(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
Midline Abdominal Wall Gap
If the abdominal wall is fibrotic following radiation treatment and the procedure is prolonged, causing edema of the bowel loops, it is not rare for the surgeon to be unable to bring together the edges of the fascia and skin of a midline abdominal incision. In milder cases, one may be able to force the fascial edges together at the risk of a compartment syndrome.
In this situation, an absorbable mesh may be placed at the level of the fascia, allowing the development of granulation tissue through the pores of the mesh, which later can be covered by a split-thickness skin graft. Dermal grafts have also been used to cover the exposed bowel loops, but the limited availability of larger sizes and inadequate tensile strength restrict their utility. Mobilization of the musculoaponeurotic layers through relaxing incisions, as in the “components separation method” [1] or variations of that method [2–4], requires extensive undermining of skin flaps in these cases and can be accompanied by about a 40 % rate of complications and hernia recurrence in 10–32 % of patients [5, 6]. These methods are applicable mainly in epigastric (midline) hernias, in which there is a fascial defect to approximate but there is still skin coverage.
In our experience [7], the preferable method of dealing with an acute, midline abdominal wall gap may be mobilization of a rectus abdominis flap consisting of the muscle and underlying sheet of transversalis fascia-peritoneum (i.e., rectus abdominis–posterior sheath [RAPS]), separating the flap from the anterior rectus sheath (Figs. 23.1 and 23.2). One of the flaps based on the superior epigastric vessels is divided at the pubic crest (Fig. 23.3), and the other, based on the inferior epigastric vessels, is divided near the costal margin. The combined sheet of transversalis fascia-peritoneum on each side is incised medial to the linea semilunaris through a vertical, longitudinal incision joining the transverse incision at one end, which provides complete mobility of each flap (Figs. 23.4 and 23.5). The two flaps joining together at the midline can cover a large midline gap (Fig. 23.4).
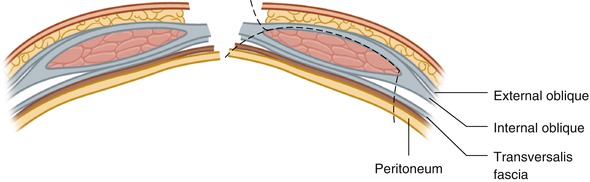
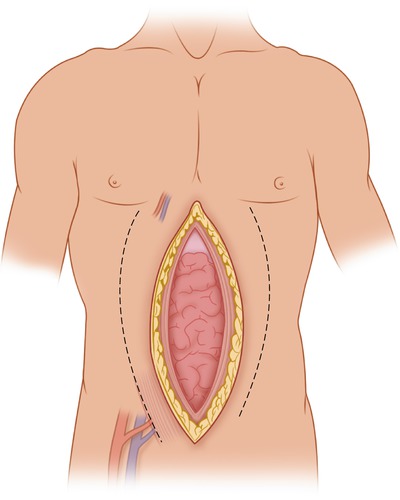
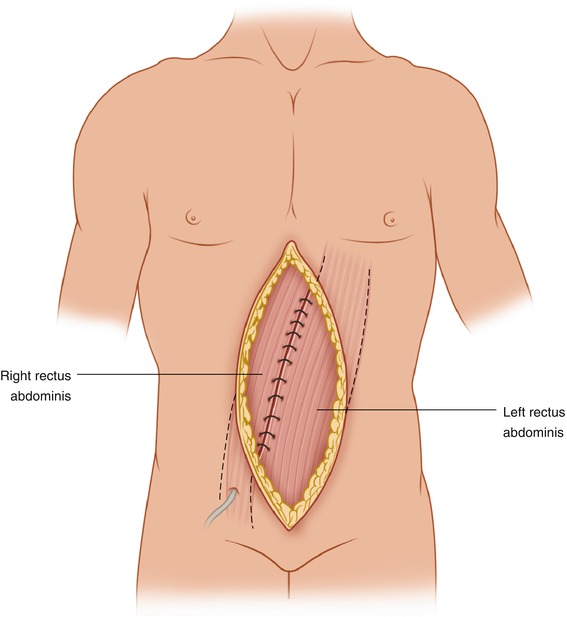
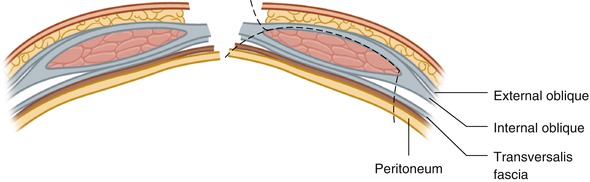
Fig. 23.1
This diagram shows a cross-section of the abdominal wall in a midline gap. The dashed line shows the plane of dissection mobilizing the rectus abdominis–posterior sheath (RAPS) flap. EO external oblique, IO internal oblique, TA transverse abdominis, TF transversalis fascia, P peritoneum
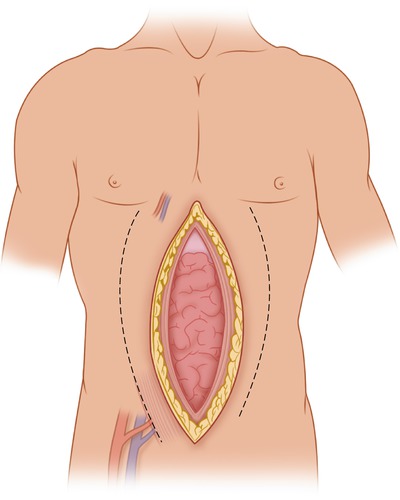
Fig. 23.2
At the end of an operation, a large gap may not be possible to bring together despite maximum relaxation. The inferior and superior epigastric vessels are outlined for the right rectus abdominis muscle
Fig. 23.3
A left RAPS flap has been mobilized to bridge the midline gap, based on the superior epigastric vessels
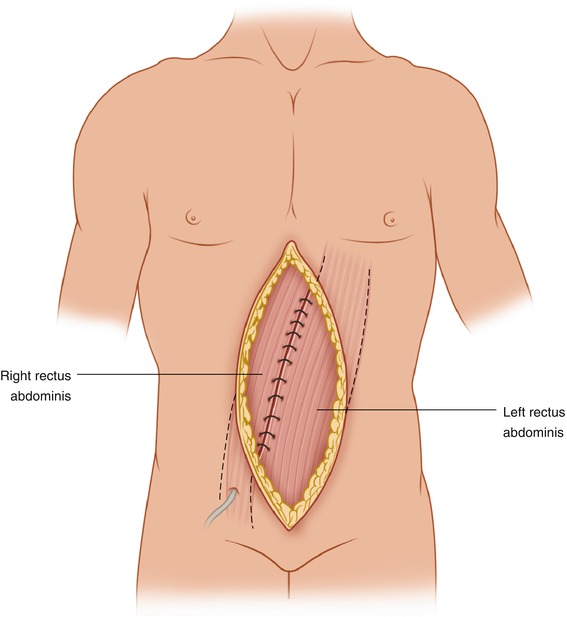
Fig. 23.4




Both right and left RAPS flaps have been mobilized to cover a large gap, which can be skin-grafted immediately
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree