Nose and Throat Syndromes
Definitions and Classifications
“Upper respiratory infection,” often abbreviated URI, is a collective term. It has the same kind of meaning as “lower respiratory infection,” i.e., it includes several anatomic syndromes. URI has become a lay term like “strep throat” or “flu.”
The term “URI” is an oversimplification. The clinical skill of a physician is related to the ability to make specific diagnoses, which are based on discrimination and distinction between shades of differences, not on oversimplifications. In general, the best diagnosticians have a large number of possible anatomic syndromes to consider. The use of the collective term URI when a more specific diagnosis is possible implies unnecessarily superficial thinking.
In a study of emergency room visits, the diagnostic terms “common cold” and “rhinitis” were rarely used by the physicians, whereas the term URI was common.1 Perhaps this was because the patient really had a more severe syndrome, sometimes referred to as the “uncommon cold,” which may include acute bronchitis or some other diagnosis the vague term URI covers.1
Two syndromes are often misdiagnosed as upper respiratory infections. The first is a systemic syndrome, manifested by relatively high fever and general symptoms such as headache and fever, but with a normal physical examination. It is useful to classify such illnesses in diagnostic terms that emphasize the fever, such as “fever without localizing signs,” as described in Chapter 10. This term is much more descriptive than “viral syndrome,” an unsophisticated phrase that usually implies fever but is vague, assumes the etiology, and lacks an anatomic component.
The second misdiagnosed syndrome is distinguished by prominent respiratory symptoms (i.e., cough and sore throat) with a moderate to high fever or with generalized weakness. It is useful to classify such illnesses as influenza-like, as described in Chapter 7. Unfortunately, these distinctions between upper respiratory illnesses, systemic febrile illnesses, and influenza-like illnesses are not widely accepted, and medical communications continue to be hampered by the lumping of a variety of separable syndromes into the category of URI or “viral syndrome.”
This chapter includes the common cold syndrome, purulent rhintis, and pharyngitis (see Box 2-1). Other respiratory syndromes are discussed in Chapters 7 and 8. Dental infections, gingivitis, stomatitis, and tongue infections are discussed in Chapter 4.
Common Cold Syndrome
The common cold syndrome was defined in adults as a self-limited illness, with watery nasal discharge, nasal stuffiness, occasionally a scratchy throat, sneezing, chills, burning eyes and nasal membranes,
and mild muscle aches. Cough may be present but is usually not prominent. Significant fever, defined as an oral temperature of 102°F (38.9°C) or higher, is unusual, especially in the older child. Common cold syndrome may reasonably be considered a rhinosinusitis. The lining of the sinuses is contiguous with the nasal mucosa and typically becomes inflamed during the course of a common cold.2
and mild muscle aches. Cough may be present but is usually not prominent. Significant fever, defined as an oral temperature of 102°F (38.9°C) or higher, is unusual, especially in the older child. Common cold syndrome may reasonably be considered a rhinosinusitis. The lining of the sinuses is contiguous with the nasal mucosa and typically becomes inflamed during the course of a common cold.2
Box 2-1 Classification of upper respiratory infections
Anatomic upper respiratory infections
|
Misdlagnosed as upper respiratory infections
|
Possible Etiologies
Rhinoviruses
The most frequent cause of the common cold syndrome in adults and probably in teenagers is infection with one of the approximately 100 serotypes of rhinovirus. Reinfection with the same serotype can occur but is usually less symptomatic.3 Unlike most other human viruses, rhinoviruses are temperature sensitive. They grow best at 33°C, about the temperature of the nasal mucosa, and growth is inhibited gradually at increasing temperatures. In vitro, most rhinoviruses do not grow well at 37°C, which is the reason they do not usually cause lower respiratory infection. It has been reported, however, that certain rhinoviruses can and do cause lower respiratory infection in some individuals,4 and also that infection of the upper respiratory tract with a rhinovirus commonly induces wheezing in patients with asthma.5
Inoculation of susceptible volunteers with a rhinovirus results in an illness that begins about the first day after inoculation and lasts about 7 days. The virus continues to be recoverable from the nasopharynx for about 1–2 weeks. More than 90% of adult volunteers had nasal discharge, nasal obstruction, and inflamed nasal mucosa, and about 50% had sneezing and cough. About 10–30% of adults with the common cold syndrome will have a rhinovirus detected when proper cultures are done.
Coronaviruses
At least two serotypes of these viruses are causes of the common cold syndrome. Experimental infection in adult volunteers produced an illness similar to that caused by rhinoviruses. The incubation period is about 24 hours longer, and the duration of illness is generally 2–3 days shorter. Headache was reported by 85% of volunteers infected with coronavirus 229E versus about half of those infected with rhinovirus.6 These viruses are difficult to detect in the laboratory.7 They have been estimated to cause about 10% of adult upper respiratory infections. They are named for their appearance in electron micrographs as spheres with crownlike, petal-shaped projections. Coronavirus colds are most frequent in young children and gradually decrease in frequency throughout life.8 Reinfection can occur. Wheezing is frequently present.7
Other Viruses
Summer “colds” are often mild infections with enteroviruses, which do not particularly cause diarrhea but do cause fevers, often with mild rhinitis or cough.
Mycoplasmas
Mycoplasma pneumoniae infection, as detected by monitoring of infants and young children, typically is asymptomatic.9 When symptomatic, there can be mild rhinitis and cough, reasonably classified as a “common cold syndrome.” More severe illness associated with M. pneumoniae infection is discussed in Chapter 7.
Modified Viral Infection (Reinfection)
In adults, many illnesses diagnosed as the common cold are probably modified infection caused by viruses that produce a mild illness on reinfection and a more severe disease on primary infection. The most common of these is respiratory syncytial virus, which circulates in epidemics yearly, and to which human adult volunteers can be productively infected repeatedly.10,11 Influenza and the parainfluenza viruses can also cause this phenomenon. Adenoviruses and enteroviruses (Coxsackie and echoviruses) are also occasionally recovered from adults with illnesses resembling the common cold.
Prodrome of a More Serious Infection
Some serious infections, such as bronchiolitis, pneumonia, or meningitis may begin with symptoms resembling those of the common cold. In the case of bronchiolitis, the cold symptoms are part of the natural course of the disease. As for meningitis, the common cold syndrome may, in fact, be a risk factor for its development, due to disruption of the nasal mucosal barrier.12
Allergic Rhinitis
This condition closely resembles the common cold syndrome of infectious etiology. It can occur as
early as the first month of life, especially if the baby is allergic to cow’s milk,13 but is rare in infancy. Mouth breathing, nasal rubbing, recurrent episodes of nasal bleeding, family or personal history of asthma or atopic dermatitis, seasonal episodes, and nasal eosinophilia support the diagnosis of allergic rhinitis.14,15
early as the first month of life, especially if the baby is allergic to cow’s milk,13 but is rare in infancy. Mouth breathing, nasal rubbing, recurrent episodes of nasal bleeding, family or personal history of asthma or atopic dermatitis, seasonal episodes, and nasal eosinophilia support the diagnosis of allergic rhinitis.14,15
Nonallergic Rhinitis with Eosinophilia Syndrome (NARES)
Children 6–12 years of age may also have this syndrome, although it is usually associated with adults.16 The syndrome is characterized by perennial rhinitis, negative allergy skin tests, normal serum immunoglobulin E (IgE), and nasal eosinophilia. It is a vasomotor rhinitis, with pale, boggy, edematous nasal mucosa, and usually responds to topical corticosteroids.
Nasal Polyps
Multiple and bilateral nasal polyps can be the presenting manifestation of cystic fibrosis, whether or not the obstruction or rhinorrhea respond to antiallergic therapy.17
Diagnostic Plan
Usually, no diagnostic studies are necessary or useful for the evaluation of a patient with the common cold syndrome.
Treatment
Antibiotics
Studies in college students, military recruits, and children have repeatedly documented the lack of efficacy of antibiotics in the treatment of the common cold.18,19,20 A Cochrane database review of prospective placebo-controlled trials concluded that antibiotic treatment of the common cold produces no clinical benefit.21 This is an expected outcome because bacteria do not cause the disease. Common cold is only occasionally complicated by secondary bacterial infection, and prophylaxis against this unusual occurrence is not effective.22 Worse, the overuse of antibiotics in clinical pediatrics is a major contributing factor for the emergence of antimicrobial resistance in bacteria. Multiple studies have identified recent antibiotic use as a risk factor for invasive disease with resistant pneumococci.23 Parental desire for antibiotics is not an indication for their use in this benign, self-limited illness. Unfortunately, surveys show that although almost all physicians understand this concept, about half of them routinely prescribe antibiotics anyway.24
Cough Medications
Cough is not in itself an indication for cough suppression. Antitussive medicines are usually not necessary in the common cold but may be helpful for selective cases if the cough is not useful to raise sputum, interferes significantly with sleep, or precipitates vomiting. Severe or protracted coughing should make the physician rethink the diagnosis of common cold syndrome. Asthma is particularly underdiagnosed in this setting, as common cold can trigger an exacerbation of reactive airways disease (see Chapter 7). When needed, dextromethorphan is almost as potent an antitussive as codeine, but it is not addictive. Studies proving the antitussive effect of dextromethorphan in children are lacking. Parents should be educated about the fact that most of the combination cough medications that are available over-the-counter contain other drugs not necessary for treatment of the cough, which can produce significant side effects. Nonsensical combinations are also marketed, such as guaifenesin (thins mucus to make it easier to expectorate) and dextromethorphan (stops the cough that would expel the thinned mucus). Generally, stopping a cough requires a larger dose of dextromethorphan (0.5–1.0 mg/kg) than is recommended on the bottle. Attempting to achieve this dosage in combination syrups is likely to lead to overdosage of one of the other ingredients. Physicians should recommend the simplest formulations available if they choose to medicate cough at all.
Decongestants
Nose drops, nasal sprays, and oral decongestants may provide temporary relief of nasal obstruction. However, excessive use of nose drops can produce sensitization or rebound vasodilation (rhinitis medicamentosa). Several prospective, placebo-controlled studies of antihistamine-decongestant combinations in children have shown no measurable efficacy.25,26 The younger the child, the less likely these medicines are to be effective. No study has ever shown clinical improvement in a child less than age 3 years with the use of these medications. Despite this, physicians continue to recommend over-the-counter antihistaminedecongestant medications,
which have the potential to produce frightening and even life-threatening side effects.27
which have the potential to produce frightening and even life-threatening side effects.27
Expectorants
Drugs such as guaifenesin are intended to reduce the viscosity of sputum. They are unnecessary in the treatment of the uncomplicated common cold. Even in acute bronchitis their value is not clearly established. They may be of some benefit in the treatment of chronic bronchitis in adults. Toxic effects of iodides include acne and goiter. Iodides are contraindicated during pregnancy and breastfeeding, because they can produce goiter in the infant.
Antihistamines
The symptoms of the common cold are caused by virus replication and by the host immune response to the virus, not by histamine release. However, some patients can get partial relief from nasal congestion by the drying effects of antihistamines, a nonspecific side effect of these medications. A metaanalysis of all the prospective, placebo-controlled trials of antihistamines in common cold syndrome concluded “the primary literature offers little support for the use of antihistamines in the common cold.”28 Antihistamines may also produce sedation, decreased bladder tone, and rare severe reactions. If the cough is productive of sputum, the drying effect of antihistamines is undesirable.
Vitamin C
At present, the efficacy of vitamin C is not proved. It has been most highly touted as a preventive, rather than a treatment. A review in the British Journal of Nutrition of the six largest vitamin C supplementation studies (studies that used dosages of 1 g/day or greater) showed no reduction in the incidence of common cold in recipients of vitamin C.29 This analysis included over 5,000 episodes. The relative risk of contracting a cold while on high-dose vitamin C was seen to be 0.99 (95% confidence interval 0.93–1.04). Adverse effects of high-dose vitamin C, other than stomach upset, are uncommon. The urine is acidified, however, which can lead to increased excretion of oxalic acid (a metabolic byproduct of ascorbic acid); this, in turn, can cause urinary tract calculi in predisposed individuals. Other than cost, perhaps the most important disadvantage is that this therapy may encourage people to use excessive doses of other, nonwater-soluble vitamins, some of which are exceedingly toxic.
Zinc Gluconate
A prospective study in adults with community-acquired common cold syndrome showed that subjects who received zinc gluconate lozenges every 2 hours for the duration of their colds recovered 3 days sooner, had half as many days with cough, one third fewer days of hoarseness and headache, two days less nasal drainage, and one third the duration of sore throat as compared with subjects in the placebo group.30 There was no difference in resolution of fever, muscle aches, scratchy throat, or sneezing. Side effect profiles were impressive, with 20% of subjects experiencing nausea and 80% complaining of bad-taste reactions. The mechanism of action of zinc is unknown. An attempt to translate the adult experience into a pediatric population was unsuccessful.31 No benefits of zinc gluconate have yet been demonstrated in childhood. The side effects, however, were preserved.
Other Therapies
Various other therapies have been tried, including anticholinergic nasal sprays, mast cell stabilizers, steroids, and new anti-viral agents active against enteroviruses including the rhinoviruses. Table 2-1 is a summary of these trials, along with the zinc trial mentioned above. The most effective therapy with the lowest side effect profile is probably nasal irrigation with warm salt water, but this has not been well studied. Commercial saline nasal sprays may not be entirely innocuous; most contain benzalkonium chloride, which is toxic to white blood cells in vitro.
Prevention
Vaccines
The need for rhinovirus vaccines, if indeed one exists, is based primarily on the frequency, rather than the severity, of rhinovirus infections. The large number of serotypes of rhinovirus, coupled with the fact that not all colds are due to rhinovirus infection, make a “common cold vaccine” impractical.
Avoid Exposure
Avoidance of exposure is not a practical measure within a family, although handwashing and not
sharing glassware, silverware, etc. may be helpful. Attack rates for rhinovirus infection within a family are high but irregular.
sharing glassware, silverware, etc. may be helpful. Attack rates for rhinovirus infection within a family are high but irregular.
TABLE 2-1. TRIALS OF TREATMENTS FOR THE COMMON COLD SYNDROME | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Rhinoviruses can be transmitted by self-inoculation of the nose or conjunctivae with the fingers.32 As nonenveloped, hard protein-shelled viruses, they can survive on environmental surfaces and fomites for prolonged periods. These viruses can be spread by large aerosol particles33 but not usually by droplet nuclei, which implies that the virus is not likely to be spread beyond 6 feet by air. An instructional program on handwashing and germs decreased the incidence of respiratory infections in a day-care setting.34
Purulent Rhinitis and Nasal Abscess
Purulent rhinitis is an objective diagnosis that implies the presence of thick nasal discharge, usually yellow to green in color. This diagnosis does not imply the presence of bacterial infection. Even if exudate has been cleaned off, the nostrils usually appear crusted. Fever may be present but is usually not greater than 102°F (38.9°C). Excoriation around the nostril may be present.
This diagnostic classification should be used as a preliminary descriptive diagnosis only when there are no findings to suggest sinusitis or otitis. Most children for whom purulent rhinitis is the only finding are younger than 5 years. Purulent or febrile rhinitis usually has been specifically excluded from studies of antibiotic value in uncomplicated upper respiratory infections.
It is not unusual for nasal discharge to change from watery early in the course of a common cold to more viscous and yellow to green 4–7 days after the onset. This is part of the natural history of the common cold syndrome. The mucus changes color because of the influx of lymphocytes, which are there to lyse infected cells and clear the infection. Thus, the appearance of thickened and possibly colored nasal discharge is a good sign, usually heralding recovery from the cold within 3–4 days. The
child usually feels quite well by this time. Parents and physicians alike seem to believe that green mucus is tantamount to a bacterial infection that must be treated with antibiotics, but no study has ever shown a correlation between the color of nasal secretions and the presence of bacteria. Despite this fact, in one study 97% of physicians admitted to routinely prescribing antibiotics for “purulent rhinitis” of any duration.24
child usually feels quite well by this time. Parents and physicians alike seem to believe that green mucus is tantamount to a bacterial infection that must be treated with antibiotics, but no study has ever shown a correlation between the color of nasal secretions and the presence of bacteria. Despite this fact, in one study 97% of physicians admitted to routinely prescribing antibiotics for “purulent rhinitis” of any duration.24
Sometimes, however, persistent purulent rhinitis is caused by bacterial infection of the sinuses. Often, it is the nasal mucosa or adenoidal lymphoid tissue that is the source of the pus. Bacterial sinusitis can be a reasonable diagnosis in cases when the nasal discharge persists for 10–14 days without improvement (See section on sinusitis, Chapter 5.)
Possible Etiologies
Group A Beta-hemolytic Streptococcus
This organism typically produces a thin, slightly bloody discharge. If there is a slow-healing excoriation about the nostril, Group A beta-hemolytic streptococcus is a likely etiology.35
Streptococcus pneumoniae
With this organism, also called the pneumococcus, the discharge is usually green and thick. If the discharge is protracted, or signs of sinusitis are present (fever, facial pain, periorbital swelling), the patient may respond to a course of therapy with amoxicillin.
Sinusitis
This diagnosis should be considered in any patient with purulent nasal discharge and is discussed in detail in Chapter 5.
Uncommon Causes
A foreign body should be considered in young children, especially if the discharge is unilateral and/or foul smelling. Nasal diphtheria is a rare cause of purulent rhinitis. A membrane is sometimes seen, and slight bleeding is often present. Allergic rhinitis is unlikely to produce a purulent discharge. Viral infections, such as those with adenoviruses, might produce purulent discharge, but this has not been documented. Purulent rhinitis without sinusitis caused by other bacteria, such as H. influenzae or Staphylococcus aureus, is difficult to document, because recovery of such normal flora on culture may be coincidental.
Diagnostic Plan
The nose should be examined carefully to exclude the presence of a foreign body. Occasionally, culture of the discharge to exclude Group A streptococcal infection may be indicated. Radiologic studies such as sinus x-rays or computed tomographic scans are usually not helpful.
Treatment
Many physicians use antibiotics to treat purulent rhinitis. Only a small prospective study of purulent rhinitis has been done, which indicated no benefit of cephalexin over placebo, with about 35 children in each group.36 In a carefully controlled study of minor respiratory infections of children, true purulent rhinitis was observed as a complication in only 5 of about 670 patients.37 Thickening and discoloration of mucus near the end of a common cold occurs with much greater regularity. In general, observation without treatment is indicated for patients with green nasal discharge unless the presence of Group A streptococci (which can be confirmed by culture) or a concomitant diagnosis of sinusitis is strongly suspected.
Complications
Acute purulent otitis media or sinusitis may occur as a complication of purulent rhinitis. The frequency of these complications is unknown, because no prospective study of purulent rhinitis has been done.
Nasal Septal Abscess or Hematoma
A history of a nasal furuncle or minor trauma is sometimes present in these cases.38 Dental infections can be a source.39 The swelling is usually bilateral and appears to arise medially. Fever and nasal obstruction are present, but the nasal discharge is usually serous rather than purulent.
Needle aspiration for confirmation and culture and surgical drainage are indicated.40
A nasal septal hematoma can be associated with bacteria without an abscess.41 Hematomas can become infected and produce purulent drainage. The hematoma should be evacuated as an urgent procedure to prevent erosion of the nasal septal cartilage.
Pharyngitis
The terms “tonsillitis,” “tonsillopharyngitis,” and “pharyngitis” are often used interchangeably. In this section, the more general term “pharyngitis” is used for brevity, as the tonsils may have been removed. Pharyngitis is best defined by objective evidence of inflammation of the pharynx, such as exudate, ulceration, or definite erythema. Redness of the throat may occur as part of the general redness of all mucous membranes in a patient with fever. Therefore, a diagnosis of pharyngitis is not justified when the pharynx is no redder than the rest of the oral mucosa or if there is only slight injection of the pharynx.
The symptom of sore throat should be distinguished from the clinical diagnosis of pharyngitis, which should be based on the evidence of definite signs on physical examination. “Sore throat” often refers to tracheal irritation, as can often be demonstrated by asking the patient to point to the location of the soreness. In tracheitis, the patient usually points to the trachea in the midline with one finger. In pharyngitis, the patient typically points with one hand, using the thumb and forefinger to point to the tonsillar nodes.
Diagnostic Approach
It is important to get a thorough look at the pharynx with a good light using whatever restraint is necessary. The pharyngeal examination can be one of the more unpleasant parts of the physical examination, and there seems to be a tendency to rationalize a cursory look. Exudate, which usually resembles a thin layer of milk or cream on the surface, should be distinguished from cryptic debris, which is shiny, yellow-tinted, hard, and smooth and forms a cast of the tonsillar crypts. A cast of debris can be carefully picked out of the crypts, but this is not advisable. Submucosal spherical white areas may be seen, which give the tonsils the appearance of raw ground beef—red with white spheres mixed throughout. These white submucosal areas are not exudate but probably are nodules of lymphoid hyperplasia.
The palate, buccal mucosa, gums, and tongue should be examined for erythema or ulcers. The size and tenderness of the anterior (tonsillar) and posterior cervical nodes should be noted. Careful examination should be done for generalized lymphadenopathy, splenomegaly, liver tenderness, and edema of the eyelids or upper malar area, all of which suggest infectious mononucleosis. Absence of a heart murmur or dependent edema should be noted for their relevance to rheumatic fever and glomerulonephritis. Vital signs, including blood pressure, should be recorded. Poor quality of the heart sounds raises the question of diphtheritic myocarditis.
Anatomic Classification
Exudative Pharyngitis
The definition of exudative pharyngitis is the presence of a white or gray scum on the surface of the tonsils or pharynx. This scum resembles milk and is readily wiped off without producing bleeding. White material seen in the tonsillar crypts is usually cryptic debris, not exudate.
Ulcerative Pharyngitis
The criterion for ulcerative pharyngitis is the presence of circular or oval shallow ulcers on the soft palate, tonsillar area, or posterior pharynx. Herpangina is an older term still used for this syndrome, discussed later.
Membranous Pharyngitis
This is defined by the presence of a membrane (also called a pseudomembrane) on the tonsils, palate, or other part of the pharynx. It is defined as a gray-white layer of materials that can be peeled from the pharynx, usually leaving the surface underneath bleeding. Membranous pharyngitis is rare. In the United States, the cause is rarely diphtheria, which typically occurs in unimmunized children. Instead, most cases are due to infectious mononucleosis, particularly in teenagers and young adults.
Uvulitis
Uvulitis is uncommon. It can be associated with serious disease or can be an isolated finding. Several patterns have been recognized.42,43,44 Uvulitis can occur in conjunction with streptococcal or other severe pharyngitis. In this case, the uvula is very red and swollen, as are the tonsils and the rest of the pharynx.
Uvulitis can also represent an extension of the acute inflammatory process of epiglottitis, so laryngeal or obstructive signs should be noted. A lateral soft-tissue roentgenogram of the neck might be indicated, as described in the section on epiglottitis. Isolated uvulitis has also been reported to occur with bacteremia due to Haemophilus influenzae type
b (Hib) without epiglottitis. Since the advent of the conjugated Hib vaccine, epiglottitis and bacteremia due to this agent have become vanishingly rare in the United States. Prior to the routine use of this vaccine, Hib bacteremia occurred primarily in younger patients and produced high fever and toxicity. Uvulitis due to Group A streptococcal infection, in contrast, is more common in school-age children, and does not cause respiratory distress or high fever.
b (Hib) without epiglottitis. Since the advent of the conjugated Hib vaccine, epiglottitis and bacteremia due to this agent have become vanishingly rare in the United States. Prior to the routine use of this vaccine, Hib bacteremia occurred primarily in younger patients and produced high fever and toxicity. Uvulitis due to Group A streptococcal infection, in contrast, is more common in school-age children, and does not cause respiratory distress or high fever.
Other causes of uvulitis include acute uvular edema.44 This can be an allergic reaction, so that the uvula is more swollen than red. Antihistamines have been recommended to shorten the course of this type of uvulitis.
Throat Culture
The most important and practical decision about pharyngitis is whether it is caused by the Group A streptococcus (S. pyogenes). The throat culture is a useful guide in this decision, but the clinician should make the final judgment as to its significance. Culturing for bacteria other than beta-hemolytic streptococci is unnecessary and usually more expensive.
The value of the throat culture has been clearly established by controlled clinical studies done in physicians’ offices during the 1950s. Valuable studies were done by Breese, Stillerman, and others, who demonstrated that throat cultures are extremely useful for the prevention of rheumatic fever and therefore can be regarded as the gold standard for office practice. Rapid methods for the detection of Group A streptococcal antigen are discussed later.
The standard method for throat cultures, which has been best studied and is in longest use, is swabbing the symptomatic patient’s throat, inoculating a sheep blood-agar plate, and streaking it with a flamed wire loop to separate the colonies.45 Breese, Stillerman, and others have found this method sufficiently sensitive to identify those outpatients who needed antibiotic therapy to prevent complications. The principal variables involved with this method include use of clinical judgment to decide which patients to culture and which plates with few or questionable beta-hemolytic colonies to ignore. The more carefully one attends to the first question, the easier the second question is to answer. Indiscriminate testing of patients who lack objective evidence of pharyngitis leads to a decreased percentage of positive tests, and, more crucially, to an increased number of false-positive test results.46 For this reason, the practice of allowing patients to have a “throat culture only” outpatient visit, during which the patient is not seen by a physician, is discouraged.
The standard throat culture method outlined above has been practical and accurate to the degree that acute rheumatic fever is virtually never observed by those physicians in private practice who use it as a guide to the diagnosis and treatment of streptococcal pharyngitis.
Etiologic Classification
For practical purposes, pharyngitis can be classified as streptococcal or nonstreptococcal on the basis of a conventional throat culture for beta-hemolytic streptococci. “Group A streptococci” and “beta-hemolytic streptococci” are two phrases that, although not synonymous, will be used interchangeably in this chapter, because beta-hemolytic streptococci that cause pharyngitis are almost always Group A.
The throat culture is primarily useful to exclude the diagnosis of streptococcal pharyngitis.47 The recovery of beta-streptococci on throat culture does not prove a streptococcal infection; infection is usually defined by a streptococcal antibody titer rise (which may be partially inhibited by early antibiotic therapy). Although Group A streptococci may not always be the cause of the pharyngitis when found in the throat, their recovery from the throat is infrequent enough using office culture methods that a positive throat culture in a patient with pharyngitis is both a convenient and a practical basis for defining streptococcal pharyngitis. The carrier rate depends on many variables, discussed later in this section.
Frequency of Streptococcal Pharyngitis
Streptococcal pharyngitis is a common disease in children. In one study of school-age children, beta-hemolytic streptococcus was the most frequent cause of moderate to severe pharyngitis and the most common cause of fever greater than 101°F (38.4°C).48 The frequency of beta-hemolytic streptococci as a cause of pharyngitis is closely related to age. In children less than 3 years of age, severe exudative pharyngitis was usually not streptoccocal in one study.49 The exact reason why Group A streptococcal pharyngitis is not common in infants and young children is not well understood. Children less than 3 years of age who have school-age siblings may be at higher risk. Certainly they should
have throat cultures if they have suggestive symptoms and older siblings or adults in the family have compatible illnesses or positive throat cultures. Clinical experience suggests that young children have a somewhat different pattern of illness, with fewer symptoms referable to the throat. It is not uncommon for a young child to not complain of throat pain at all, but rather to have headache, abdominal pain, fever, nausea and vomiting, or some combination of these symptoms. Streptococcal pharyngitis is certainly not unheard of in young children. One study of children with pharyngitis indicated that 17% of those less than 1 year, 19% of those 1–2 years, and 35% of those 2–3 years of age had Group A streptococci recovered.50 Young adults without exposure to children, and older adults also do not frequently contract Group A streptococcal pharyngitis. However, a study of adults presenting to an emergency room with pharyngitis indicated that it is worthwhile to culture those patients with fever or exudates.51
have throat cultures if they have suggestive symptoms and older siblings or adults in the family have compatible illnesses or positive throat cultures. Clinical experience suggests that young children have a somewhat different pattern of illness, with fewer symptoms referable to the throat. It is not uncommon for a young child to not complain of throat pain at all, but rather to have headache, abdominal pain, fever, nausea and vomiting, or some combination of these symptoms. Streptococcal pharyngitis is certainly not unheard of in young children. One study of children with pharyngitis indicated that 17% of those less than 1 year, 19% of those 1–2 years, and 35% of those 2–3 years of age had Group A streptococci recovered.50 Young adults without exposure to children, and older adults also do not frequently contract Group A streptococcal pharyngitis. However, a study of adults presenting to an emergency room with pharyngitis indicated that it is worthwhile to culture those patients with fever or exudates.51
Laboratory Methods
Throat Culture
Swabbing the tonsillar area for inoculation of a sheep blood-agar plate is the practical specific method for recognition of streptococcal pharyngitis. Nasal cultures need not be done and are much less sensitive than are throat cultures for the detection of Group A streptococci if the patient has pharyngitis. Viral culture of the throat is not a practical method for early diagnosis of viral pharyngitis. Viral agents causing pharyngitis are more likely to be recovered from a swab of the deep nasopharynx. Occasionally, viral throat cultures will have educational value for late confirmation of a clinical diagnosis.
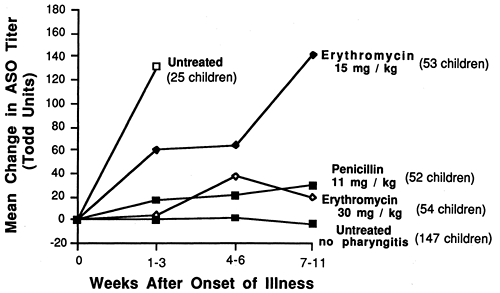
Antistreptolysin O Titer
Serologic methods are also of no practical value in determining whether pharyngitis is streptococcal or not. A rise in antistreptolysin O (ASO) titer takes 3–6 weeks or longer, and waiting that long without antibiotic therapy increases the risk of acute rheumatic fever. Antibiotic therapy tends to prevent a rise in ASO titer, but if a rise occurs in spite of antibiotic therapy, this can be taken as accurate evidence of a streptococcal pharyngitis. Sometimes it is asserted that failure to develop an antibody titer rise is evidence that a patient was a streptococcal carrier and that the pharyngitis had some other cause. However, carriers should not be defined in this way, because the ASO titer is suppressed by antibiotic therapy, and more so by early treatment and larger doses (Fig. 2-1).52,53,54
The ASO titer may be useful to demonstrate that a recent unrecognized and untreated streptococcal
infection has occurred in a patient with suspected acute rheumatic fever, as discussed in Chapter 18. However, it is neither necessary nor advisable to use ASO titers to follow the antibody response of patients with streptococcal pharyngitis who are adequately treated with antibiotics.
infection has occurred in a patient with suspected acute rheumatic fever, as discussed in Chapter 18. However, it is neither necessary nor advisable to use ASO titers to follow the antibody response of patients with streptococcal pharyngitis who are adequately treated with antibiotics.
Antigen Detection Methods
Group A streptococcal antigen tests that detect the presence of streptococci in throat swabs are now widely available and are being used with increasing frequency in the routine evaluation of children with pharyngitis.
The most relevant problem of these rapid antigen tests is whether the sensitivity is sufficient. Studies show that most commercially available antigen detection kits have a sensitivity of about 90% compared with conventional throat culture techniques, especially if cultures with fewer than 10 colonies are considered negative.55 However, many children with fewer than ten colonies of Group A streptococci on throat cultures will have a rise in their titer of antistreptococcal antibodies if untreated. This has led many clinicians to back up rapid antigen detection methods with conventional culture. Children with positive antigen tests are treated, and those with negative tests are not treated unless their throat culture becomes positive. Newer rapid antigen tests that utilize an optical immunoassay (OIA) may actually be more sensitive than traditional culture,56 but are not yet widely available (in this study Todd-Hewitt broth culture was used as the gold standard). In a recent study, polymerase chain reaction was as sensitive as culture and much more so than antigen testing.57 However, this test takes longer than rapid antigen testing and is not yet widely available.
The consequences of having rapidly available results in the office are important. The patient (or patient’s family) is often interested in obtaining a rapid diagnosis so that therapy can begin as soon as possible. There is also a psychological benefit from obtaining a diagnosis on the day of the visit. Enthusiasm for these tests needs to be tempered by remembering that (1) streptococcal pharyngitis is a self-limited disease, in which the symptoms are modulated somewhat but not eliminated by antibiotic therapy, (2) there is no increased risk of nonsuppurative complications by delaying therapy until the throat culture results are available, and (3) early institution of therapy against Group A streptococcus may ameliorate the patient’s antibody response, which may predispose to more frequent reinfection.58
The gold standard against which all these rapid antigen tests are measured is the usual office procedure of using a sheep blood-agar plate streaked on the surface and cultured in ordinary incubator temperature without CO2 or anaerobic conditions. False-negative cultures may be obtained when throats are too gingerly or rapidly swabbed, or when the patient has had a recent dose of an antibiotic.
Nonspecific Laboratory Methods
These studies are of little value in the etiologic diagnosis of pharyngitis. Throat smears are of no value in making an etiologic diagnosis of any type of pharyngitis, and are likely to be misleading in the diagnosis of diphtheria because “diphtheroids” are frequently seen. Owing to an effective vaccine, diphtheria has become so rare that there are few technicians, bacteriologists, or pathologists who see it often enough to maintain competence in reading smears for corynebacteria. The interpretation of smears for diphtheria is frequently false positive.
White blood cell counts are often equivocal and are of no specific value in ruling in or out the diagnosis of streptococcal disease. The presence of lymphocytosis or atypical lymphocytes may aid in the diagnosis of infectious mononucleosis. High white blood cell counts may occur in viral, as well as in Group A streptococcal, pharyngitis.
C-reactive protein or other measures of inflammation are of no value in distinguishing streptococcal from viral pharyngitis.59
Reasons to Do Throat Cultures
Throat cultures for streptococci are recommended, especially for school-age and preschool children, when the following conditions are present:
Pharyngitis without hoarseness or significant cough, especially with fever
Febrile cervical adenitis
Illnesses with definite fever but no apparent focus of infection, especially if headache, abdominal pain, vomiting without diarrhea, or a scarlatiniform rash are present
Symptomatic family contacts of patients with streptococcal pharyngitis.60 Asymptomatic family contacts should not be cultured.
TABLE 2-2. FINAL CLINICAL DIAGNOSES IN 230 CONSECUTIVE ADMISSIONS TO A CHILDREN’S HOME INFIRMARY OF SCHOOL-AGE CHILDREN WITH AN ORAL TEMPERATURE OF 101°F OR HIGHER | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
As shown in Table 2-2, both otitis media and fever without localizing signs are associated with Group A streptococci significantly more frequently than they are seen in a normal control group. The office throat culture is a simple and inexpensive way to detect concurrent streptococcal pharyngitis. In patients with obvious acute otitis media that requires treatment with antibiotics (see Chapter 5), throat culture may be omitted because the antibiotics that treat otitis media also treat streptococcal pharyngitis.
Methods for Throat Culture
Personnel charged with obtaining throat cultures must be trained in the proper technique in order to derive useful information. A single cotton-tipped swab is used to swab the patient’s tonsillar area. Refrigerating the swab overnight or retaining it at room temperature for several hours does not significantly reduce the accuracy of the method.61 “False-negative” results where two consecutive cultures reveal one positive and one negative result are usually found in patients with small numbers of colonies and probably have little if any clinical significance.48,52
Anaerobic incubation or incubation in CO2 may yield a slightly greater frequency of positive cultures for Group A streptococci.62 However, the simpler, practical methods described above have been sufficiently sensitive for prevention of rheumatic fever by detecting streptococcal pharyngitis in office practice.45 Selective media for Group A streptococci are available, but their increased sensitivity has not been proved necessary in office practice.
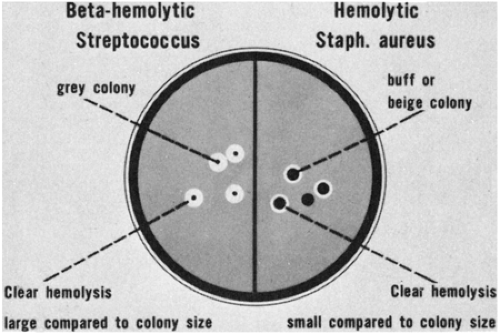 FIGURE 2-2 Comparison of size of hemolysis zone produced by beta-hemolytic streptococci with that produced by hemolytic S. aureus. |
As mentioned above, after inoculation onto a sheep blood-agar plate, the culture should be streaked with a flamed wire loop. Beta-hemolysis can often be recognized after 12–16 hours of incubation at 37°C. The area of hemolysis is large compared with the colony size (Fig. 2-2). The plate should be reexamined for beta-hemolytic colonies after an additional 24 hours at room temperature, since this will detect approximately 10% of the additional positive cultures. Non-Group A beta-hemolytic streptococci are not inhibited by a bacitracin disk placed on the plate at the time of inoculation (Fig. 2-3).
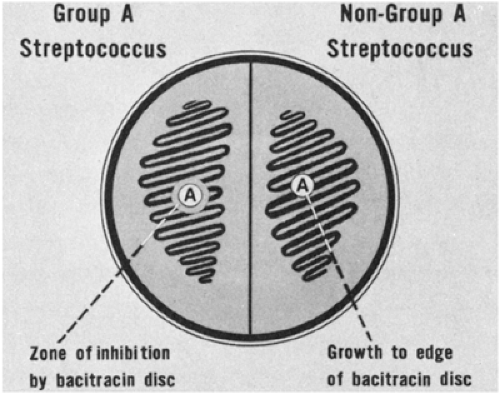 FIGURE 2-3 Group A streptococci are inhibited by bacitracin, but other groups of streptococci are not. |
Although there are more sensitive methods for the recovery of Group A streptococci, the above method is sensitive enough for practice purposes and avoids identifying small numbers of Group A streptococci in well individuals. The simple surface streaking method has a long history of successful discrimination between normal children and those at risk for acute rheumatic fever.45
Non-Group A Streptococcal Pharyngitis
The fact that beta-hemolytic streptococci other than Group A can cause streptococcal pharyngitis has been well established for at least 25 years. The primary basis of this evidence is food-borne outbreaks, where one of the non-Group A streptococci has contaminated food, particularly milk, and resulted in an outbreak of pharyngitis. Such outbreaks have confirmed that Group C or Group G streptococci can cause pharyngitis.63 Of course, outbreaks of Group A streptococcal infection due to contaminated foodstuffs have also been reported, usually when food was contaminated by someone with active Group A streptococcal pharyngitis.64 One outbreak of food-borne Group A streptococcal pharyngitis secondary to foodstuff contaminated by a cook with an infected hand wound has been reported.65
Group B streptococci also have a statistical relation with pharyngitis.66 Because Groups C, G, and B can also be normal pharyngeal flora, it is still not known whether it is important to look for these organisms in nonoutbreak situations, or whether penicillin therapy should be given when they are recovered from the throat. A reasonable solution is that if on throat culture a patient with pharyngitis has streptococci that are not bacitracin sensitive, a recheck of the patient’s symptoms should be done; if the patient is still sick, one could consider using penicillin, which may afford some symptomatic relief. However, it should be emphasized that there is no risk of acute rheumatic fever after non-Group A streptococcal pharyngitis.
Interpretation of Throat Culture
Carrier Rates
Interpretation of positive throat cultures is occasionally complicated by the fact that the isolation of Group A streptococci from the throat does not necessarily imply infection. The frequency of Group A streptococcal carriage in normal children has varied from study to study and is a function of the sensitivity of the culture method and the relative certainty of the patient’s being “normal.”45 In a private practice, where the certainty that an individual was “normal” was great, Group A streptococci were recovered from 3–5% of children.45,67 In a study in a children’s home in which children were under close supervision, about 8% of normal children with nonpharyngeal disease had positive cultures with more than 10 colonies of Group A streptococci (see Table 2-2).48 In surveys of schoolchildren, in which many have had a recent unreported illness, the recovery rate of Group A streptococci has usually been about 10–40% but has been as high as an average of 30% of “normal” (nonsick) individuals.45
The high carrier rates found in surveys of schoolchildren is best explained by use of excessively sensitive methods for recovery of Group A streptococci, use of multiple cultures, failure to assess the normality of the children by history and physical examination, and detection of a high convalescent carrier rate in a lower socioeconomic group that often did not seek medical care for illness.45 The lower carrier rates of about 5–10% or less by Breese, Moffet, McCracken, and others reflect use of a single culture and careful screening to exclude convalescent individuals.45,48,68
Numbers of Colonies
In general, there is a correlation between the number of colonies of Group A streptococci found on throat culture and the clinical and laboratory findings of the patient. That is, the fewer the colonies on the culture plate, the less likely the patient is to have had recent or severe clinical pharyngitis, a typable Group A streptococcus, or an ASO titer rise. However, some patients with a severe pharyngitis do have fewer than 10 colonies; in one series, 33% of patients with fewer than 10 colonies had an ASO titer rise.69 Another study revealed that 82 (29%) of 279 children with fewer than 10 colonies of beta-hemolytic streptococci had a typable organism, and one third of these 82 children had an ASO titer rise (Table 2-3). Thus, about 10% of children with fewer than 10 colonies will have both a typable Group A streptococcus and an ASO titer rise. Yet another study gave even a higher estimate: about half of patients with 10 or fewer colonies had a rise in ASO or anti-DNAse B titer.53
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree