Abstract
This chapter reviews the pathophysiology, clinical presentation, useful diagnostic studies, and available treatments for breast cancer–associated pericardial disease. Treatment of pericardial involvement in breast cancer is aimed primarily at providing comfort and improved quality of life rather than at prolonging survival.
Keywords
pericardium, pericardial effusion, constrictive pericarditis, pericardial tamponade
The pericardium consists of parietal and visceral surfaces and is composed of relatively inelastic collagen fibers. The pericardium protects the heart from pathologic conditions involving adjacent structures such as the lung, fixes the heart within the thorax, and imposes a physical limitation on the acute expansion of heart volume that may occur with abrupt aortic or mitral regurgitation. The space between the parietal and visceral pericardium contains up to 50 mL of fluid that serves as a lubricant between the two surfaces, which are in constant motion in relation to one another. This space is drained primarily by lymphatics.
This chapter reviews the pathophysiology, clinical presentation, useful diagnostic studies, and available treatments for breast cancer–associated pericardial disease. Treatment of pericardial involvement in breast cancer is aimed primarily at providing comfort and improved quality of life rather than at prolonging survival.
Pericardial Effusion in Breast Cancer
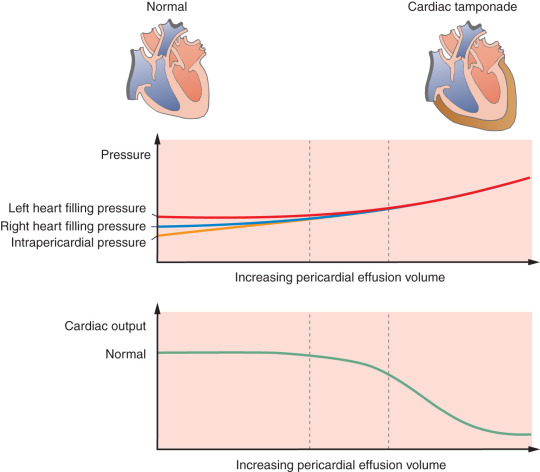
The hemodynamic effect of excess fluid in the pericardial space depends primarily on its volume and rate of accumulation. Because the parietal pericardium is relatively noncompliant, small increments of pericardial fluid that accumulate abruptly (e.g., myocardial rupture) above approximately 200 mL rapidly affect systemic hemodynamics and lead to tamponade. Slow accumulation of fluid (e.g., with metastatic disease) allows the parietal pericardium to stretch to accommodate a substantial increase in volume. Volumes in excess of 1000 or 2000 mL can be accommodated with minimal symptoms if the process is sufficiently slow. It is unusual for the patient with breast cancer to present with acute tamponade and small-volume effusions and much more common for these patients to present with subacute or chronic pericardial effusion associated with moderate to large effusion volume.
Pathology
Metastases from breast cancer most commonly spread to the pericardium via the lymphatic channels, although hematogenous spread and local extension can also occur. In autopsy studies, approximately 20% of patients dying with breast cancer have pericardial metastases, yet clinically apparent pericardial disease develops in only a small subset of these patients. Most commonly, pericardial metastases result in production of a serosanguineous fluid, which, if a sufficient volume collects more rapidly than can be reabsorbed in the confined pericardial space, results in the accumulation of pericardial effusion.
Importantly, nonmalignant involvement of the pericardium is seen in up to 50% of patients with metastatic breast cancer and pericardial effusion. Exposure to chemotherapeutic agents such as doxorubicin or to radiation can cause pericardial effusion. In the patient with breast cancer, pericardial effusion can result from inflammatory or infectious causes as well.
Pathophysiology
The pathophysiology of pericardial tamponade is reviewed in detail in many general cardiology texts. Regardless of etiology, at some point during accumulation of fluid, the parietal pericardium can no longer stretch to accommodate additional volume and pressure within the pericardial space rises. As a result, ventricular filling pressure rises while ventricular volume is constrained secondary to elevated pericardial pressure ( Fig. 74.1 ). Clinically, increased filling pressure leads to dyspnea, and reduced stroke volume leads to tachycardia—and ultimately to reduced cardiac output and systemic hypotension. In dehydrated patients, effusions of relatively smaller volume causing less elevation of intrapericardial pressure can be hemodynamically significant (termed low-pressure tamponade ).
Clinical Presentation
Pericardial effusion is not infrequently first detected as an incidental finding in an asymptomatic patient. Effusion can be identified in a chest computed tomography or magnetic resonance imaging scan or in an echocardiogram (ECG) performed for another reason.
Clinical symptoms and signs associated with pericardial effusion depend on the pressure of the effusion on surrounding structures (e.g., lung, trachea, esophagus, nerves) and the degree to which ventricular filling pressure is increased and cardiac output is impaired.
A common symptom is dyspnea, which may result from multiple causes including elevated ventricular filling pressure and potentially compression of the lung, trachea, or bronchi. Fatigue is also a common symptom, resulting from reduced cardiac output. A decreased stroke volume typically leads to tachycardia (to maintain cardiac output), which in turn can lead to a sense of a “rapid heartbeat” or palpitations. Other less common symptoms include dysphagia resulting from esophageal compression, hiccups resulting from vagal or phrenic nerve involvement, and hoarseness resulting from recurrent laryngeal nerve involvement. Hemodynamic collapse secondary to cardiac tamponade is a still less common but potentially fatal presentation.
Tachycardia is the most common sign in tamponade. In addition, pulsus paradoxus, an exaggeration of the normal inspiratory decline in systolic blood pressure, is greater than 10 mm Hg in tamponade. Marked elevation of the jugular venous pulse is often present on examination of the neck veins but may be absent in the dehydrated patient. The lung fields are typically clear and heart sounds may be normal or diminished in intensity.
Diagnostic Evaluation
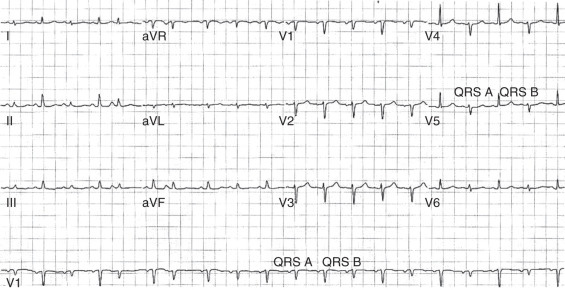
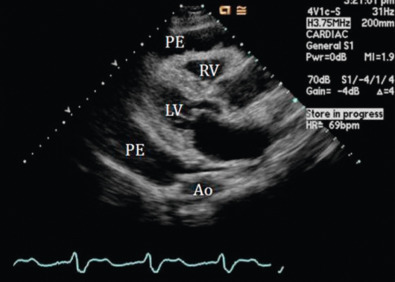
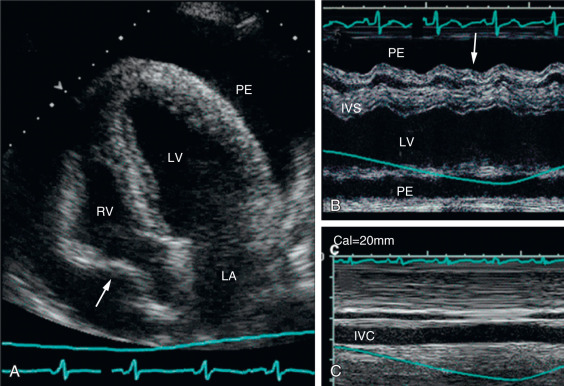
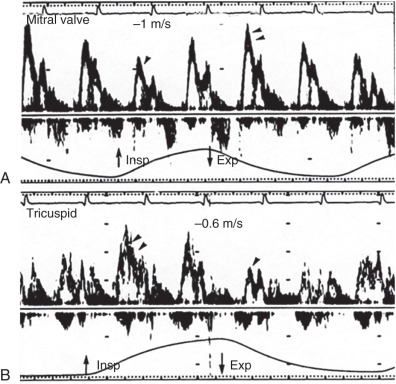
The chest x-ray may reveal a classic “water-bottle” enlargement of the heart with clear lung fields. The ECG is not specific but with very large effusions, and, particularly with tamponade, QRS complex amplitude is reduced and electrical alternans is an occasional finding ( Fig. 74.2 ). The echocardiogram ( Fig. 74.3 ) is useful in qualitatively defining the volume and hemodynamic significance of pericardial effusion even before tamponade is apparent clinically. Diastolic collapse of the right atrium and ventricle ( Fig. 74.4 ), marked and 180-degree out-of-phase respiratory variation in mitral and tricuspid diastolic inflow velocity (E velocity; Fig. 74.5 ), and dilatation of the inferior vena cava and absence of respiratory variation in its diameter are all echocardiographic features of actual or impending tamponade.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree