Glioblastoma multiforme is the most common primary malignant tumor of the central nervous system. Despite new insights into glioblastoma pathophysiology, the prognosis for patients diagnosed with this highly aggressive tumor remains bleak. Current treatment regimens combine surgical resection and chemoradiotherapy, providing an increase in median overall survival from 12.1 to 14.6 months. Ongoing preclinical and clinical studies evaluating the efficacy of novel therapies provide hope for increasing survival benefit. This article reviews the advancements in glioblastoma treatment in newly diagnosed and recurrent glioblastoma, including novel therapies such as antiangiogenic agents, mammalian target of rapamycin inhibitors, poly(ADP-ribose) polymerase-1 inhibitors, and immunotherapies.
- •
Current first-line treatment regimens combine surgical resection and chemoradiotherapy, providing a slight increase in overall survival.
- •
Age on its own should not be used as an exclusion criterion for glioblastoma multiforme (GBM) treatment, but performance status should be factored heavily into the decision-making process for treatment planning.
- •
Despite aggressive initial treatment, most patients develop recurrent disease, which can be treated with reresection, systemic treatment with targeted agents or cytotoxic chemotherapy, reirradiation, or radiosurgery.
- •
Research into novel therapies is investigating alternative temozolomide regimens, convection-enhanced delivery, immunotherapy, gene therapy, antiangiogenic agents with and without cytotoxic chemotherapy, poly(adenosine diphosphate-ribose) polymerase-1 inhibitors, and targeting of tumor growth-promoting pathways or cancer stem cell signaling pathways.
- •
Given the aggressive and resilient nature of GBM, continued efforts to better understand GBM pathophysiology are required to discover novel targets for future therapies.
Introduction
Nearly 10,000 cases of glioblastoma multiforme (GBM) are diagnosed annually in the United States, making GBM the most common primary malignant tumor of the central nervous system (CNS). Ongoing research has drastically advanced our understanding of GBM pathophysiology; however, meaningful survival improvement has not occurred.
With near-certain relapse, prognostic factors are important in counseling patients and selecting individual patients for specific treatment modalities. Nomograms can be helpful in predicting the prognosis of individual patients, taking into account pertinent molecular and prognostic factors. Age, performance status, extent of surgical resection, temozolomide (TMZ) treatment, O 6 -methylguanine-DNA methyltransferase (MGMT) promoter methylation status, and neurologic functioning as expressed by the Mini-Mental State Examination score are important prognostic factors.
Although no treatment has proved curative and overall mortality remains high, continued research promises to lead to novel individualized and localized therapies.
Current treatments
Current treatment protocols for GBM combine surgery, chemotherapy, and radiation, providing palliation and moderate survival benefit. For newly diagnosed patients with GBM, standard treatment includes maximal surgical resection followed by combined radiotherapy and chemotherapy.
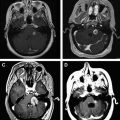
Surgical Resection
The goal of surgery in GBM treatment is to provide maximal tumor resection, with preservation or restoration of neurologic function. Recent studies have shown gross total resection to enhance the overall survival (OS) in GBM. When maximal total resection is not feasible, near-total and subtotal resection provides additional survival benefit. In a study of 451 patients with GBM undergoing primary resection, the median survival after gross-total resection, near-total resection, and subtotal resection was 13, 11, and 8 months, respectively.
Advances in image-guided surgical techniques, including intraoperative magnetic resonance imaging (MRI), cortical mapping, and stereotactic surgery have assisted in the ability to safely increase the extent of tumor resection. These new modalities have had a significant impact on patients with tumors in eloquent cortical areas where resection is frequently abandoned before total removal to avoid neurologic deficits. A phase III trial of 322 patients showed the benefit of fluorescence-guided tumor resections with 5-aminolevulinic acid. When combined with intraoperative monitoring and cortical and subcortical stimulation, fluorescence guidance provides the surgeon with direct visualization of tumor borders and allows for the largest possible resection with minimal neurologic deficits.
Chemotherapy-Impregnated Wafers
Implantation of biodegradable carmustine (1,2-bis[2-chloreoethyl]-1-nitrosourea, BCNU) wafers (CW) is an approved therapeutic option for patients with newly diagnosed and relapsed glioblastoma. These wafers are placed in the surgical resection site at the time of initial operative debulking. The chemotherapeutic agent is released into surrounding brain tissue beginning immediately after tumor resection and lasting for several weeks. Use of CW results in a statistically significant benefit in the OS of patients undergoing initial surgery for malignant gliomas (13.9 vs 11.6 months). However, subgroup analysis failed to show significant benefit in GBM.
In patients undergoing primary resection and adjuvant radiotherapy, the addition of CW and concomitant TMZ provides significant survival benefit over CW alone. Patients undergoing radiation therapy (XRT) + CW + TMZ compared with patients undergoing XRT + CW alone showed an increase in median OS (21.3 vs 12.4 months). In addition, 2-year survival was found to be 39% of patients undergoing XRT + CW + TMZ therapy versus 18% with XRT + CW. Because this study was underpowered to compare XRT + CW + TMZ cohorts with XRT + TMZ alone, future prospective studies are required to characterize the role of CW in standard of care therapy.
Although integrating CW into the standard adjuvant regimen with concomitant chemotherapy has proved safe and feasible, its use remains physician dependent. In phase III studies, the wafers have been found to delay wound healing and are associated with edema, requiring subsequent steroids, seizures, and blood-brain barrier (BBB) disruption, making the interpretation of follow-up MRI unreliable. Often, the pathologic diagnosis is not known before surgical resection, making CW implantation problematic without proper preparation by the surgeon. In addition, placement of CW can lead to exclusion from enrollment in clinical trials.
Chemoradiotherapy
After maximum surgical resection or biopsy, chemoradiotherapy has been established as the standard treatment administered postoperatively. Radiotherapy uses high-dose volume incorporating the enhancing tumor plus a limited margin to plan the target volume. The total dose delivered is in the range of 50 to 60 Gy in fraction sizes of 1.8 to 2.0 Gy.
Before TMZ therapy, the role of chemotherapy in GBM was controversial. A meta-analysis of 12 randomized trials, which included more than 3000 patients, showed an increase in 1-year survival from 40% to 46% with chemotherapy. One common treatment regimen was PCV (procarbazine, CCNU [lomustine], and vincristine).
In 2005, in an international randomized phase III trial of 573 patients with GBM the European Organization for Research and Treatment of Cancer (EORTC) and National Cancer Institute of Canada (NCIC) reported a significant improvement in survival with the early addition of TMZ to XRT compared with XRT alone. Follow-up results after 5 years showed continued benefit of adjuvant TMZ with XRT with OS of 9.8% compared with 1.9% in the radiotherapy alone group. Median OS rates for radiotherapy + TMZ versus radiotherapy alone were 14.6 months and 12.1 months, respectively. Progression-free survival (PFS) rates for patients receiving radiotherapy + TMZ compared with radiotherapy alone were 11.2% and 1.8% at 2 years, 6.0% and 1.3% at 3 years, 5.6% and 1.3% at 4 years, and 4.1% and 1.3% at 5 years. Treatment is generally well tolerated, with most notable toxicities including myelosuppression, thromboembolic events, fatigue, pneumonia, nausea, vomiting, rash, constipation, and arthralgias. The dose-limiting toxicity of TMZ is myelosuppression, with any grade 3 or 4 hematologic toxic effect found to affect 14% of patients during adjuvant TMZ therapy. Four percent of patients experienced a grade 3 or 4 neutropenia and 11% experienced a grade 3 or 4 thrombocytopenia.
Standard dosing for concomitant TMZ therapy is 75 mg/m 2 /d given daily during XRT followed by 150 to 200 mg/m 2 /d for 5 days every 28 days for a total of 6 cycles. Multiple studies are evaluating different dosing protocols as well as the combination of TMZ with other chemotherapeutic and targeted agents in the treatment of GBM. A randomized phase III study (Radiation Therapy Oncology Group [RTOG] 0525) comparing standard adjuvant TMZ and a dose-dense schedule (75–100 mg/m 2 daily, days 1–21) in 833 newly diagnosed patients with GBM found no improvement in OS with dose-dense TMZ regardless of MGMT methylation status.
Treatment of Elderly Patients
The incidence of GBM increases with age, with a median age of onset of 60 years. Patient survival decreases almost linearly beyond the age of 45 years. The median survival times in elderly patients are significantly less than younger patients (4–11 months). Both historical series and clinical trials have found the 2-year survival of less than 5% in patients older than 65 years compared with 26% in patients younger than 50 years. However, poor outcomes and poor response to toxic therapies have resulted in more aggressive treatments being withheld from the elderly population with GBM.
Large population-based studies suggest that nearly 50% of patients with GBM older than 65 years do not receive the standard of care treatment with surgical debulking or radiotherapy. A retrospective review of 394 elderly patients with GBM from Memorial Sloan Kettering Cancer Center found significant survival benefit in elderly patients aged 65 years or older undergoing gross total resection compared with subtotal resection or biopsy (60% vs 40% decrease in risk of death). One study found OS increased from 17 to 30 weeks when patients had biopsy and radiation therapy compared with surgical resection of the entire contrast-enhancing lesion and radiation, respectively. Similar studies show the benefit of radiation therapy alone compared with supportive care. A total of 81 patients aged 70 years or older from 10 institutions with GBM had a median OS of 29.1 weeks when treated with supportive care and radiotherapy compared with 16.9 weeks in those patients receiving supportive care alone. Median PFS was 14.9 weeks and 5.4 weeks for radiotherapy and supportive care compared with supportive care alone, respectively.
In an attempt to shorten treatment duration, hypofractionated radiotherapy is often used, which gives larger radiation doses per fraction in fewer total fractions over a shorter period of time. A common regimen of 40 Gy in 15 fractions over 3 weeks has been shown to be equivalent in older patients to the standard 6-week schedule of 60 Gy in 30 fractions. This is a reasonable regimen to consider in older patients with borderline performance status for whom the ability to tolerate a 6-week course of concurrent TMZ and radiation is in question.
A prospective study of 79 elderly patients with GBM older than 65 years investigated the benefit of chemotherapy (PCV or TMZ) in patients undergoing surgery and radiotherapy. Three groups of patients were analyzed after maximal surgical resection. The groups were treated with radiotherapy alone (n = 24), radiotherapy with adjuvant PCV (n = 32), or radiotherapy with adjuvant TMZ (n = 23). The group receiving TMZ had a significant survival benefit compared with those patients receiving radiotherapy alone (14.9 months vs 11.2 months). Whereas OS did not differ between patients receiving adjuvant TMZ or PCV, the PFS was significantly longer in those receiving adjuvant TMZ. The 6-month and 12-month PFS was 56.25% and 15.6% in those patients receiving PCV and 87% and 47.4% in those treated with TMZ. In addition, TMZ therapy was better tolerated, because PCV was associated with more frequent hematologic toxicity.
The 5-year follow-up analysis of the EORTC-NCIC trial published by Stupp and colleagues reported a benefit of concomitant and adjuvant TMZ and radiotherapy in all clinical prognostic subgroups, including patients aged 60 to 70 years. At 2 years, the median OS was 21.8% in those patients receiving combined therapy and 5.7% in those patients receiving radiotherapy alone. This effect was maintained at 5 years with median OS of 6.6% and 0.0%.
A phase II study analyzed the use of TMZ in elderly patients with newly diagnosed GBM and poor performance status. The study, comparing TMZ treatment with supportive care alone, found TMZ to be well tolerated, improve functional status, and increase OS in 70 patients older than 70 years with newly diagnosed GBM and Karnofsky performance score (KPS) less than 70. Furthermore, when patients had a methylated MGMT promoter, TMZ had a more significant impact on PFS and OS.
Age on its own should not be used as an exclusion criterion for GBM treatment, but performance status should be factored heavily into the decision-making process for treatment planning.
Current treatments
Current treatment protocols for GBM combine surgery, chemotherapy, and radiation, providing palliation and moderate survival benefit. For newly diagnosed patients with GBM, standard treatment includes maximal surgical resection followed by combined radiotherapy and chemotherapy.
Surgical Resection
The goal of surgery in GBM treatment is to provide maximal tumor resection, with preservation or restoration of neurologic function. Recent studies have shown gross total resection to enhance the overall survival (OS) in GBM. When maximal total resection is not feasible, near-total and subtotal resection provides additional survival benefit. In a study of 451 patients with GBM undergoing primary resection, the median survival after gross-total resection, near-total resection, and subtotal resection was 13, 11, and 8 months, respectively.
Advances in image-guided surgical techniques, including intraoperative magnetic resonance imaging (MRI), cortical mapping, and stereotactic surgery have assisted in the ability to safely increase the extent of tumor resection. These new modalities have had a significant impact on patients with tumors in eloquent cortical areas where resection is frequently abandoned before total removal to avoid neurologic deficits. A phase III trial of 322 patients showed the benefit of fluorescence-guided tumor resections with 5-aminolevulinic acid. When combined with intraoperative monitoring and cortical and subcortical stimulation, fluorescence guidance provides the surgeon with direct visualization of tumor borders and allows for the largest possible resection with minimal neurologic deficits.
Chemotherapy-Impregnated Wafers
Implantation of biodegradable carmustine (1,2-bis[2-chloreoethyl]-1-nitrosourea, BCNU) wafers (CW) is an approved therapeutic option for patients with newly diagnosed and relapsed glioblastoma. These wafers are placed in the surgical resection site at the time of initial operative debulking. The chemotherapeutic agent is released into surrounding brain tissue beginning immediately after tumor resection and lasting for several weeks. Use of CW results in a statistically significant benefit in the OS of patients undergoing initial surgery for malignant gliomas (13.9 vs 11.6 months). However, subgroup analysis failed to show significant benefit in GBM.
In patients undergoing primary resection and adjuvant radiotherapy, the addition of CW and concomitant TMZ provides significant survival benefit over CW alone. Patients undergoing radiation therapy (XRT) + CW + TMZ compared with patients undergoing XRT + CW alone showed an increase in median OS (21.3 vs 12.4 months). In addition, 2-year survival was found to be 39% of patients undergoing XRT + CW + TMZ therapy versus 18% with XRT + CW. Because this study was underpowered to compare XRT + CW + TMZ cohorts with XRT + TMZ alone, future prospective studies are required to characterize the role of CW in standard of care therapy.
Although integrating CW into the standard adjuvant regimen with concomitant chemotherapy has proved safe and feasible, its use remains physician dependent. In phase III studies, the wafers have been found to delay wound healing and are associated with edema, requiring subsequent steroids, seizures, and blood-brain barrier (BBB) disruption, making the interpretation of follow-up MRI unreliable. Often, the pathologic diagnosis is not known before surgical resection, making CW implantation problematic without proper preparation by the surgeon. In addition, placement of CW can lead to exclusion from enrollment in clinical trials.
Chemoradiotherapy
After maximum surgical resection or biopsy, chemoradiotherapy has been established as the standard treatment administered postoperatively. Radiotherapy uses high-dose volume incorporating the enhancing tumor plus a limited margin to plan the target volume. The total dose delivered is in the range of 50 to 60 Gy in fraction sizes of 1.8 to 2.0 Gy.
Before TMZ therapy, the role of chemotherapy in GBM was controversial. A meta-analysis of 12 randomized trials, which included more than 3000 patients, showed an increase in 1-year survival from 40% to 46% with chemotherapy. One common treatment regimen was PCV (procarbazine, CCNU [lomustine], and vincristine).
In 2005, in an international randomized phase III trial of 573 patients with GBM the European Organization for Research and Treatment of Cancer (EORTC) and National Cancer Institute of Canada (NCIC) reported a significant improvement in survival with the early addition of TMZ to XRT compared with XRT alone. Follow-up results after 5 years showed continued benefit of adjuvant TMZ with XRT with OS of 9.8% compared with 1.9% in the radiotherapy alone group. Median OS rates for radiotherapy + TMZ versus radiotherapy alone were 14.6 months and 12.1 months, respectively. Progression-free survival (PFS) rates for patients receiving radiotherapy + TMZ compared with radiotherapy alone were 11.2% and 1.8% at 2 years, 6.0% and 1.3% at 3 years, 5.6% and 1.3% at 4 years, and 4.1% and 1.3% at 5 years. Treatment is generally well tolerated, with most notable toxicities including myelosuppression, thromboembolic events, fatigue, pneumonia, nausea, vomiting, rash, constipation, and arthralgias. The dose-limiting toxicity of TMZ is myelosuppression, with any grade 3 or 4 hematologic toxic effect found to affect 14% of patients during adjuvant TMZ therapy. Four percent of patients experienced a grade 3 or 4 neutropenia and 11% experienced a grade 3 or 4 thrombocytopenia.
Standard dosing for concomitant TMZ therapy is 75 mg/m 2 /d given daily during XRT followed by 150 to 200 mg/m 2 /d for 5 days every 28 days for a total of 6 cycles. Multiple studies are evaluating different dosing protocols as well as the combination of TMZ with other chemotherapeutic and targeted agents in the treatment of GBM. A randomized phase III study (Radiation Therapy Oncology Group [RTOG] 0525) comparing standard adjuvant TMZ and a dose-dense schedule (75–100 mg/m 2 daily, days 1–21) in 833 newly diagnosed patients with GBM found no improvement in OS with dose-dense TMZ regardless of MGMT methylation status.
Treatment of Elderly Patients
The incidence of GBM increases with age, with a median age of onset of 60 years. Patient survival decreases almost linearly beyond the age of 45 years. The median survival times in elderly patients are significantly less than younger patients (4–11 months). Both historical series and clinical trials have found the 2-year survival of less than 5% in patients older than 65 years compared with 26% in patients younger than 50 years. However, poor outcomes and poor response to toxic therapies have resulted in more aggressive treatments being withheld from the elderly population with GBM.
Large population-based studies suggest that nearly 50% of patients with GBM older than 65 years do not receive the standard of care treatment with surgical debulking or radiotherapy. A retrospective review of 394 elderly patients with GBM from Memorial Sloan Kettering Cancer Center found significant survival benefit in elderly patients aged 65 years or older undergoing gross total resection compared with subtotal resection or biopsy (60% vs 40% decrease in risk of death). One study found OS increased from 17 to 30 weeks when patients had biopsy and radiation therapy compared with surgical resection of the entire contrast-enhancing lesion and radiation, respectively. Similar studies show the benefit of radiation therapy alone compared with supportive care. A total of 81 patients aged 70 years or older from 10 institutions with GBM had a median OS of 29.1 weeks when treated with supportive care and radiotherapy compared with 16.9 weeks in those patients receiving supportive care alone. Median PFS was 14.9 weeks and 5.4 weeks for radiotherapy and supportive care compared with supportive care alone, respectively.
In an attempt to shorten treatment duration, hypofractionated radiotherapy is often used, which gives larger radiation doses per fraction in fewer total fractions over a shorter period of time. A common regimen of 40 Gy in 15 fractions over 3 weeks has been shown to be equivalent in older patients to the standard 6-week schedule of 60 Gy in 30 fractions. This is a reasonable regimen to consider in older patients with borderline performance status for whom the ability to tolerate a 6-week course of concurrent TMZ and radiation is in question.
A prospective study of 79 elderly patients with GBM older than 65 years investigated the benefit of chemotherapy (PCV or TMZ) in patients undergoing surgery and radiotherapy. Three groups of patients were analyzed after maximal surgical resection. The groups were treated with radiotherapy alone (n = 24), radiotherapy with adjuvant PCV (n = 32), or radiotherapy with adjuvant TMZ (n = 23). The group receiving TMZ had a significant survival benefit compared with those patients receiving radiotherapy alone (14.9 months vs 11.2 months). Whereas OS did not differ between patients receiving adjuvant TMZ or PCV, the PFS was significantly longer in those receiving adjuvant TMZ. The 6-month and 12-month PFS was 56.25% and 15.6% in those patients receiving PCV and 87% and 47.4% in those treated with TMZ. In addition, TMZ therapy was better tolerated, because PCV was associated with more frequent hematologic toxicity.
The 5-year follow-up analysis of the EORTC-NCIC trial published by Stupp and colleagues reported a benefit of concomitant and adjuvant TMZ and radiotherapy in all clinical prognostic subgroups, including patients aged 60 to 70 years. At 2 years, the median OS was 21.8% in those patients receiving combined therapy and 5.7% in those patients receiving radiotherapy alone. This effect was maintained at 5 years with median OS of 6.6% and 0.0%.
A phase II study analyzed the use of TMZ in elderly patients with newly diagnosed GBM and poor performance status. The study, comparing TMZ treatment with supportive care alone, found TMZ to be well tolerated, improve functional status, and increase OS in 70 patients older than 70 years with newly diagnosed GBM and Karnofsky performance score (KPS) less than 70. Furthermore, when patients had a methylated MGMT promoter, TMZ had a more significant impact on PFS and OS.
Age on its own should not be used as an exclusion criterion for GBM treatment, but performance status should be factored heavily into the decision-making process for treatment planning.
Recurrent disease
Despite aggressive initial treatment with surgical resection, radiotherapy, and chemotherapy virtually all patients with GBM relapse. Unlike newly diagnosed GBM, there is currently no standard of care treatment of GBM relapse. Ongoing clinical trials are investigating targeted agents with various mechanisms of action as salvage therapy for patients with recurrent GBM ( Table 1 ).
| Drug | Mechanism of Action | Phase | Number of Patients | 6-Month PFS (%) | Median OS (wk) | Median PFS (wk) | Reference |
|---|---|---|---|---|---|---|---|
| Meta-analysis | Various | II | 225 | 15 | 25 | 9 | Wong et al |
| Meta-analysis | Various | II | 437 | 16 | 30 | Lamborn et al | |
| BCNU a | Alkylating agent | Retrospective | 35 | 13 | 22 | 11 | Reithmeier et al |
| Lomustine | Alkylating agent | III | 92 | 19 | 31 | 7 | Wick et al |
| Enzastaurin | Protein kinase C β inhibitor | III | 174 | 11 | 28 | 6 | Wick et al |
| Temsirolimus (CCI-779) | mTOR inhibitor | II | 65 | 8 | 19 | 10 | Galanis et al |
| Erlotinib | EGFR tyrosine kinase inhibitor | II | 48 | 17 | 43 | Cloughesy et al | |
| II | 54 | 11 b | 33 | Van den Bent et al | |||
| Erlotinib + sirolimus | EGFR TKI + mTOR inhibitor | II | 32 | 3 | 34 | 7 | Reardon et al |
| Vorinostat | Histone deacetylase inhibitor | II | 66 | 17 | 25 | Galanis et al | |
| Imatinib | Multiple TKI, including PDGFR | II | 51 | 16 | 25 | 8 | Raymond et al |
| Imatinib + hydroxyurea | Multiple TKI + antimetabolite | II | 231 | 11 | 26 | Reardon et al | |
| II | 33 | 27 | 49 | 14 | Reardon et al |
a BCNU was associated with significant toxicity including pulmonary embolism, pulmonary fibrosis, and myelosuppression.
b 6-month PFS in control arm of carmustine or TMZ was 24% and erlotinib was believed to have insufficient single-agent activity.
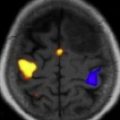
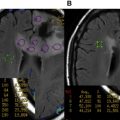
Pseudoprogression
Before initiating treatment of recurrent GBM, true disease progression must be distinguished from pseudoprogression. Pseudoprogression is a treatment-related reaction, occurring frequently with combination radiotherapy + TMZ, which is visualized as increased enhancement or edema on MRI. The reaction is highly suggestive of disease progression but without an increase in tumor activity. This local tissue reaction is triggered by a treatment-induced increase in vessel permeability, inflammatory infiltration, and resulting edema. In most cases, pseudoprogression resolves even without treatment, although with a variable time course, rendering distinction from tumor progression difficult.
An analysis of 85 patients with GBM treated with radiotherapy + TMZ found 21% of patients had pseudoprogression, of whom 67% remained asymptomatic despite the new radiologic changes. Another study found similar results with 31% of 103 patients with GBM undergoing pseudoprogressive changes and 66% remaining asymptomatic. In addition, for those patients with enlarging lesions on first MRI after radiation, Brandes and colleagues found a 91.3% probability of pseudoprogression in patients with methylated MGMT promoter tumors and a 59% probability of early disease progression in unmethylated MGMT promoter tumors.
Current data suggest the need for novel imaging techniques or biochemical markers to better distinguish pseudoprogression from true progression. This strategy prevents patients from undergoing unnecessary surgical interventions and premature discontinuance of adjuvant treatments.
Re-Resection
The US National Institutes of Health (NIH) recurrent GBM scale has been validated for use in identifying patients likely to benefit from repeat surgery. To determine a patient’s score, 1 point is assigned for the presence of each of the following factors: KPS score 80 or less, tumor volume 50 cm 3 or greater, and motor-speech-middle cerebral artery score 2 or greater. Patient survival after surgery can be stratified based on their total score, ranging from 0 to 3. Good (0 points), intermediate (1–2 points), and poor (3 points) prognostic groups were found to have postoperative survival times of 10.8, 4.5, and 1.0 months, respectively.
Several case series have shown increased survival periods in patients undergoing reoperations. A study of 301 patients, with 46 undergoing re-resection, found a significant increase in survival compared with those treated with the same protocols without reoperations (36 vs 23 weeks). However, most of these studies acknowledge an inherent patient selection bias to perform surgery in patients with high functional status, favorable tumor locations, and minimal medical contraindications.
In a review of studies investigating GBM retreatment strategies, Nieder and colleagues found that median survival in patients undergoing re-resection ranged from 14 to 50 weeks. The role of re-resection by itself remains unclear because most patients receive postoperative radiotherapy or chemotherapy. In a small study of 24 patients undergoing re-resection alone, median survival was 14 weeks. A carefully selected subgroup of 18 patients underwent reoperation and were compared with 36 patients who did not undergo surgery at the time of tumor recurrence. A median survival time of 5 months in the surgical subgroup was significantly longer than 2 months observed in those patients not undergoing surgical intervention.
Chemotherapy-Impregnated Wafers
In patients undergoing re-resection for GBM relapse, carmustine-impregnated wafers have been investigated in combination with other adjuvant therapies. A double-blind, randomized, placebo-controlled study showed the efficacy of local chemotherapy with CW in patients with recurrent GBM. Six-month survival in patients receiving CW was 64% compared with 44% in patients treated with placebo.
A phase II trial showed that efficacy of implanted CW may be improved with the addition of O 6 -benzylguanine, which suppresses tumor O6-alkylguanine-DNA alkyltransferase levels in patients with recurrent GBM. In the 52 patients studied, the 6-month OS was 82%. The median OS was 50.3 weeks and 1-year and 2-year survival rates were 47% and 10%, respectively. Notable toxicities included grade 3 hydrocephalus (9.6%), grade 3 cerebrospinal fluid (CSF) leak (19.2%), and grade 3 CSF/brain infection (13.4%).
Overall, CW implantation has been well tolerated and continues to be used in the multimodality treatment protocols required in GBM, although potential toxicities and exclusion from clinical trials remain a concern.
Bevacizumab
Bevacizumab (10 mg/kg intravenously every 2 weeks) received accelerated approval for the treatment of recurrent GBM in May 2009 because of its effectiveness when used alone or in combination with chemotherapy. In a phase II trial of 35 patients with GBM, Vredenburgh and colleagues found 6-month PFS with bevacizumab + irinotecan was 46% and 6-month OS was 77%. In a phase II trial evaluating the role of bevacizumab alone (n = 85) or in combination with irinotecan (n = 82), the 6-month PFS was 42.6% and 50.3%, respectively. In addition, secondary end points showed OS of 9.2 months for patients treated with bevacizumab alone and 8.7 months for those treated with bevacizumab and irinotecan, although the study was not designed to compare efficacy of these 2 arms of treatment with each other. The study did show a trend for decreasing steroid dose in patients on therapy.
More recently, a phase II trial of daily TMZ + biweekly bevacizumab found 6-month PFS of 18.8%, 6-month median OS of 37 weeks, and 12-month median OS of 31.3%. Although the results were not as good as results seen in bevacizumab monotherapy or bevacizumab/irinotecan combination therapy, this study included heavily pretreated patients with 78% having had 2 or more previous chemotherapy regimens and 12% of patients having had previous treatment with bevacizumab. Combination therapy with bevacizumab and etoposide or erlotinib has failed to show a significant difference from other bevacizumab regimens.
A recent meta-analysis reviewed the efficacy of bevacizumab treatment in 548 patients with recurrent GBM, comprising 15 studies published between 2005 and 2009. Median OS, 6-month PFS, and 6-month OS were 9.3 months, 45%, and 76%, respectively. Although requiring confirmation in clinical trial, the analysis found no difference in bevacizumab dose-response benefit between 5, 10, or 15 mg/kg.
Bevacizumab has shown promising results in small cohort studies; however, because of the direct effects of antiangiogenic agents on vessel permeability, the imaging response analyses are difficult to interpret. Other reported side effects of bevacizumab therapy include intracranial hemorrhage and thrombotic events, including deep venous thrombosis, pulmonary embolus, and ischemic stroke. A retrospective study of 161 patients with recurrent GBM treated with bevacizumab found an incidence of 1.9% and 1.9% for ischemic stroke and intracranial hemorrhage, respectively. Ischemic stroke appeared to be a complication of prolonged antiangiogenic therapy, whereas intratumoral bleeds occurred more frequently in tumor progression.
Despite its efficacy in the treatment of recurrent GBM, patients inevitably relapse after bevacizumab therapy. A retrospective review of 54 patients with recurrent GBM who progressed on a bevacizumab-containing regimen found that a response was rarely seen when patients were retreated with an alternate bevacizumab-containing regimen. After the second bevacizumab regimen, 6-month PFS was 2% and median PFS was 37.5 days.
An ongoing phase III double-blind, placebo-controlled trial (RTOG 0825) that recently completed accrual with 978 patients is investigating concurrent chemoradiation and adjuvant TMZ with bevacizumab compared with chemoradiation and adjuvant TMZ in newly diagnosed GBM. Results from this study will provide valuable insight into the efficacy of bevacizumab therapy and its ability to provide a clear survival benefit in patients with GBM.
TMZ Rechallenge
TMZ is standard of care therapy in newly diagnosed GBM. However, there is no consensus on optimal therapy for GBM relapse. TMZ rechallenge remains 1 therapeutic option available to patients with recurrent disease.
Studies have shown TMZ rechallenge to be effective when dosed continuously. Perry and colleagues investigated a continuous TMZ dose of 50 mg/m 2 and found 6-month PFS was 57% in patients who relapsed after completing standard concomitant and adjuvant TMZ.
Several dose-intensive schedules have been investigated in recurrent GBM. Twenty-eight patients with GBM were treated with 75 mg/m 2 /d for 42 consecutive days in a 70-day cycle. Six-month PFS was 19% and OS was 7.7 months. Brandes and colleagues investigated the 75 mg/m 2 /d dose for 21 days every 28 days. Six-month PFS was found to be 30.3%, and OS at 6 months and 1 year was 73% and 38%, respectively. Furthermore, in patients with methylated MGMT, the median survival and percentage of patients alive at 1 year were 48.2 weeks and 50%, respectively. In those patients with unmethylated MGMT, the median survival was 34.7 weeks and 1-year survival was 21.4%. Although prognosis was better in patients with methylated MGMT, there was no clear difference in response and 6-month PFS in relation to MGMT status.
An alternating weekly regimen (1 week on/1 week off) of TMZ was investigated in a randomized, phase II trial of 64 patients with recurrent GBM. TMZ was administered at 150 mg/m 2 on days 1 to 7 and 15 to 21 of 28-day cycles. Six-month and 12-month PFS was 43.8% and 12.5%, respectively. Of the 36 patients with GBM with available tumor specimens, 17 had methylated MGMT and 19 were unmethylated. The median PFS was 19 weeks in patients with unmethylated MGMT and 27 weeks with methylated MGMT; however, these results were not statistically significant. Of the 64 patients with GBM, 22 were chemotherapy naive, whereas 30 had previous nimustine/teniposide therapy, 3 had previous PCV, and 9 had previous lomustine/TMZ. This study is compared with the Brandes and colleagues study in which all patients were chemotherapy naive.
Of importance in recurrent GBM treatment consideration is the expression of the MGMT promoter, which confers resistance to TMZ. Continuous suppression of MGMT activity may prove necessary for maximal benefit. The large, multi-center phase II Canadian (RESCUE) study used a continuous dose-intense TMZ regimen of 50 mg/m 2 /d in patients who had previous exposure to TMZ. This dosing represented dose intensification from 750 to 1000 mg/m 2 /28-d cycle with conventional dosing to 1400 mg/m 2 /28-d cycle. Of the 116 patients studied, the median time on continuous TMZ was 2.7 months, with 15 patients completing 12 months of continuous therapy. The overall 6-month PFS for patients with GBM was 23.9% and median survival was 9.3 months. The most significant benefit was shown in patients with GBM who had completed a previous course of concomitant TMZ/radiotherapy with adjuvant TMZ followed by a drug-free period of at least 2 months (6-month PFS of 35.7%). A similar benefit was seen in patients who progressed before completing 6 cycles of adjuvant TMZ with 6-month PFS of 27.3%. However, those patients who progressed while still on extended adjuvant TMZ therapy beyond 6 cycles did significantly worse than the other 2 groups, with a 6-month PFS of 7.4%. The investigators hypothesized that a continuous regimen may lead to a depletion of MGMT and restoration of TMZ sensitivity, as had been previously reported. In addition, the Perry and colleagues study reported similar benefit in patients with or without methylated MGMT, although the methylated group had a longer interval from time of initial surgery to start of therapy for recurrence.
Reirradiation
Investigators have failed to show significant differences between conventional external beam radiotherapy, stereotactic radiotherapy, or brachytherapy. Median survival after various methods of reirradiation was 26 to 60 weeks. In a recent review of more than 300 patients, palliative reirradiation regimens without additional chemotherapy achieved a PFS at 6 months of 28% to 39% and 1-year survival of 18% to 48%, which compares favorably with targeted systemic therapies that have been evaluated for recurrent GBM.
Given the poor prognosis in patients with GBM, assessment of treatment toxicity and quality of life must be incorporated into therapy decisions. Hypofractionated stereotactic radiotherapy (H-SRT) is able to deliver treatment over a 2-week period compared with the 3-week to 4-week therapy in standard fractionation regimens. A retrospective study of 147 patients between 1994 and 2008 who underwent H-SRT for high-grade gliomas found a significant survival benefit with minimal adverse effects. Using daily fractions of 3.5 Gy with a median dose of 35 Gy, investigators were able to achieve a median survival time of 11 months, comparable with other systemic agents, and minimize toxicities seen at higher doses. The data suggest that higher doses of H-SRT result in improved survival; however, doses greater than 40 Gy have been associated with increased toxicity.
An analysis of 20 patients with recurrent GBM was designed to test the safety and efficacy of H-SRT in combination with bevacizumab treatment. The 6-month PFS for patients with GBM was 65% and median OS was 12.5 months. The overall toxicity in this study was in line with other reports of bevacizumab therapy in patients with malignant glioma. These results suggest that this combination can be evaluated further in the treatment of both newly diagnosed GBM and recurrent GBM.
Radiosurgery
Radiotherapy has shown increasing survival benefit with doses up to 60 Gy, beyond which exposure and toxicity to normal surrounding tissue becomes problematic. Stereotactic radiosurgery (SRS) prevents injury to surrounding normal tissue by producing a sharp radiation decrease outside the target area.
A randomized controlled trial of 203 patients concluded that postoperative SRS followed by external beam radiation therapy (EBRT) and BCNU did not improve the outcome, quality of life, or cognitive functioning of newly diagnosed patients with GBM when compared with EBRT and BCNU alone. Although discouraging for the prospects of SRS in the treatment of GBM, this study analyzed a single timing for SRS therapy and a single combination chemotherapy, leaving room for further investigations.
With the implementation of TMZ into standard GBM therapy, the role of SRS in both newly diagnosed and recurrent GBM continues to be investigated. A retrospective review of 48 patients with GBM treated with SRS between 1991 and 2007, with 22 treated as part of their initial therapy and 26 treated at the time of progression, found an OS benefit in those treated at the time of progression (17.4 vs 15.1 months). In a multivariate analysis, RTOG class III patients, those with more extensive resections, and lack of steroids at the time of SRS had significantly improved OS. The results of this study suggest a role for SRS delivered after radiation therapy in some well-selected patients.
A recent retrospective review analyzed 26 consecutive patients who underwent gamma knife radiosurgery for small recurrent high-grade gliomas (16 with GBM) after radical resection, EBRT, and TMZ between 2004 and 2009. Median OS from SRS was 12.9 months. These results were comparable with the OS from SRS of 13 months found in the prospective cohort of 114 consecutive patients (65 with GBM) published by Kong and colleagues. Several other retrospective studies have reported prolonged survival in patients undergoing SRS for recurrent GBM.
The most likely reason why radiotherapy is unable to effectively control long-term disease is the inability to detect the spread pattern of GBM. An area of significant interest is the use of systemic radiosensitizers that may enhance the effect of focal irradiation as well as exert cytotoxic activity on distant cell populations. Many of these agents have failed to show significant benefit and others continue to undergo preclinical investigation.
Electrical Fields
The disruption of cancer cell mitosis using a low-intensity, medium frequency, alternating electrical field, called tumor treating fields (TTF), was first described by Kirson and colleagues in 2004. In preclinical studies, tumor cell lines exposed to electrical fields for greater than 24 hours entered a stunned, nonproliferative state, unable to undergo mitosis.
Two single-arm, phase I trials in 2007 (10 patients) and 2009 (20 patients) treated patients with TTF. The median survival in 10 patients with recurrent GBM treated with TTF was 62.2 weeks and no adverse events were noted. A follow-up study studied 10 patients with recurrent GBM treated with TTF alone after TMZ maintenance failure and 10 newly diagnosed patients with GBM treated with postoperative TTF and maintenance TMZ therapy. Patients treated with TTF-TMZ combination therapy showed a median PFS of 155 weeks and a median OS of more than 39 months.
In 2010, the US Food and Drug Administration (FDA) narrowly approved the NovoTTF-100A device for the treatment of GBM despite failure to meet the primary end point (OS) in the pivotal trial comparing the device with salvage chemotherapy. The phase III trial that randomized 237 patients with recurrent GBM to treatment with NovoTTF (20–24 h/d, 7 d/wk) or the best standard chemotherapy (BSC) at each physician’s discretion found a median OS of 6.6 months for TTF and 6.0 months for BSC and 6-month PFS of 21% versus 15%. The OS results did not achieve statistical significance. Survey of patients in the study suggested a quality of life benefit with TTF compared with chemotherapy. TTF was well tolerated, with 17% patients experiencing mild to moderate skin rash beneath the electrodes.
Future perspectives
Despite recent advances, the prognosis for newly diagnosed patients with GBM remains dismal. Current treatment regimens provide maximal benefit measured in months and virtually all patients relapse, stimulating the need for continued pursuit of novel therapies.
TMZ: Alternate Regimens
Many studies are investigating alternative dosing schedules of TMZ in both newly diagnosed and patients with recurrent GBM. In a randomized phase II study evaluating 2 TMZ regimens in the adjuvant treatment of newly diagnosed GBM, a dose-dense regimen provided a more significant survival benefit than a metronomic regimen. The median OS of the 31 patients assigned to the dose-dense TMZ treatment group was 17.1 months after receiving 150 mg/m 2 /d for days 1 to 7 and days 15 to 21 of 28-day cycles. All patients received initial EBRT to approximately 60 Gy with concurrent TMZ at 75 mg/m 2 /d through the course of RT. The recently presented results of RTOG 0525, as mentioned earlier, which failed to show a difference between standard and dose-dense TMZ, do raise concerns about efficacy of these alternative regimens.
TMZ rechallenge remains a consideration in recurrent GBM treatment and optional regimens remain under investigation ( Table 2 ).