Early History of Infectious Disease: Epidemiology and Control of Infectious Diseases
Kenrad E. Nelson
Carolyn Masters Williams
INTRODUCTION
Epidemics of infectious diseases have been documented throughout history. In ancient Greece and Egypt, accounts describe epidemics of smallpox, leprosy, tuberculosis, meningococcal infections, and diphtheria.1 The morbidity and mortality of infectious diseases profoundly shaped politics, commerce, and culture. In epidemics, no one was spared. Smallpox likely disfigured and killed Ramses V in 1157 BCE, although his mummy has a significant head wound as well.2 At times, political upheavals exacerbated the spread of disease. The Spartan wars caused massive dislocation of Greeks into Athens, triggering the epidemic of 430-427 BCE that killed up to half of the population of ancient Athens.3 Thucydides’ vivid descriptions of this epidemic make clear its political and cultural impact, and provide valuable clinical details of the epidemic.4 Several modern epidemiologists have speculated about the causative agent. Langmuir et al.5 favor an influenza and toxin-producing Staphylococcus epidemic, while Morrens and Chu suggest Rift Valley fever.6 A third researcher, Holladay believes the causative agent no longer exists.7
From the earliest times, humans have sought to understand the natural forces and risk factors affecting the patterns of illness and death in society. These theories have evolved as our understanding of the natural world has advanced—sometimes slowly; sometimes, when there are profound breakthroughs, with incredible speed. Remarkably, advances in knowledge and changes in theory have not always proceeded in synchrony. Although wrong theories or knowledge has hindered advances in understanding, one can also cite examples of great creativity when scientists have successfully pursued their theories beyond the knowledge of the time.
THE ERA OF PLAGUES
The sheer magnitude and mortality of early epidemics are difficult to imagine. Medicine and religion both strove to console the sick and dying. However, before advances in the underlying science of health, medicine lacked effective tools, and religious explanations for disease dominated. As early communities consolidated people more closely, severe epidemics of plague, smallpox, and syphilis occurred.
The bubonic plague and its coinfections, measles and smallpox, were the most devastating of the epidemic diseases. In 160 CE plague contributed to the collapse of the Han Empire,8 and six years later the Roman Empire was ravaged by the Antonine Plague (165-180 CE), which likely killed both coemperors Lucius Verus (130-169 CE) and Marcus Aurelius (121-180 CE) along with 5 million others.9, 10 Plague and other communicable diseases flourished in the cities of the Roman Empire and surely contributed to its final demise.11 The devastating Justinian plague (541 CE) was caused by a distinct strain of Yersinia pestis. This epidemic killed approximately 40% of Constantinople and heralded the end of the second plague era. From 700 CE until the massive epidemics of the 14th century, bubonic plague was much less common. However, the plague—or
Black Death, as it was then called—struck again in 1345 and swept across Europe. Starting in the lower Volga, it spread to Italy and Egypt in 1347 on merchant ships carrying rats and fleas infected with the plague bacillus, Yersinia pestis.1 During the next five years (1347-1351), the Black Death killed 3 Europeans out of 10, leaving 24 million Europeans dead and causing a total of 40 million deaths worldwide.1, 12, 13 and 14 These waves of bubonic plague fundamentally affected the development of civilizations as well as imposed a genetic bottleneck on those populations exposed to the pathogen. In fact, Europeans may be able to attribute their lower susceptibility to leprosy and human immunodeficiency virus (HIV) to the selective pressure of bubonic plague.15 To survive in an ancient city was no small immunologic feat— and populations that had the immunologic fortitude had an advantage over others when exploration and colonization brought them and their pathogens together.11
Black Death, as it was then called—struck again in 1345 and swept across Europe. Starting in the lower Volga, it spread to Italy and Egypt in 1347 on merchant ships carrying rats and fleas infected with the plague bacillus, Yersinia pestis.1 During the next five years (1347-1351), the Black Death killed 3 Europeans out of 10, leaving 24 million Europeans dead and causing a total of 40 million deaths worldwide.1, 12, 13 and 14 These waves of bubonic plague fundamentally affected the development of civilizations as well as imposed a genetic bottleneck on those populations exposed to the pathogen. In fact, Europeans may be able to attribute their lower susceptibility to leprosy and human immunodeficiency virus (HIV) to the selective pressure of bubonic plague.15 To survive in an ancient city was no small immunologic feat— and populations that had the immunologic fortitude had an advantage over others when exploration and colonization brought them and their pathogens together.11
The first recorded epidemic of smallpox was in 1350 BCE, during the Egyptian-Hittite war.1 In addition to Ramses V, typical smallpox scars have been seen on the faces of mummies from the time of the 18th and 20th Egyptian dynasties (1570-1085 BCE). Smallpox was disseminated during the Arabian expansion, the Crusades, the discovery of the West Indies, and the colonization of the Americas. Mortality ranged from 10% to 50% in many epidemics. The disease apparently was unknown in the New World prior to the appearance of the Spanish and Portuguese conquistadors. Cortez was routed in battle in 1520 but ultimately proved victorious as smallpox killed more than 25% of the Aztecs over the next year.8 Mortality rates of 60-90% were described by the Spanish priest Fray Toribio Motolinia. He reported that 1000 persons per day died in Tlaxcala, with ultimately 150,000 total dead.16 Smallpox then traveled north across the Americas, devastating the previously unexposed Native American populations.11
At that time, there was a reasonable understanding of the epidemiology of smallpox transmission. At the least, it was appreciated that the skin lesions and scabs could transmit the disease. Survivors of the infection were recognized as being immune to reinfection after further exposure. The practice of inoculation, or variolation, whereby people were intentionally exposed to smallpox was practiced in China, Africa, and India centuries before the practice would be adopted in Europe and the Americas.17
Syphilis is another epidemic infectious disease of great historical importance. Syphilis became epidemic in the 1490s as a highly contagious venereal disease in Spain, Italy, and France. By the 1530s, the venereal spread of this infection was widely recognized in Europe.18 The name syphilis originated from the popular, and extremely long, poem by Girolamo Fracastoro “Syphilis sive morbus Gallicus.” Written in 1546, the poem recounts the causes of disease and the origin and treatment of syphilis.12, 18 Fracastoro describes the legend of a handsome young shepherd named Syphilis, who, because of an insult to the god Apollo, was punished with a terrible disease, “the French Disease”—or syphilis. The origins of venereal syphilis are debated. One theory proposes that it began as a tropical disease transmitted by direct (nonsexual) contact.18 In support of this theory, the causative organism, Treponema pallidum, was isolated from patients with endemic (nonvenereal) syphilis (bejel) and yaws. After the first accounts of syphilis appeared, it was reported to spread rapidly through Europe and then North America. In keeping with the hypothesis that syphilis was a recently emerged disease, mortality from syphilis was high in these early epidemics.11
EARLY EPIDEMIOLOGY
In Western medicine, Hippocrates (460-377 BCE) was among the first to record his theories on the occurrence of disease. In his treatise Airs, Water and Places, Hippocrates dismissed supernatural explanations of disease and instead attributed illness to characteristics of the climate, soil, water, mode of life, and nutrition surrounding the patient.2, 19, 20 and 21 It is Hippocrates who coined the terms endemic and epidemic disease to differentiate those diseases that are always present in a population (endemic) from those that are not always present but sometimes occur in large numbers (epidemic). It was Claudius Galen (131-201 CE), however, who codified the Hippocratic theories in his writings. Galen combined his practical experience caring for gladiators with experiments, including vivisections of animals, to study the anatomy and physiology of humans.22 His voluminous writings carried both his correct and incorrect views into the Middle Ages. It was more than 1000 years before Andreas Vesalius (1514-1564), who based his work on dissections of humans, was able to correct Galen’s errors in anatomy.22
That infectious diseases were contagious was recognized in early epidemics, but because knowledge of the true epidemiology of diseases was lacking, efforts to control the spread of such diseases
were flawed. Plague was recognized to be contagious; however, the control measures focused primarily on quarantine and disposal of the bodies and the possessions (presumably contaminated) of the victims. Although it was observed that large numbers of rats appeared during an epidemic of plague, the role of rats and their fleas was not appreciated.
were flawed. Plague was recognized to be contagious; however, the control measures focused primarily on quarantine and disposal of the bodies and the possessions (presumably contaminated) of the victims. Although it was observed that large numbers of rats appeared during an epidemic of plague, the role of rats and their fleas was not appreciated.
As far back as biblical times, leprosy was believed to be highly contagious. Afflicted patients were treated with fear and stigmatization. Given that leprosy progresses slowly, quarantine of cases late in disease likely had little effect on the epidemic spread. In the Middle Ages, lepers were literally stricken from society as leprosy became increasingly equated with sin. Some even required lepers to stand in a dug grave and receive the “Mass of Separation” from a priest after which they were considered “dead.” One example of a Mass of Separation reads as follows:
I forbid you to ever enter a church, a monastery, a fair, a mill, a market or an assembly of people. I forbid you to leave your house unless dressed in your recognizable garb and also shod. I forbid you to wash your hands or to launder anything or to drink at any stream or fountain, unless using your own barrel or dipper. I forbid you to touch anything you buy or barter for, until it becomes your own. I forbid you to enter any tavern; and if you wish for wine, whether you buy it or it is given to you, have it funneled into your keg. I forbid you to share house with any woman but your wife. I command you, if accosted by anyone while traveling on a road, to set yourself downwind of them before you answer. I forbid you to enter any narrow passage, lest a passerby bump into you. I forbid you, wherever you go, to touch the rim or the rope of a well without donning your gloves. I forbid you to touch any child or give them anything. I forbid you to drink or eat from any vessel but your own.23
Persons with leprosy, or suspected leprosy, were forced to carry a bell to warn others that they were coming (see Figure 1-1).
Fracastoro (1478-1553) was much more than just an author of the popular poem on syphilis. A true Renaissance man, he was also an astronomer and doctor. In his book published in 1546, De contajione, ontagiosis morbis et curatine (On Contagion, Contagious Diseases, and Their Treatment), he proposed the revolutionary theory that infectious diseases were transmitted from person to person by minute invisible particles.12, 24 Fracastoro conceived of the idea that infections were spread from person to person by minute invisible seeds, or seminaria, that were specific for individual diseases, were self-replicating, and acted on the humors of the body to create disease. Although his theory was revolutionary, Fracastoro did not realize that the seeds of a disease were microbes, and he held to ancient beliefs that they were influenced by planetary conjugation particularly “nostra trium superiorum, Saturni, Iovis et Martis” (“our three most distant bodies: Saturn, Jupiter, and Mars”). He postulated that the environment became polluted with seminaria and that epidemics occurred in association with certain atmospheric and astrologic conditions.12, 24 Fracastoro proposed three modes of transmission of contagious disease: by direct contact from one person to another, through contact with fomites (a term for contaminated articles still used today), and through the air. His theories were respected and certainly far ahead of their time. Fracastoro was able to persuade Pope Paul III to transfer the Council of Trent to Bologna because of the prevalence of contagious disease in Trent and the risk of contact with contaminated fomites.1 Nevertheless, it would take the discovery of the microscope 200 years later to prove his theories.
THE OBSERVATION AND CARE OF PATIENTS
Medical practice was gradually transformed by the introduction of disease-specific treatments during the Renaissance era. Peruvian bark, or cinchona, was imported into Europe for the treatment of malaria around 1630.25 Its active ingredient, quinine, was the first specific treatment for the disease. Based on the observation that smallpox disease conferred immunity in those who survived its ravages, intentional inoculation of healthy people to induce immunity was attempted. This process, which was known as variolation, was advocated by Thomas Jefferson (1743-1826), Benjamin Franklin (1706-1790), and Cotton Mather (1663-1728). Mather learned of it from a man he enslaved, Onesimus, who was inoculated with smallpox in a cut as a child in Africa.17
In 1796, Edward Jenner (1749-1823), based on the observation that milkmaids were immune to smallpox, greatly improved the process by substituting cowpox in place of the human pathogen. He performed the first vaccine clinical trial by inoculating 8-year-old James Phipps (1788-1853) with lesions containing cowpox (vaccinia virus) and later showed that the boy was immune to variolation, or challenge with variola virus.26 Thus was born the science of vaccination, which led eventually (180 years later) to the eradication of smallpox.26 Napoleon (1769-1821) showed his support by vaccinating his army, declaring that “anything Jenner wants shall be granted. He has been my most faithful servant in the European campaigns.”27
It is worthy of mention that other empiric attempts were proposed during the 1700s to induce protection by intentional inoculation, such as for measles (called morbillication) and syphilis. Neither of these efforts was successful, however.
Changes in the practice of clinical medicine in the 1600s began to differentiate diseases from one another. One of the earliest advocates of careful observation of patients’ symptoms and their disease course was the London doctor Thomas Sydenham (1624-1689). He classified various febrile illnesses plaguing London in the 1660s and 1670s in a book entitled Observations Medicae. Sydenham’s approach departed from that employed by Galen and Hippocrates, who focused on the individual and their illness rather than on trying to differentiate specific diseases. After Sydenham, the Italian physician Giovanni Morgagni (1682-1771) inaugurated the method of clinicopathologic correlation. His book De sedibus et causis morborum per anatomen indagatis (On the Seats and Causes of Diseases, Investigated by Anatomy), based on more than 700 autopsies, attributed particular signs and symptoms to pathologic changes in the tissues and organs. The influence of Sydenham and Morgagni on medicine can be seen in Benjamin Rush’s (1745-1813) description of dengue among patients afflicted in the 1780 Philadelphia epidemic:
The pains which accompanied this fever were exquisitely severe in the head, back, and limbs. The pains in the head were sometimes in the back parts of it, and at other times they occupied only the eyeballs. In some people, the pains were so acute in their backs and hips that they could not lie in bed…. A few complained of their flesh being sore to the touch, in every part of the body. From these circumstances, the disease was sometimes believed to be a rheumatism. But its more general name among all classes of people was the Breakbone fever.28
This new way of thinking about diseases, requiring careful clinical observation, differentiation, and specific diagnosis, led naturally to the search for specific, as opposed to general, causes of illness.
Expanding on the concept of careful clinical observation of individuals, epidemiologists in the 1800s observed unusual epidemics and performed controlled studies of exposed persons. Epidemiologic theories about the means of transmission of various infectious diseases often preceded the laboratory and clinical studies of the causative organisms. Peter Panum (1820-1885) recorded his observation of an epidemic of measles on the Faroe Islands in 1846.29 Measles had not occurred on these remote Scandinavian islands for 65 years. Remarkably, the attack rate among those younger than 65 years old was near 97%, but older persons were completely spared. This selectivity demonstrated that immunity after an attack of natural measles persists for a lifetime. Further, Panum described the mean 14-day incubation period between cases.29 Observations of outbreaks of mumps and other contagious diseases in isolated populations also contributed to the early understanding of the epidemiology of these diseases.30, 31
The epidemiology of bacterial diseases also progressed at this time. John Snow (1813-1858) performed classic epidemiology of the transmission of cholera in the mid-1850s, nearly 30 years prior to the identification of the causative organism.32 William Budd (1868-1953) demonstrated the means of transmission of typhoid fever and the importance of the human carrier in transmission
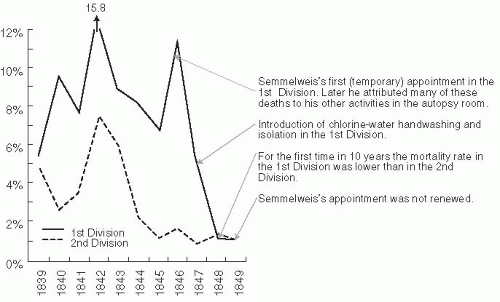
35 years prior to the isolation of Salmonella typhi.33 Ignatz Semmelweiss (1818-1865) demonstrated with a retrospective record review that an epidemic of puerperal fever, or childbed fever, in 1847 at the Vienna Lying-In hospital was due to transmission of infection on the hands of medical students and physicians who went from the autopsy room to the delivery room without washing their hands. In contrast, the women who were delivered by midwives, who used aseptic techniques (by immersing their hands in antiseptic solution prior to contact with the patient), had much lower rates of puerperal sepsis (Figure 1-2).34 Unfortunately, while Semmelweiss was correct, bacteria had not yet been identified and his theories were not welcomed by the medical profession. This factor, combined with his more liberal political views, resulted in his leaving the hospital in 1849.27 These early epidemiologic theories would have to wait for scientific knowledge to catch up.
35 years prior to the isolation of Salmonella typhi.33 Ignatz Semmelweiss (1818-1865) demonstrated with a retrospective record review that an epidemic of puerperal fever, or childbed fever, in 1847 at the Vienna Lying-In hospital was due to transmission of infection on the hands of medical students and physicians who went from the autopsy room to the delivery room without washing their hands. In contrast, the women who were delivered by midwives, who used aseptic techniques (by immersing their hands in antiseptic solution prior to contact with the patient), had much lower rates of puerperal sepsis (Figure 1-2).34 Unfortunately, while Semmelweiss was correct, bacteria had not yet been identified and his theories were not welcomed by the medical profession. This factor, combined with his more liberal political views, resulted in his leaving the hospital in 1849.27 These early epidemiologic theories would have to wait for scientific knowledge to catch up.
THE DEVELOPMENT OF STATISTICS AND SURVEILLANCE
Meanwhile, the fields of probability and political arithmetic—a term coined by William Petty (1623-1687) to describe vital statistics on morbidity and mortality27—were advancing. Gerolamo Cardana (1501-1576) introduced the concept of probability and described that the probability of any roll of the dice was equal so long as the die was fair.35 Jacques Bernoulli (1654-1705) carried this concept further with the central limit theorem, which states that the observed probability approaches the theoretical probability as the number of observations increases.35
One of the early leaders in the use of statistics to help understand the natural occurrence and epidemiology of infectious diseases was John Graunt (1620-1674), a wealthy haberdasher; he became interested in bills of mortality and published the Natural and Political Observations—The Bills of Mortality in 1662.27, 36 In this document, he detailed the number and causes of deaths in London during the preceding third of a century. Graunt used inductive reasoning to interpret the mortality trends and noted the ratio of male to female births and deaths, mortality by season, and mortality in persons living in rural versus urban locations. He examined several causes of deaths over time and constructed the first life tables.36 Subsequently, other observers used public health data for the study of epidemics of infectious diseases. For example, Daniel Bernoulli (1700-1782), the son of Jacques Bernoulli, analyzed smallpox mortality to estimate the risk-benefit ratio of variolation.12 His calculations determined that the fatality rate of variolation exceeded the benefit in population survival.37
In England, numerous improvements in public health sanitation and vital registries were made in the 1800s. Edwin Chadwick (1800-1890), an arrogant zealot, managed to institute numerous sanitary reforms when he was not annoying his peers.27 Chadwick used health statistics to effectively change public policy. His 1842 report “to the Poor Law
Commission” outlined the cost-effectiveness of public health. His report emphasized the understanding that hygiene was closely related to health, but Chadwick also linked morality to hygiene and health. He made the following pronouncements:
Commission” outlined the cost-effectiveness of public health. His report emphasized the understanding that hygiene was closely related to health, but Chadwick also linked morality to hygiene and health. He made the following pronouncements:
That the formation of all habits of cleanliness is obstructed by defective supplies of water.
That the younger population, bred up under noxious physical agencies, is inferior in physical organization and general health to a population preserved from the presence of such agencies.
That the population so exposed is less susceptible of moral influences, and the effects of education are more transient than with a healthy population.
That these adverse circumstances tend to produce an adult population short-lived, improvident, reckless, and intemperate, and with habitual avidity for sensual gratifications.
That defective town cleansing fosters habits of the most abject degradation and tends to the demoralization of large numbers of human beings, who subsist by means of what they find amidst the noxious filth accumulated in neglected streets and bye-places.
That the expense of public drainage, of supplies of water laid on in houses, and of means of improved cleansing would be a pecuniary gain, by diminishing the existing charges attendant on sickness and premature mortality.38
Chadwick’s countryman William Farr (1807-1883) made important contributions to the improvement and analytical use of public health statistical data. His careful documentation of deaths was used by John Snow to investigate the 1849-1953 London cholera epidemics. Farr initially disagreed with Snow’s hypothesis that cholera was transmitted by water, instead preferring the miasma theory. However, he was eventually convinced, and his book based on the 1866 epidemic demonstrated that contaminated water was a risk for cholera.39
THE DISCOVERY OF MICROORGANISMS
A significant leap forward in scientific understanding came with the visualization of microorganisms. Anton van Leeuwenhoek (1632-1723) invented the microscope, and in 1683 he described how materials such as rainwater and human excretions contained cocci, bacilli, and spirochetes.8 He did not evaluate these organisms as agents of disease, however, and considerable controversy arose over the origin of these minute forms. Because they were often present in decaying or fermenting materials, some people maintained that they were spontaneously generated from inanimate material. However, Leeuwenhoek believed that they were derived from animate life.27
Louis Pasteur (1822-1895) demonstrated the dependence of fermentation on microorganisms in 1857 and showed that these organisms came from similar organisms present in the air.40 Subsequently, Robert Koch (1843-1910) demonstrated in 1876 that he could reproducibly transmit anthrax to mice by inoculating them with blood from sick cattle and that he could then recover the same rodlike bacteria from the sick mice as came from the cattle. Further, he could pass the disease from one mouse to another by inoculating the animals with these microorganisms.12 Based on these experiments he proposed the “Henle-Koch postulates” as proof that a microorganism was the cause of an infectious disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree