This article presents an overview of medulloblastomas, central nervous system primitive neuroectodermal tumors, and germ cell tumors for the practicing oncologist. Discussion includes the definition of these tumors, histopathologic findings, molecular and genetic characteristics, prognoses, and evolution of treatment.
- •
Brain tumors are the most common solid tumors during childhood. Treatment of central nervous system (CNS) germ cell tumors and embryonal brain tumors is complex; however, survival rates have improved.
- •
Medulloblastoma is the most common malignant brain tumor in children. Neither clinical stratification nor pathologic classification has been fully adequate in predicting outcomes. The presence of certain molecular markers has been shown to impact survival. Molecular stratification will guide future therapeutic approaches.
- •
CNS primitive neuroectodermal tumors (PNETs) have worse outcomes when compared with medulloblastoma. Supratentorial PNETs are characterized by multiple genetic alterations, which are different from pineoblastomas and medulloblastomas.
- •
There is no standard therapy for relapsed CNS PNETs and medulloblastoma.
- •
CNS germ cell tumors are classified into pure germinomas and nongerminomatous germ cell tumors. The treatment approach is dependent on the subtype, but usually combines radiotherapy and chemotherapy.
Introduction
Brain tumors are the most common solid tumors and the second most common malignancy during childhood. The overall annual incidence in the United States is estimated to be 33 per million children younger than 14 years. Major advances in neurosurgery, chemotherapy, and radiation techniques have led to a decline in mortality rate in the last 2 decades.
Treatment of brain tumors including central nervous system (CNS) germ cell tumors and embryonal brain tumors is complex, and although survival rates have improved for some subtypes of these lesions, the treatment-related morbidity remains high. Novel diagnostic and treatment strategies are essential to selectively target these tumors without affecting the normal tissue. The evolution of and current approaches in both diagnosis and treatment of germ cell and medulloblastoma/primitive neuroectodermal tumors (PNETs) in children are reviewed in this article.
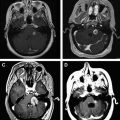
Medulloblastoma
Medulloblastoma is a malignant embryonal (World Health Organization [WHO] grade IV) tumor that affects the cerebellum, comprises approximately 17% of all pediatric brain tumors, and is the most common malignant brain tumor in children. Studies have shown a bimodal peak distribution with maximum incidence between age 3 to 5 and 8 to 9 years. The etiology of some medulloblastomas has been linked to certain genetic disorders, including Gorlin syndrome (patched homolog 1 [PTCH1] mutation) and Turcot syndrome (adenomatous polyposis coli [APC] mutation). Overall survival for children with average-risk disease (to be defined later in this article) now exceeds 80%, but remains lower in infants and for those with high-risk disease. In addition, treatment-related long-term side effects are considerable; examples include neurocognitive impairment; endocrine abnormalities; hearing loss; and secondary malignancy. Evolution of treatment approaches seeks to improve survival rates while decreasing toxicity through developing targeted molecular therapy, as well as improving radiation techniques and reduction of radiotherapy doses.
Histologic Features of Medulloblastoma
Histopathologically, classical medulloblastoma consists of densely packed cells with immunopositivity for neuronal markers such as synaptophysin and neuron-specific enolase. Glial differentiation denoted by immunopositivity to glial fibrillary acidic protein may occur. Other histologic subtypes include: (1) desmoplastic/nodular medulloblastoma characterized by nodular reticulin-free zones surrounded by densely packed cells, this type being more common in infants and adults ; (2) medulloblastoma with extensive nodularity, similar to the desmoplastic variant but with more expanded lobular architecture; (3) anaplastic medulloblastoma characterized by high mitotic activity with marked nuclear pleomorphisim and atypical forms; and (4) large-cell medulloblastoma characterized by a monomorphic large round cell with variable amounts of eosinophilic cytoplasm. Any of these types can present histologically with myogenic differentiation (medullomyoblastoma) or melanotic differentiation (melanocytic medulloblastoma).
Risk Stratification of Medulloblastoma
Current clinical and radiographic disease stratification uses patient age, extent of tumor resection, pathologic subtype, and metastatic (M) status. Previous studies showed that children younger than 3 years had inferior 5-year progression-free survival (PFS) when compared with children 3 years or older (32% vs 58%, respectively). The extent of surgical excision was found in early series to be a statistically significant prognostic factor, as M0 patients in whom less than 1.5 cm 2 residual tumor was evident experienced a better 5-year PFS when compared with those with residual tumor of 1.5 cm 2 or greater (78% vs 54%) ; more recent studies have questioned the significance of the relatively arbitrary 1.5 cm 2 criteria. Infants with desmoplastic medulloblastomas had better outcomes than infants with classic medulloblastomas, with reported 3-year event-free survival (EFS) of 73%, and tumors with diffuse anaplasia have been associated with a poorer prognosis than classic tumors. Patients are considered high risk if they have more than 1.5 cm 2 of residual tumor postresection, have large-cell or anaplastic histology, and/or have evidence of metastatic disease, as shown in Table 1 .
| Average-Risk Disease | High-Risk Disease | |
|---|---|---|
| Extent of resection | Near total and total | Biopsy and subtotal |
| M status | M0 | M1–M4 |
| Histology | Classic/desmoplastic | Anaplastic/large cell |
Neither the clinical stratification nor the pathologic classification has been fully adequate in predicting outcomes. Subsets of children with average-risk medulloblastoma may still do very poorly, with resistance to treatment, early relapse, and dissemination.
Molecular Stratification
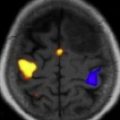
The presence of certain molecular markers has been shown to affect survival. Studies showed that nuclear immunoreactivity for β-catenin, CTNNB1 mutation, overexpression of neurotrophin-3 receptor (TRKC3), and monosomy 6 were associated with improved survival, whereas ERBB2 expression and MYCC or OTX2 amplification were associated with poorer outcomes. However, the clinical utility of some of these markers remains limited given conflicting conclusions in reports. Recently, multiple molecular pathways have been implicated in the pathogenesis of medulloblastoma. For example, in some tumors the sonic hedgehog (Shh) pathway is activated and mediates tumorigenesis via the activation of glioma-associated homolog 1 (Gli1); this activation may be through modification of any component of the Shh pathway, including elements such as patched, suppressor of fused (SUFU), and smoothened (SMO) proteins. Gli1 is a transcription factor that promotes proliferation through activation of various oncogenes including cyclinD1 and cyclinD2. In other medulloblastomas, the wingless type (Wnt) pathway seems to mediate activation of several oncogenes that promote tumorigenesis and inhibit apoptosis such as MYC, cyclinD1, and RE1-silencing transcription factor (REST). Using high-density microarrays, recent analysis led to the discovery of other genes altered in 16% of children with medulloblastoma, including histone-lysine N -methyl transferase genes (MLL2 or MLL3).
Multiple independent groups have further used gene and mRNA profiling to discover the presence of at least 4 molecular subtypes of medulloblastoma. The subtypes include tumors associated with: (1) Wnt pathway activation; (2) Shh pathway activation; (3) c-MYC activation (labeled group C); and (4) high levels of the orthodenticle homeobox 2 ( OTX2) and forkhead box protein G1b (FOXG1B ), but lacking high expression of MYC (group D). These groups seem to predict outcome more accurately than historical staging criteria. In one study, when outcomes for children with metastatic disease were controlled for molecular tumor subtype, overall survival was similar in those with or without metastatic disease. The Wnt pathway subtype is associated with excellent prognosis, and to a lesser extent so are tumors with Shh activation. Group C tumors (c-MYC amplified) have poor outcomes. Group D patients have increased heterogeneity in their outcomes, implying that additional factors are needed to differentiate this group. Reports have demonstrated that immunopositivity for follistatin-like 5 (FSTL5) identified a cohort of patients at high risk for relapse and death. As greater than 50% of non-Wnt/non-Shh tumors displayed FSTL5 negativity, some group D tumors may potentially carry a better prognosis.
Treatment of Medulloblastoma
The treatment of medulloblastoma is complex and usually involves a combination of surgery, radiation therapy, and chemotherapy. The role of surgery was recognized in the early 1900s by Harvey Cushing, and studies subsequently demonstrated that residual tumor bulk is one of the most important predictors for PFS in medulloblastoma. Surgery can be complicated in up to 20% of posterior fossa tumors by cerebellar mutism or posterior fossa syndrome, which typically arises hours to 1 to 2 days after resection. This condition is characterized by speech impairment progressing to significant mutism, hypotonia, ataxia, and emotional lability. It is thought to be due to an injury in the dentate nuclei and their efferent pathways. However, Cushing recognized that tumor resection alone was inadequate, as most of his surgically treated patients suffered relapse. Focal radiotherapy was thus used as adjuvant therapy, and evolved to encompass the posterior fossa. After poor survival rates were noted with focal radiotherapy alone, craniospinal irradiation (CSI) was used with resultant improved survival. Current standard radiotherapy is, therefore, CSI with a focal boost to the posterior fossa and other areas of disease. Standard doses were historically 36 Gy of CSI for both average-risk and high-risk patients, with a focal boost to 54 Gy.
Radiation to the developing brain is fraught with complications, including vasculopathy with the risk of stroke and endocrine complications. Neurocognitive sequelae have been among the most troubling, with full-scale intelligence quotient (IQ) declines of 2 to 9 points per year after irradiation, and greater IQ deficits associated with younger age or higher doses at radiotherapy ; thus, attempts have been made to reduce the dose of radiotherapy. Such attempts were more successful with the addition of chemotherapy, which was able to augment radiotherapy and improve outcomes.
Average-Risk Medulloblastoma
Children with average-risk medulloblastoma have postsurgical residual tumor equal to or less than 1.5 cm 2 on magnetic resonance imaging (MRI), no evidence of disseminated disease in the preoperative or postoperative MRI, postoperative lumbar cerebrospinal fluid that displays no tumor cells (M0), and nonanaplastic/large-cell histopathology. Because of the relatively good survival but substantial adverse events with standard treatment strategies, multiple trials have examined dose reductions of CSI to 23.40 Gy without adjuvant chemotherapy. These studies showed a potentially lesser negative impact on neurocognition with less significant IQ point decreases of 10 to 15 points, but with higher relapse rates (5-year PFS was 67% in the full-dose CSI arm and 52% in the reduced-dose CSI arm). By contrast, when adjuvant chemotherapy (lomustine [CCNU], vincristine, and cisplatin) was added during and after radiotherapy, survival rates compared favorably with those obtained in studies using full-dose radiation therapy alone (5-year PFS 79%). Subsequent studies prospectively compared 2 adjuvant chemotherapy regimens: CCNU, cisplatin, and vincristine or cyclophosphamide, cisplatin, and vincristine; this study showed no difference in the 5-year EFS between the treatment groups (81% and 86%, respectively). A separate, smaller trial using 23.4 Gy CSI followed by 4 cycles of high-dose chemotherapy (vincristine, cyclophosphamide, and cisplatin) with stem cell support showed a 5-year EFS of 83%. The use of intensive preirradiation chemotherapy (ifosfamide, etoposide, intravenous high-dose methotrexate, cisplatin, and cytarabine) resulted in a poorer 3-year EFS and worsened myelotoxicity when compared with immediate radiotherapy (35 Gy) with concomitant vincristine followed by cisplatin, CCNU, and vincristine (65% vs 78%, respectively). Hence, chemotherapy is typically given after radiotherapy.
The feasibility of further dose reduction of radiotherapy to 18 Gy for patients between 3 and 7 years is currently being investigated, as is a reduction in the field of the boost based on number of pilot studies. Further modification of chemotherapy, such as dose reduction of cisplatin to minimize ototoxicity, is also being explored.
High-Risk Medulloblastoma
Despite treatment with higher doses of CSI and chemotherapy, children with high-risk medulloblastoma continue to have poor outcomes (5-year EFS 50%–60%). Thus no dose reduction in CSI has been implemented in these patients. The role of chemotherapy in this disease has been investigated in multiple clinical trials. When adjuvant chemotherapy (consisting of CCNU, vincristine, and prednisone) was used after radiotherapy, the estimated 5-year EFS was 59% compared with 50% for patients treated with radiotherapy alone. However, when only including patients with more extensive disease, the group that received adjuvant chemotherapy showed significantly better EFS when compared with similar patients treated with radiotherapy alone (48% vs 0%). Preirradiation chemotherapy (cisplatin and etoposide) followed by adjuvant chemotherapy (cyclophosphamide and etoposide) showed no impact on 5-year PFS and overall survival (OS) when compared with radiotherapy after surgical resection, followed by chemotherapy (cisplatin, etoposide, cyclophosphamide, and vincristine). Other approaches such as a dose-intensive, alkylator-based regimen of chemotherapy (4 cycles of cyclophosphamide, cisplatin, and vincristine) with stem cell support have been used after maximum resection and radiotherapy, resulting in a similarly improved outcome (5-year EFS 70%) but with substantial reduction in the duration of treatment (4 months vs 12 months). The Children’s Oncology Group (COG) is currently investigating the efficacy of carboplatin administered concomitantly with radiation and isotretinoin as a proapoptotic agent administered with 6 cycles of adjuvant chemotherapy.
Medulloblastoma in Young Children
Patients younger than 3 years generally have a poor prognosis with an estimated 5-year PFS of 30% to 40%, attributable to an increased incidence of neuraxis dissemination, inability or physician/patient reluctance to administer full-dose radiotherapy, and the possible presence of different genetic alterations. One notable exception is the relatively good outcome of patients with medulloblastoma with desmoplastic histology, which can be treated with chemotherapy alone with a 5-year PFS of 65% to 85%. Given the risks of radiotherapy-induced severe neurocognitive sequelae in very young children, the overall strategy has been to use chemotherapy in an attempt to delay or avoid irradiation. One trial that attempted to delay radiotherapy by 1 to 2 years using intensive chemotherapy consisting of vincristine, cyclophosphamide, etoposide, and cisplatin resulted in early failure (most failures occurred during the first 6 months of chemotherapy) and poor 5-year EFS and OS (32% and 40%, respectively). In this study, infants without metastatic disease who also had a gross total resection had slightly better outcome, with 5-year OS of 69%. Other chemotherapy regimens that have been attempted include combinations variably including procarbazine, ifosfamide, intravenous/intrathecal methotrexate, cisplatin, cytarabine, and vincristine. These regimens were associated with relatively poor 5-year OS (35%). A study comparing an induction regimen based on cyclophosphamide and cisplatin with one based on ifosfamide and carboplatin, followed by maintenance chemotherapy, showed no difference between the 2 treatment arms, with 5-year EFS of 32% in both arms. A similarly poor 3-year EFS of 40% resulted after induction chemotherapy based on cisplatin and high-dose methotrexate, followed by consolidation with high-dose chemotherapy and stem cell rescue. Radiation in this study was given at a dose of 23.4 Gy for patients with evidence of residual disease at the end of induction chemotherapy. The COG recently completed a pilot trial in which 3 courses of standard chemotherapy followed by 3 courses of high-dose chemotherapy with stem cell rescue preliminarily showed slightly superior outcomes, with a 3-year EFS of 67% in M0 patients.
There is no consensus regarding the use of radiation therapy in children younger than 3 years, and despite the use of varying intensive chemotherapy regimens, CSI could only be delayed by 1 year in up to 34% of patients because of early recurrence or progressive disease.
Recurrent Medulloblastoma
Recurrent and progressive medulloblastomas have very poor prognoses, with postrecurrence 2-year OS of approximately 25% despite aggressive treatment regimens. Only anecdotal reports have described prolonged survival after relapse. It has been suggested that early identification of recurrence is associated with a longer survival. Current suggested approaches include the use of reirradiation, which has some limited data on its efficacy, especially in patients without gross disease, with 48% 5-year EFS. A metronomic combination of oral etoposide, cyclophosphamide, thalidomide, celecoxib, and fenofibrate, augmented with alternating courses of intrathecal etoposide and liposomal cytarabine in combination with biweekly intravenous bevacizumab, was also explored in a study that included 6 patients with recurrent medulloblastoma, with resulting 2-year OS of 80% and PFS of 53%.
For younger patients with metastatic or recurrent disease, the use of radiotherapy is usually based on physician’s discretion and family wishes, but may have some utility in salvaging patients.
Future Directions
Future approaches for the treatment of medulloblastoma will likely be based on an increased understanding of the molecular features of individual tumors and the development of specific, patient-tailored, molecularly targeted therapies. Using this improved knowledge of underlying molecular characteristics, risk stratification may be more accurately assigned to particular patients, resulting in more appropriate treatment regimen applications and decreased toxicity. Such treatment is already undergoing investigation, using therapeutics targeting the Shh with SMO small-molecule antagonist (GDC-0449). Antiangiogenic therapies such as bevacizumab, inhibitor of poly(ADP-ribose) polymerase (PARP), and anti–insulin-like growth factor I receptor monoclonal antibody (IMC-A12) in combination with an mTOR inhibitor (temsirolimus) are also being examined in different pediatric CNS tumors including medulloblastoma.
Other studies are currently examining the feasibility of adding the histone deacetylase inhibitor, suberoylanilide hydroxamic acid (SAHA), and isotretinoin to standard induction-chemotherapy drugs. This approach is based on preclinical studies suggesting that isotretinoin induces apoptosis through promoting BMP-2 transcription and clinical studies suggesting isotretinoin synergy with cisplatin. SAHA has also been shown to induce apoptosis in medulloblastoma cell lines.
[Tags: Medulloblastoma, Average-risk medulloblastoma, High-risk medulloblastoma, Wnt pathway, Shh pathway, Recurrent medulloblastoma, Medulloblastoma at young age, Molecular stratification of medulloblastoma, Clinical stratification of medulloblastoma, Radiotherapy dose reduction in medulloblastoma].
Medulloblastoma
Medulloblastoma is a malignant embryonal (World Health Organization [WHO] grade IV) tumor that affects the cerebellum, comprises approximately 17% of all pediatric brain tumors, and is the most common malignant brain tumor in children. Studies have shown a bimodal peak distribution with maximum incidence between age 3 to 5 and 8 to 9 years. The etiology of some medulloblastomas has been linked to certain genetic disorders, including Gorlin syndrome (patched homolog 1 [PTCH1] mutation) and Turcot syndrome (adenomatous polyposis coli [APC] mutation). Overall survival for children with average-risk disease (to be defined later in this article) now exceeds 80%, but remains lower in infants and for those with high-risk disease. In addition, treatment-related long-term side effects are considerable; examples include neurocognitive impairment; endocrine abnormalities; hearing loss; and secondary malignancy. Evolution of treatment approaches seeks to improve survival rates while decreasing toxicity through developing targeted molecular therapy, as well as improving radiation techniques and reduction of radiotherapy doses.
Histologic Features of Medulloblastoma
Histopathologically, classical medulloblastoma consists of densely packed cells with immunopositivity for neuronal markers such as synaptophysin and neuron-specific enolase. Glial differentiation denoted by immunopositivity to glial fibrillary acidic protein may occur. Other histologic subtypes include: (1) desmoplastic/nodular medulloblastoma characterized by nodular reticulin-free zones surrounded by densely packed cells, this type being more common in infants and adults ; (2) medulloblastoma with extensive nodularity, similar to the desmoplastic variant but with more expanded lobular architecture; (3) anaplastic medulloblastoma characterized by high mitotic activity with marked nuclear pleomorphisim and atypical forms; and (4) large-cell medulloblastoma characterized by a monomorphic large round cell with variable amounts of eosinophilic cytoplasm. Any of these types can present histologically with myogenic differentiation (medullomyoblastoma) or melanotic differentiation (melanocytic medulloblastoma).
Risk Stratification of Medulloblastoma
Current clinical and radiographic disease stratification uses patient age, extent of tumor resection, pathologic subtype, and metastatic (M) status. Previous studies showed that children younger than 3 years had inferior 5-year progression-free survival (PFS) when compared with children 3 years or older (32% vs 58%, respectively). The extent of surgical excision was found in early series to be a statistically significant prognostic factor, as M0 patients in whom less than 1.5 cm 2 residual tumor was evident experienced a better 5-year PFS when compared with those with residual tumor of 1.5 cm 2 or greater (78% vs 54%) ; more recent studies have questioned the significance of the relatively arbitrary 1.5 cm 2 criteria. Infants with desmoplastic medulloblastomas had better outcomes than infants with classic medulloblastomas, with reported 3-year event-free survival (EFS) of 73%, and tumors with diffuse anaplasia have been associated with a poorer prognosis than classic tumors. Patients are considered high risk if they have more than 1.5 cm 2 of residual tumor postresection, have large-cell or anaplastic histology, and/or have evidence of metastatic disease, as shown in Table 1 .
| Average-Risk Disease | High-Risk Disease | |
|---|---|---|
| Extent of resection | Near total and total | Biopsy and subtotal |
| M status | M0 | M1–M4 |
| Histology | Classic/desmoplastic | Anaplastic/large cell |
Neither the clinical stratification nor the pathologic classification has been fully adequate in predicting outcomes. Subsets of children with average-risk medulloblastoma may still do very poorly, with resistance to treatment, early relapse, and dissemination.
Molecular Stratification
The presence of certain molecular markers has been shown to affect survival. Studies showed that nuclear immunoreactivity for β-catenin, CTNNB1 mutation, overexpression of neurotrophin-3 receptor (TRKC3), and monosomy 6 were associated with improved survival, whereas ERBB2 expression and MYCC or OTX2 amplification were associated with poorer outcomes. However, the clinical utility of some of these markers remains limited given conflicting conclusions in reports. Recently, multiple molecular pathways have been implicated in the pathogenesis of medulloblastoma. For example, in some tumors the sonic hedgehog (Shh) pathway is activated and mediates tumorigenesis via the activation of glioma-associated homolog 1 (Gli1); this activation may be through modification of any component of the Shh pathway, including elements such as patched, suppressor of fused (SUFU), and smoothened (SMO) proteins. Gli1 is a transcription factor that promotes proliferation through activation of various oncogenes including cyclinD1 and cyclinD2. In other medulloblastomas, the wingless type (Wnt) pathway seems to mediate activation of several oncogenes that promote tumorigenesis and inhibit apoptosis such as MYC, cyclinD1, and RE1-silencing transcription factor (REST). Using high-density microarrays, recent analysis led to the discovery of other genes altered in 16% of children with medulloblastoma, including histone-lysine N -methyl transferase genes (MLL2 or MLL3).
Multiple independent groups have further used gene and mRNA profiling to discover the presence of at least 4 molecular subtypes of medulloblastoma. The subtypes include tumors associated with: (1) Wnt pathway activation; (2) Shh pathway activation; (3) c-MYC activation (labeled group C); and (4) high levels of the orthodenticle homeobox 2 ( OTX2) and forkhead box protein G1b (FOXG1B ), but lacking high expression of MYC (group D). These groups seem to predict outcome more accurately than historical staging criteria. In one study, when outcomes for children with metastatic disease were controlled for molecular tumor subtype, overall survival was similar in those with or without metastatic disease. The Wnt pathway subtype is associated with excellent prognosis, and to a lesser extent so are tumors with Shh activation. Group C tumors (c-MYC amplified) have poor outcomes. Group D patients have increased heterogeneity in their outcomes, implying that additional factors are needed to differentiate this group. Reports have demonstrated that immunopositivity for follistatin-like 5 (FSTL5) identified a cohort of patients at high risk for relapse and death. As greater than 50% of non-Wnt/non-Shh tumors displayed FSTL5 negativity, some group D tumors may potentially carry a better prognosis.
Treatment of Medulloblastoma
The treatment of medulloblastoma is complex and usually involves a combination of surgery, radiation therapy, and chemotherapy. The role of surgery was recognized in the early 1900s by Harvey Cushing, and studies subsequently demonstrated that residual tumor bulk is one of the most important predictors for PFS in medulloblastoma. Surgery can be complicated in up to 20% of posterior fossa tumors by cerebellar mutism or posterior fossa syndrome, which typically arises hours to 1 to 2 days after resection. This condition is characterized by speech impairment progressing to significant mutism, hypotonia, ataxia, and emotional lability. It is thought to be due to an injury in the dentate nuclei and their efferent pathways. However, Cushing recognized that tumor resection alone was inadequate, as most of his surgically treated patients suffered relapse. Focal radiotherapy was thus used as adjuvant therapy, and evolved to encompass the posterior fossa. After poor survival rates were noted with focal radiotherapy alone, craniospinal irradiation (CSI) was used with resultant improved survival. Current standard radiotherapy is, therefore, CSI with a focal boost to the posterior fossa and other areas of disease. Standard doses were historically 36 Gy of CSI for both average-risk and high-risk patients, with a focal boost to 54 Gy.
Radiation to the developing brain is fraught with complications, including vasculopathy with the risk of stroke and endocrine complications. Neurocognitive sequelae have been among the most troubling, with full-scale intelligence quotient (IQ) declines of 2 to 9 points per year after irradiation, and greater IQ deficits associated with younger age or higher doses at radiotherapy ; thus, attempts have been made to reduce the dose of radiotherapy. Such attempts were more successful with the addition of chemotherapy, which was able to augment radiotherapy and improve outcomes.
Average-Risk Medulloblastoma
Children with average-risk medulloblastoma have postsurgical residual tumor equal to or less than 1.5 cm 2 on magnetic resonance imaging (MRI), no evidence of disseminated disease in the preoperative or postoperative MRI, postoperative lumbar cerebrospinal fluid that displays no tumor cells (M0), and nonanaplastic/large-cell histopathology. Because of the relatively good survival but substantial adverse events with standard treatment strategies, multiple trials have examined dose reductions of CSI to 23.40 Gy without adjuvant chemotherapy. These studies showed a potentially lesser negative impact on neurocognition with less significant IQ point decreases of 10 to 15 points, but with higher relapse rates (5-year PFS was 67% in the full-dose CSI arm and 52% in the reduced-dose CSI arm). By contrast, when adjuvant chemotherapy (lomustine [CCNU], vincristine, and cisplatin) was added during and after radiotherapy, survival rates compared favorably with those obtained in studies using full-dose radiation therapy alone (5-year PFS 79%). Subsequent studies prospectively compared 2 adjuvant chemotherapy regimens: CCNU, cisplatin, and vincristine or cyclophosphamide, cisplatin, and vincristine; this study showed no difference in the 5-year EFS between the treatment groups (81% and 86%, respectively). A separate, smaller trial using 23.4 Gy CSI followed by 4 cycles of high-dose chemotherapy (vincristine, cyclophosphamide, and cisplatin) with stem cell support showed a 5-year EFS of 83%. The use of intensive preirradiation chemotherapy (ifosfamide, etoposide, intravenous high-dose methotrexate, cisplatin, and cytarabine) resulted in a poorer 3-year EFS and worsened myelotoxicity when compared with immediate radiotherapy (35 Gy) with concomitant vincristine followed by cisplatin, CCNU, and vincristine (65% vs 78%, respectively). Hence, chemotherapy is typically given after radiotherapy.
The feasibility of further dose reduction of radiotherapy to 18 Gy for patients between 3 and 7 years is currently being investigated, as is a reduction in the field of the boost based on number of pilot studies. Further modification of chemotherapy, such as dose reduction of cisplatin to minimize ototoxicity, is also being explored.
High-Risk Medulloblastoma
Despite treatment with higher doses of CSI and chemotherapy, children with high-risk medulloblastoma continue to have poor outcomes (5-year EFS 50%–60%). Thus no dose reduction in CSI has been implemented in these patients. The role of chemotherapy in this disease has been investigated in multiple clinical trials. When adjuvant chemotherapy (consisting of CCNU, vincristine, and prednisone) was used after radiotherapy, the estimated 5-year EFS was 59% compared with 50% for patients treated with radiotherapy alone. However, when only including patients with more extensive disease, the group that received adjuvant chemotherapy showed significantly better EFS when compared with similar patients treated with radiotherapy alone (48% vs 0%). Preirradiation chemotherapy (cisplatin and etoposide) followed by adjuvant chemotherapy (cyclophosphamide and etoposide) showed no impact on 5-year PFS and overall survival (OS) when compared with radiotherapy after surgical resection, followed by chemotherapy (cisplatin, etoposide, cyclophosphamide, and vincristine). Other approaches such as a dose-intensive, alkylator-based regimen of chemotherapy (4 cycles of cyclophosphamide, cisplatin, and vincristine) with stem cell support have been used after maximum resection and radiotherapy, resulting in a similarly improved outcome (5-year EFS 70%) but with substantial reduction in the duration of treatment (4 months vs 12 months). The Children’s Oncology Group (COG) is currently investigating the efficacy of carboplatin administered concomitantly with radiation and isotretinoin as a proapoptotic agent administered with 6 cycles of adjuvant chemotherapy.
Medulloblastoma in Young Children
Patients younger than 3 years generally have a poor prognosis with an estimated 5-year PFS of 30% to 40%, attributable to an increased incidence of neuraxis dissemination, inability or physician/patient reluctance to administer full-dose radiotherapy, and the possible presence of different genetic alterations. One notable exception is the relatively good outcome of patients with medulloblastoma with desmoplastic histology, which can be treated with chemotherapy alone with a 5-year PFS of 65% to 85%. Given the risks of radiotherapy-induced severe neurocognitive sequelae in very young children, the overall strategy has been to use chemotherapy in an attempt to delay or avoid irradiation. One trial that attempted to delay radiotherapy by 1 to 2 years using intensive chemotherapy consisting of vincristine, cyclophosphamide, etoposide, and cisplatin resulted in early failure (most failures occurred during the first 6 months of chemotherapy) and poor 5-year EFS and OS (32% and 40%, respectively). In this study, infants without metastatic disease who also had a gross total resection had slightly better outcome, with 5-year OS of 69%. Other chemotherapy regimens that have been attempted include combinations variably including procarbazine, ifosfamide, intravenous/intrathecal methotrexate, cisplatin, cytarabine, and vincristine. These regimens were associated with relatively poor 5-year OS (35%). A study comparing an induction regimen based on cyclophosphamide and cisplatin with one based on ifosfamide and carboplatin, followed by maintenance chemotherapy, showed no difference between the 2 treatment arms, with 5-year EFS of 32% in both arms. A similarly poor 3-year EFS of 40% resulted after induction chemotherapy based on cisplatin and high-dose methotrexate, followed by consolidation with high-dose chemotherapy and stem cell rescue. Radiation in this study was given at a dose of 23.4 Gy for patients with evidence of residual disease at the end of induction chemotherapy. The COG recently completed a pilot trial in which 3 courses of standard chemotherapy followed by 3 courses of high-dose chemotherapy with stem cell rescue preliminarily showed slightly superior outcomes, with a 3-year EFS of 67% in M0 patients.
There is no consensus regarding the use of radiation therapy in children younger than 3 years, and despite the use of varying intensive chemotherapy regimens, CSI could only be delayed by 1 year in up to 34% of patients because of early recurrence or progressive disease.
Recurrent Medulloblastoma
Recurrent and progressive medulloblastomas have very poor prognoses, with postrecurrence 2-year OS of approximately 25% despite aggressive treatment regimens. Only anecdotal reports have described prolonged survival after relapse. It has been suggested that early identification of recurrence is associated with a longer survival. Current suggested approaches include the use of reirradiation, which has some limited data on its efficacy, especially in patients without gross disease, with 48% 5-year EFS. A metronomic combination of oral etoposide, cyclophosphamide, thalidomide, celecoxib, and fenofibrate, augmented with alternating courses of intrathecal etoposide and liposomal cytarabine in combination with biweekly intravenous bevacizumab, was also explored in a study that included 6 patients with recurrent medulloblastoma, with resulting 2-year OS of 80% and PFS of 53%.
For younger patients with metastatic or recurrent disease, the use of radiotherapy is usually based on physician’s discretion and family wishes, but may have some utility in salvaging patients.
Future Directions
Future approaches for the treatment of medulloblastoma will likely be based on an increased understanding of the molecular features of individual tumors and the development of specific, patient-tailored, molecularly targeted therapies. Using this improved knowledge of underlying molecular characteristics, risk stratification may be more accurately assigned to particular patients, resulting in more appropriate treatment regimen applications and decreased toxicity. Such treatment is already undergoing investigation, using therapeutics targeting the Shh with SMO small-molecule antagonist (GDC-0449). Antiangiogenic therapies such as bevacizumab, inhibitor of poly(ADP-ribose) polymerase (PARP), and anti–insulin-like growth factor I receptor monoclonal antibody (IMC-A12) in combination with an mTOR inhibitor (temsirolimus) are also being examined in different pediatric CNS tumors including medulloblastoma.
Other studies are currently examining the feasibility of adding the histone deacetylase inhibitor, suberoylanilide hydroxamic acid (SAHA), and isotretinoin to standard induction-chemotherapy drugs. This approach is based on preclinical studies suggesting that isotretinoin induces apoptosis through promoting BMP-2 transcription and clinical studies suggesting isotretinoin synergy with cisplatin. SAHA has also been shown to induce apoptosis in medulloblastoma cell lines.
[Tags: Medulloblastoma, Average-risk medulloblastoma, High-risk medulloblastoma, Wnt pathway, Shh pathway, Recurrent medulloblastoma, Medulloblastoma at young age, Molecular stratification of medulloblastoma, Clinical stratification of medulloblastoma, Radiotherapy dose reduction in medulloblastoma].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree