, cultural, and religious factors may all influence consistent condom use. Practical considerations include cost and availability. While condoms are relatively inexpensive, even a minimal cost can be prohibitive for individuals in low- and middle-income settings.
49 For individuals who can afford condoms, it can be embarrassing to actually purchase them. This embarrassment can significantly negatively impact consistency of condom use.
50 Indeed, neighborhoods that have a greater number of stores requiring assistance from store personnel to purchase condoms are more likely to have higher rates of HIV, STIs, and teen pregnancy.
51Consistent condom use also requires individuals to initiate and negotiate their use with partners. This process can be hindered by substance use
49,
52 (use of alcohol or drugs often precedes sexual activity), by partner type, and, within heterosexual partnerships, by gendered power imbalances.
53 For example, in relation to partner type, condom use may be seen as appropriate when visiting a sex worker
54 but not within a more established partnership for both heterosexual individuals and MSM.
52,
55 Among heterosexual adolescents, a similar dynamic occurs where condoms are used with partners who are “dirty,” and young women who have condoms or suggest using them are stigmatized for being sexually experienced.
56 Younger age (e.g., younger than age 24) is itself associated with condom use that is more likely to be inconsistent.
57,
58Cultural norms or religious beliefs or traditions, such as those that suggest that condom use can make men “ill” or waste “bodily powers,”
54 or that flatly forbid condom use given its association with preventing procreation, can also discourage consistent condom use. At the same time, structural interventions that turn condom use into a norm, including several measures that have been implemented among sex workers,
59 have been associated with decreased HIV incidence.
Despite the practical, behavioral, and societal challenges discussed previously, condoms remain perhaps the most valuable preventive measure against most STIs. When used consistently and correctly, they are highly effective. They are relatively
inexpensive, and countries and communities can have a demonstrated positive impact in ensuring their broad accessibility and acceptability.
60 In the absence of vaccines for most STIs, they remain an essential and important prevention tool.