Infectious Mononucleosis and Mononucleosis-like Syndromes
Classic Infectious Mononucleosis
Definitions and Classifications
Terminology is a problem in infectious mononucleosis (IM) and related syndromes, and historical usage needs to be integrated with practical and meaningful definitions. Clinical IM was classified by Hoagland in 1960 as having pharyngeal (very common), typhoidal (fever only), and icteric forms. The last two forms are now readily recognized if Epstein-Barr virus (EBV) serology is done in patients with acute hepatitis and in febrile patients with atypical lymphocytes on blood smear. The classification used in this book is outlined in Table 3-1. Classic IM is defined as meeting all three criteria of clinical, hematologic, and serologic features.
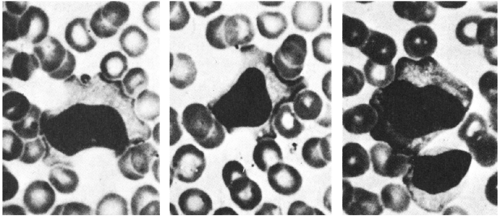
The clinical features of classic IM (or “mono”) typically include at least three of the following: exudative pharyngitis, generalized lymphadenopathy, splenomegaly, malar facial swelling, and easy fatigability. The hematologic feature is the presence in the peripheral blood smear of at least 5% atypical lymphocytes (Fig. 3-1). The serologic feature is a slide test positive for IM antibodies (agglutinins for sheep or horse erythrocytes). This book uses “heterophile antibody” to mean the current customary usage; namely, the sheep or horse erythrocyte-agglutinating antibody that is absorbed by guinea pig antigen but not by beef antigen. Perhaps Paul and Bunnell’s original speculation was correct that the agent of IM (EBV) has a cross-reacting antigen that usually stimulates humans (except many young children) to produce such a heterophile antibody.1
Primary EBV infection can now be demonstrated by antibody titers. However, “EBV infection” and “infectious mononucleosis” should not be used as synonyms: EBV infection often does not result in classic IM, and mono-like illness can have causes other than EBV infection. This distinction in terminology is analogous to distinguishing between mumps virus infection and parotitis. EBV is a possible etiology of many syndromes that are not like IM, as discussed in chapters on other syndromes. Heterophile-negative IM is discussed in the section on mono-like syndromes.
Clinical Diagnosis
Pharyngitis
Febrile exudative pharyngitis is the most frequent clinical picture of IM.2,3,4,5,6,7,8,9 It often is severe and may resemble the membranous pharyngitis of diphtheria. Concurrent Group A streptococcal pharyngitis is no more common than in normal controls.6 However, a throat culture to exclude concurrent streptococcal pharyngitis is reasonable in this situation, as the pharyngitis of Group A streptococcus and that of EBV infection are clinically indistinguishable. A certain number of streptococcal carriers will be falsely identified as having streptococcal pharyngitis when this approach is taken. Therefore, if the diagnosis of IM is clinically obvious the pharyngitis can be attributed to EBV infection, and the throat culture omitted. Petechiae on the hard palate are an occasional feature of both streptococcal and EBV pharyngitis.
Lymphadenopathy
Most patients with IM have generalized adenopathy. Enlargement of the anterior cervical (tonsillar) nodes is of little diagnostic value, since it may accompany tonsillitis from any cause. Posterior cervical adenopathy is much more suggestive of IM.5
Splenomegaly
Most patients with classic IM have splenomegaly, a sign that may make the physician suspect IM. Athletic teenagers often have well-developed
abdominal musculature that impairs palpation, but typically they have splenic enlargement by percussion.
abdominal musculature that impairs palpation, but typically they have splenic enlargement by percussion.
TABLE 3-1. LOGICAL COMBINATIONS OF THREE FEATURES OF INFECTIOUS MONONUCLEOSIS-LIKE SYNDROMES | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
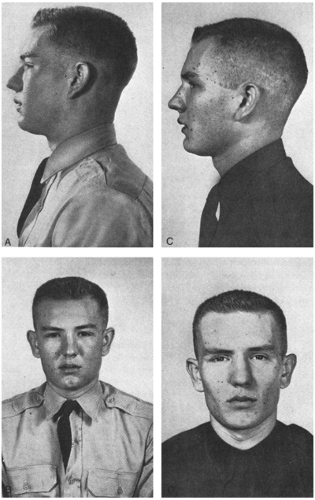
Edema around Eyes
Edema of the upper eyelid, and especially edema of the upper cheek just below the eye, is an extremely useful, if often overlooked, finding that is present in about one third of adolescents or young adults with IM (Figure 3-2).5 This feature was first described by Hoagland and is sometimes called “Hoagland’s sign.”
Jaundice
About 5% of young adults with IM have jaundice. In one series of children under 16, serum aminotransferase levels were elevated in about 40% during the acute illness.7 When unusually high alkaline phosphatase levels are found in nongrowing teenagers or young adults with minimal and disproportionately low bilirubin levels, IM should be suspected.8
Mild Abdominal Pain
The enlarged liver or spleen may produce mild upper abdominal pain and tenderness on palpation.
Rash
A maculopapular rash has been noted in about 10% of children3 but was noted in 40% of patients in one large series.9 If the patient has been given ampicillin (a poor choice for any pharyngitis), a rash occurs in 70–100% and usually is confluent and extensive and may be frightening. In bygone days, the appearance of a rash in patients with IM upon exposure to ampicillin was used as a diagnostic test. The rash may also occur in patients with IM due to cytomegalovirus (CMV) infection, as well as in patients with acute lymphocytic leukemia.10 Rash may also occur upon treatment with other antibiotics,
including amoxicillin and cephalexin.11 The mechanism by which antibiotic-associated rash is produced in patients with IM is not understood.
including amoxicillin and cephalexin.11 The mechanism by which antibiotic-associated rash is produced in patients with IM is not understood.
Easy Fatigability
Most children who are old enough to articulate this symptom will volunteer it or acknowledge it on questioning.
Laboratory Approach
Atypical Lymphocytosis
An increase in the number of lymphocytes with atypical forms is usually found in IM. Atypical lymphocytosis can be observed in association with many viral diseases (Box 3-1), some nonviral diseases (toxoplasmosis, babesiosis, malaria, tsutsugamushi scrub typhus),
poisoning, toxin exposure, radiation, malignancies, drug reactions, and allergies.4,12 Some authorities emphasize that the atypical lymphocytes of IM can often be distinguished from those of other diseases, but few laboratory technologists can make this distinction accurately. Thus, the finding of atypical lymphocytes is not specific, but it is useful to stimulate a search for more specific diagnostic information, especially if more than 10% of the lymphocytes are atypical. Some laboratories report a small percentage of atypical lymphocytes in many patients who do not have IM. This finding is usually of no significance. Patients with IM commonly also have a “shift” toward the lymphocyte lineage, in that greater than 50% of the white blood cells are lymphocytic. Experienced observers use many features of staining and morphology to recognize atypical lymphocytes. For the physician who does not examine smears often, the presence of denting or scalloping of lymphocytes by erythrocytes is a useful finding (Fig. 3-1). Dented cytoplasm is also seen in the atypical lymphocytes of the mono-like syndrome caused by cytomegalovirus.
poisoning, toxin exposure, radiation, malignancies, drug reactions, and allergies.4,12 Some authorities emphasize that the atypical lymphocytes of IM can often be distinguished from those of other diseases, but few laboratory technologists can make this distinction accurately. Thus, the finding of atypical lymphocytes is not specific, but it is useful to stimulate a search for more specific diagnostic information, especially if more than 10% of the lymphocytes are atypical. Some laboratories report a small percentage of atypical lymphocytes in many patients who do not have IM. This finding is usually of no significance. Patients with IM commonly also have a “shift” toward the lymphocyte lineage, in that greater than 50% of the white blood cells are lymphocytic. Experienced observers use many features of staining and morphology to recognize atypical lymphocytes. For the physician who does not examine smears often, the presence of denting or scalloping of lymphocytes by erythrocytes is a useful finding (Fig. 3-1). Dented cytoplasm is also seen in the atypical lymphocytes of the mono-like syndrome caused by cytomegalovirus.
BOX 3-1 Causes of Lymphocytosis
| Atypical lymphocytosis |
| Common Epstein-Barr virus Cytomegalovirus |
| Uncommon Hepatitis A virusa Respiratory syncytial virusa,15 HIV (Acute retroviral syndrome)b |
| Rare Toxoplasmosisa Babesiosisa Malariac Drug-hypersensitivity syndromes Toxin exposure Malignancies (especially non-Hodgkin’s lymphoma) |
| Typical lymphocytosis Pertussis Acute infectious lymphocytosis16 |
| aUsually does not cause an atypical lymphocytosis. bFrequently causes atypical lymphocytosis. cAlmost always associated with some degree of atypical lymphocytosis. |
Pertussis is classically associated with a lymphocytosis, but the lymphocytes are not atypical and the clinical presentation does not resemble IM (see Chapter 7). Rarely, other infections may be associated with extremely high white blood cell counts with a lymphocytic predominance. This pattern has been termed acute infectious lymphocytosis. Typically, the etiologic agent is not discovered. Cases attributable to viral13 and even parasitic14 infections have been described. Atypical lymphocytes are not observed. As the lymphocytosis resolves, a transient eosinophilia sometimes develops.
Serologic Diagnosis
The traditional serologic test for heterophile antibody is a tube dilution test using sheep erythrocytes as antigen, but cumbersome tube tests are no longer necessary. Several slide tests using horse or sheep erythrocytes are simple and rapid screening tests for the antibody and can easily be repeated in a week or so if the initial test is negative but the diagnosis is still suspected. When the person reading the test is experienced in the practice, slide screening tests (such as Monospot®), have a high degree of specificity for IM; that is, false-positive results are uncommon.17,18 A small percentage of normal individuals, however, will have persistently false-positive slide tests.
The principal limitation of these tests is their low sensitivity. A negative slide screening test in no way eliminates the diagnosis of IM. The negative predictive value of the slide test was found to be 82% in one recent study involving 299 children and adolescents with clinically and serologically defined IM.19 Another study showed that 271 (82%) of 329 patients with clinical IM who eventually had positive heterophile antibody tests required more than one sample before a positive result was obtained.20 Finally, in a small cohort, no correlation could be found between severity of disease and the percent positive by heterophile antibody testing.21 This implies that even patients who are very sick with EBV-induced IM may test falsely negative by heterophile antibody testing methods. Clinical practice backs up the experience reported in these studies; we have seen hospitalized patients with EBV-induced IM who had 2 or even 3 negative Monospot® tests. In these patients, the diagnosis can be made by testing for specific antibody production with EBV serology. Those with CMV-induced IM are also negative by heterophile antibody tests, so inclusion of CMV titers is often helpful in evaluation of patients with clinically suspect IM but negative slide screening tests.
Interpreting EBV serologic results is simpler if you use this seemingly silly but useful analogy and think of EBV as a peanut M&M. The candy coating is the viral capsid antigen (VCA). Since the candy is the first thing you taste when eating a peanut M&M, this reminds you that antibodies, both immunoglobulin M (IgM) and immunoglobulin G (IgG), to VCA are the first antibodies the immune system makes after EBV infection. The next layer is the chocolate, which represents EBV early antigen (EA). Antibody to EA, therefore, is made second. Finally, the peanut symbolizes the Epstein-Barr nuclear antigen (EBNA). Antibody to EBNA arises last. IgG antibody to VCA and antibody to EBNA persist for life, but antibody to early antigen wanes, usually within 6–9 months (Table 3-2). Stretching the analogy slightly further, remembering that chocolate melts makes it easy to recall that antibody to EA goes away over time.
Duration of Positivity
The most useful specific antibody for diagnosing primary EBV infection is the IgM EBV capsid antibody (Table 3-2). This appears within one month and becomes negative by three months in 80% of patients. As noted above, antibody to EA disappears within 9 months in most patients, but can persist for several years. There is no clinical significance to this phenomenon. The heterophile antibody test may remain positive in 75% of patients for up to one year.
TABLE 3-2. ANTIBODIES USUALLY INCLUDED IN AN EBV-ANTIBODY PANEL (EBV SEROLOGY), AND THEIR INTERPRETATION | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Age Frequency
A positive heterophile slide test occurs most frequently in the 10- to 29-year-old group.9,22 In one series of 575 cases of heterophile-positive IM in Georgia, less than 1% were 4 years of age or younger, only 5% were less than 10 years of age, and only 3% were 30 years of age or older.9 This is not to suggest, however, that EBV infection does not occur in young children, but rather that it may be harder to diagnose. It is not known why young children do not reliably produce heterophile antibodies in response to EBV infection. These patients can be diagnosed, however, by specific EBV serology. In the study cited above, all patients, including those less than 2 years of age, mounted a measurable serologic response to the viral capsid antigen, although Monospot® testing was often negative.
In summary, the majority of children less than 10 years of age who have EBV infections are asymptomatic or have illnesses that do not resemble classic IM.23,24 However, if a young child does appear to have classic IM, specific EBV antibody tests, in addition to a test for heterophile antibody, should be done. Some will be rapid slide test positive; one study showed that 35% of children ages 2 and 3
years were positive, versus 80% of children between the ages of 4 and 11 years.25
years were positive, versus 80% of children between the ages of 4 and 11 years.25
Contagion
Initial lytic replication of EBV probably takes place in mucosal epithelial cells of the oropharynx. From there the virus infects and then immortalizes B cells, in which it establishes latency. It has been shown to be periodically shed from the oropharynx. Several recent investigations suggest that replication in B cells must occasionally be lytic; using polymerase chain reaction (PCR), EBV DNA can be found in the serum of at least 20% of patients with EBV-induced IM.26,27 Studies have also identified not only EBV genome, but also replication-competent EBV particles in the urine of patients with IM,28 although there is no epidemiologic evidence supporting transmission of the virus through urine.
The spread of the disease by saliva was deduced by Hoagland as early as 1960 from West Point cadets.29 He noted lack of spread among roommates, and an incubation period of 5–7 weeks based on histories of brief episodes of intimate kissing. He also noted an incubation period of 21 days after blood transfusions.
Outbreaks have been reported, documented by EBV-specific serology.30 However, outbreaks reported on the basis of slide tests may well be pseudo-outbreaks related to improper performance and interpretation of the tests.31 Studies of families have indicated that about one-fourth of susceptible members will develop infection as evidenced by seroconversion, but that the younger children will usually not develop clinical disease.32 EBV has been recovered from the pharynx 9 days before onset of symptoms and can persist for as long as 6 months.32,33 It has also been shown that asymptomatic shedding of EBV in saliva can and does occur intermittently throughout life after EBV infection. At any point in time, between 6 and 20% of adults have measurable amounts of EBV in their saliva.34 Many factors, including stress and intercurrent illness, have been implicated in the periodic asymptomatic reactivation of EBV replication.
Treatment and Prevention
Rest is usually the only treatment necessary. Most patients have significant fatigue, so rest is not difficult to enforce. Corticosteroid therapy for 6–10 days has been advocated for severe cases, such as those with potential airway obstruction. Corticosteroids are effective in reducing fever and other symptoms,35 but it is doubtful that such potent therapy is justified for symptomatic relief in a self-limiting illness, and therapy may even prolong recovery.
In vitro, acyclovir inhibits lytic replication of EBV. Acyclovir given intravenously (10 mg/kg) every 8 hours for 7 days was statistically more effective than placebo, but only when six measures of improvement were combined.36 Liver enzymes were not improved in the treated group. Another study looked at using prednisolone and acyclovir in uncomplicated IM. Oropharyngeal EBV shedding was significantly decreased in the treatment group, but no effect was observed on duration of illness, sore throat, weight loss, or other symptomatic parameters.37 The lack of effect of acyclovir is intuitive, because the clinical manifestations of EBV infection are primarily due to the host immune response, not to viral replication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree