Infections Complicating Chronic Diseases
Certain chronic diseases of children are associated with a higher than expected frequency of infectious complications. Some of these patients are immunocompromised hosts (ICH) and their unusual infecting organisms are referred to as opportunistic pathogens, because the microorganism may be normal flora or may only rarely produce disease in healthy children. Other patients may have a normal immune system, but the presence of an anatomic abnormality predisposes them to particular infections. Often, a combination of these factors exists.
This chapter classifies infections by the abnormal organ system or the disease rather than by the infecting agent or the physiologic defect of the host (Table 22-1). Infections in transplant recipients are included here. The approach to the child with a possible but unknown immune deficiency is covered in Chapter 23, as is the management of the child with a known primary immune disorder. HIV infection is covered in Chapter 20.
Several other infections in children with chronic illness are discussed elsewhere in this book where it seems more logical. The problem of fever in patients with heart disease is discussed in the section on endocarditis in Chapter 18. Intravascular device infections are covered in Chapter 10, neurosurgical shunt infections in Chapter 9, and postoperative wound infections in Chapter 17.
Splenic Absence or Dysfunction
Individuals who are born without a spleen (congenital asplenia), who have been splenectomized for any reason, or whose splenic function is impaired by disease, such as sickle cell anemia, are at a significantly increased risk for fatal septicemia. In many cases, the infection is fulminating and is typically caused by encapsulated bacteria, usually Streptococcus pneumoniae or, less commonly, Haemophilus influenzae type b. In infants younger than 6 months with congenital asplenia, the organism is more likely to be an encapsulated strain of Klebsiella or E. coli.1 Other infections to which asplenic patients are especially susceptible include meningococcemia, malaria, babesiosis, and Capnocytophaga canimorsus infection, which is associated with dog bites.
Functions of the Spleen
The frequency of encapsulated organisms in bacteremia in the asplenic patient provides strong evidence that the spleen aids in phagocytosis, both by the filtering effect of macrophages and production of specific Ig (immunoglobulin) M antibodies to opsonize bacteria.2 Heavily encapsulated bacteria, such as the pneumococcus, are poorly opsonized by complement. The patient without capsular-specific antibodies from prior infection or from immunization relies on splenic macrophages to recognize and remove the bacteria before overwhelming sepsis ensues. The importance of the spleen is much greater during the first 2 years of life, possibly because other organs can later take over part of its function. Other protective roles of the spleen include synthesis of tuftsin (a stimulator of phagocytes), production of a platelet humoral factor and possibly production of other humoral factors related to immunity, and clearance of intraerythrocytic parasites, such as that of malaria. The spleen is believed to be necessary for normal thymic maturation during the neonatal period and to be involved in B-cell and T-cell interactions.
Howell-Jolly Bodies
These are very small, round, dark blue inclusions within red blood cells and are made up of nuclear debris. The spleen usually removes red cells containing these inclusions, and thus their presence is suggestive of hyposplenism. If the possibility of asplenia is suspected, a manual review of the
peripheral smear should be requested. Howell-Jolly bodies may be found in the peripheral smear in normal neonates, but are uncommon later in life. Interference phase-contrast microscopy can be used to detect red cells that are “pocked,” which has slightly greater sensitivity3 and specificity4 for asplenia than does the presence of Howell-Jolly bodies.
peripheral smear should be requested. Howell-Jolly bodies may be found in the peripheral smear in normal neonates, but are uncommon later in life. Interference phase-contrast microscopy can be used to detect red cells that are “pocked,” which has slightly greater sensitivity3 and specificity4 for asplenia than does the presence of Howell-Jolly bodies.
TABLE 22-1. CONTENTS OF THIS CHAPTER | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
If Howell-Jolly bodies are discovered incidentally, a history should be obtained, both regarding previous episodes of sepsis as well as the looking for causes of asplenia and hyposplenia. An abdominal ultrasound should be performed, looking for the spleen. If the spleen is present, a technicium-99m liver-spleen scan should be performed. If there is no uptake of the radioactive tracer by the spleen, a diagnosis of functional hyposplenism can be made.5
Clinical Manifestations
Overwhelming postsplenectomy infection often begins with a nonspecific influenza-like prodrome with fever, chills, malaise, myalgia, and headache. In addition, gastrointestinal symptoms such as vomiting, diarrhea, and abdominal pain may be prominent, distracting the physician from the diagnosis and resulting in delayed treatment.6 The prodrome, which may last a few days or only a few hours, is followed by rapid progression to septic shock, with hypotension and disseminated intravascular coagulation. Symmetric peripheral gangrene may result. The mortality is greater than 50%. In contrast, if bacteremia is recognized and treated prior to the development of clinical sepsis, the mortality rate is less than 10%.5
Specific Conditions
Congenital Asplenia
This may occur as an isolated finding but is most commonly associated with complex congenital cardiac defects, especially atrioventricular canal, transposition of the great arteries, pulmonary stenosis or atresia, and total anomalous pulmonary venous return. Children with these defects should have an abdominal ultrasound looking for the presence of a spleen. After the first month of life, such children are at greater risk of dying of sepsis than from their cardiac defect; thus, antibacterial prophylaxis is warranted.1 Some of these children have accessory splenic tissue in the peritoneal cavity (polysplenia). However, the degree of protection offered by accessory spleens is variable, and antibacterial prophylaxis is probably warranted.5 Heterotaxy syndromes are usually associated with asplenia or polysplenia. In addition to cardiac defects, patients may have primary ciliary dyskinesis, biliary atresia, intestinal malrotation, and multiple other anomalies.7,8
Postsplenectomy
Removal of the spleen may be necessary because of splenic trauma, malignancy, or hypersplenism (such as occurs in immune thrombocytopenic purpura). Children are at a higher risk of postsplenectomy sepsis than adults, and the risk is greater
in persons undergoing splenectomy because of malignancy or thalassemia than for trauma.9 This may be because of the frequent presence of splenic implants (splenosis) in patients who undergo splenectomy for trauma, which is sometimes (but not predictably) protective.10
in persons undergoing splenectomy because of malignancy or thalassemia than for trauma.9 This may be because of the frequent presence of splenic implants (splenosis) in patients who undergo splenectomy for trauma, which is sometimes (but not predictably) protective.10
The highest risk for infection is during the first 2 years after splenectomy. However, a third of infections occur up to 5 years later, and cases of fulminant infection have been reported more than 20 years postsplenectomy. The increased risk of dying of serious infection, although not quantifiable, is clinically significant and almost certainly lifelong.11
Functional Asplenism
In addition to the hemoglobinopathies, splenic dysfunction has been linked to a variety of conditions, including celiac disease, ulcerative colitis, portal hypertension, systemic lupus erythematosus, Graves’ disease, polyarteritis nodosa, sarcoidosis, and HIV infection.5 An important category of patients with functional hyposplenism are those who have received splenic irradiation for cancer or those who have undergone a stem cell transplant and develop graft-versus-host disease.12,13
Sickle Cell Anemia
Due to autoinfarction of the spleen, children with sickle cell anemia are at substantially increased risk for sepsis. In the first 5 years of life, the risk for pneumococcal sepsis is approximately 400 times that of the general population.14 Patients with other hemoglobinopathies, such as sickle-C disease, are at intermediate risk.15 The greatest risk is in young children with high fever and elevated white blood cell (WBC) count.16 However, some children will present in a more subtle fashion. Bacteremia should be considered in all children with sickle cell anemia and fever (T greater than 38°C) especially in the first 5 years of life. In such children, blood cultures should be obtained and empiric treatment with ceftriaxone given. Children at higher risk (less than 2 years old, temperature greater than 40°C, WBC less than 5000/mcL or greater than 30,000/mcL, those who are ill-appearing or have pulmonary infiltrates or another focus of infection) should be admitted to the hospital for intravenous antibiotics. Well-appearing children at lower risk are often treated as outpatients, with careful follow-up and a second dose of ceftriaxone intramuscularly until the initial culture is negative at 48 hours.17
In addition to sepsis with encapsulated bacteria, patients with sickle cell anemia are also at risk for other infectious complications. As described in Chapter 11, infection with parvovirus B19, the agent of erythema infectiosum, can precipitate severe hypoplastic crisis in patients with sickle cell disease. The increased risk of osteomyelitis (especially due to Salmonella spp.), and the difficulty in distinguishing this condition from the more common bone infarction, is discussed in Chapter 16.
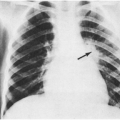
The acute chest syndrome is the leading cause of death among patients with sickle cell disease. It can be defined as a new pulmonary infiltrate involving at least one complete lung segment and one or more of the following findings: temperature greater than 38.5°C (seen in 80% of patients), cough (62%), chest pain (44%), or wheezing (26%).18 The lower lobes are typically involved, and effusions develop in about half of cases. Acute chest syndrome is most commonly caused by infection; infarction and fat embolism are also frequent causes. In a prospective multicenter study of 671 episodes among 538 patients (all of whom underwent bronchoalveolar lavage), an infectious cause was found in 249 (37%).18 Of the 249 episodes triggered by infection, Chlamydia pneumoniae was the most frequently identified organism, found in 71 (29%). Other frequent causes were Mycoplasma pneumoniae (20%), respiratory syncytial virus (10%), and Staphylococcus aureus, S. pneumoniae, Mycoplasma hominis, and parvovirus (4% each). Eighteen (3%) of the 528 patients died, and infection was a factor in 10 deaths. S. pneumoniae, E. coli, H. influenzae, legionella, cytomegalovirus, S. aureus, and chlamydia were implicated in fatal cases. Appropriate management of the acute chest syndrome includes a third-generation cephalosporin and a macrolide, as well as oxygen, bronchodilator therapy, and often, red cell transfusion.
Prevention
Effective prevention of invasive disease in patients with an absent or dysfunctional spleen requires a three-pronged approach of education, vaccination, and prophylactic antibiotics.5
Education
In one survey, of 63 patients who had undergone a splenectomy in the previous few years, only 10 (16%) were aware of any health precautions.19 Asplenic patients should be aware of the need to notify
their physician or seek immediate medical care in the event of any acute febrile illness. Patients should be encouraged to wear a Medi-Alert bracelet indicating their asplenic status.11 They should be counseled regarding the risk of C. canimorsus sepsis after dog bites.
their physician or seek immediate medical care in the event of any acute febrile illness. Patients should be encouraged to wear a Medi-Alert bracelet indicating their asplenic status.11 They should be counseled regarding the risk of C. canimorsus sepsis after dog bites.
Expert travel advice is especially important. Travel to areas where malaria is endemic should be discouraged.11 If travel to such areas is necessary, patients should be made aware of their increased risk of severe falciparum malaria and the need for strict adherence to effective antimalarial prophylaxis as well as protective measures, such as the use of DEET-containing insect repellent and mosquito netting. Patients traveling to sub-Saharan Africa should receive quadrivalent meningococcal vaccine if they have not already done so.
Pneumococcal Vaccination
Patients with an absent or dysfunctional spleen should definitely be vaccinated against S. pneumoniae. Unfortunately, 30–60% of eligible patients never receive the pneumococcal vaccine.19,20 In the case of elective splenectomy, the vaccine should be given at least 2 weeks before surgery since asplenic individuals have impaired antibody production.
The recent introduction of the seven-valent conjugated pneumococcal vaccine (PCV7) represents a significant advance in the prevention of invasive pneumococcal disease. In contrast to the 23-valent polysaccharide pneumococcal vaccine (PPV23), the conjugate vaccine is immunogenic in young infants and induces immunologic memory both in healthy children21 and in children with sickle cell diesase.22 Children should receive the primary series of PCV7 as described in Table 22-2. Children 2 years old or more who have been primed with PCV7 have a significant booster response to PPV23.21,22 Thus, in order to receive protection against the additional serotypes contained in the 23-valent vaccine, high-risk children who have received PCV7 should also receive PPV23, according to the schedule in Table 22-3.
TABLE 22-2. RECOMMENDED SCHEDULE FOR USE OF 7-VALENT PNEUMOCOCCAL CONJUGATE VACCINE (PCV7) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Children at high risk for invasive pneumococcal disease who have already received PPV23 (but who have not received PCV7) should receive 2 doses of PCV7, 2 months apart. Although the vaccine is only FDA approved for children up to age 9 years, it has been shown to be immunogenic in persons aged 4–30 years with sickle cell disease,23 and administering PCV7 to older children with high-risk conditions is not contraindicated.24
In children with functional or anatomic asplenia, the parents and patients should understand the risk of fulminant pneumococcal disease and that vaccination does not guarantee protection.25 Prompt medical attention is required for febrile illnesses. Immediate expectant antimicrobial treatment should be given for suspected bacteremia, the initial signs and symptoms of which may be subtle.
H. influenzae Type b Vaccine
Children with an absent or dysfunctional spleen should have their immunization history reviewed. Most children in the United States will have received
conjugate H. influenzae type b vaccination. Children who have not completed the primary series and booster at 12–15 months of age should be vaccinated. Asplenic children older than 5 years who have not previously been vaccinated should receive 2 doses, 2 months apart.26 The vaccine has been shown to be immunogenic in children with sickle cell disease.27
conjugate H. influenzae type b vaccination. Children who have not completed the primary series and booster at 12–15 months of age should be vaccinated. Asplenic children older than 5 years who have not previously been vaccinated should receive 2 doses, 2 months apart.26 The vaccine has been shown to be immunogenic in children with sickle cell disease.27
TABLE 22-3. SCHEDULE FOR VACCINATION USING 23-VALENT POLYSACCHARIDE VACCINE (PPV23) FOR CHILDREN AGED 2 YEARS OR MORE WHO HAVE PREVIOUSLY RECEIVED THE 7-VALENT CONJUGATE VACCINE (PCV7) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
N. meningitidis Vaccine
Quadrivalent meningococcal vaccine contains purified polysaccharides of serogroups A, C, Y, and W135 and is poorly immunogenic in young children. No vaccine is available for the prevention of serogroup B disease. Meningococcal vaccine should be given to all children with functional or anatomic asplenia at 2 years of age or older. The need for additional doses is unclear, but reimmunization does not elicit a booster response to serogroup C.28 A meningococcal group C conjugate vaccine was introduced into routine use for infant immunization in the United Kingdom in 1999, but is not currently available in the United States.29
Influenza Vaccine
Influenza vaccination is effective in reducing the risk of secondary bacterial infection thus, children with hyposplenia and their household contacts should receive annual influenza immunization.30 Despite this recommendation, immunization rates in such high-risk patients younger than 65 years are typically low (30–40%).31 Influenza vaccine has been shown to be reasonably immunogenic in preschool and school-aged children with sickle cell disease.32
Prophylactic Antibiotics
Daily oral penicillin has been shown to decrease the risk of serious bacterial infection by 84% in young children with sickle cell disease.33 Prophylaxis should begin as soon as the child is found to have sickle cell disease and preferably by 2 months of age. Most experts recommend penicillin V 125 mg b.i.d. for children younger than 5 years and 250 mg b.i.d. for those aged 5 years or older (alternatively, amoxicillin 20 mg/kg daily may be given). For the penicillin-allergic child, options are limited. Trimethoprim-sulfamethoxazole or erythromycin may be given, but the rates of pneumococcal resistance to these organisms are higher than to the penicillins.
Penicillin prophylaxis generally results in an overall decrease in the nasopharyngeal carriage rate of S. pneumoniae.34 An increase in the proportion of penicillin-resistant pneumococci colonizing the nasopharynx of children taking penicillin prophylaxis has been reported in some studies34,35 but not in others.36,37 Despite the concern about increasing resistance rates, penicillin’s safety profile, low cost, and lack of a suitable alternative oral agent argues for its continued status as the prophylactic drug of choice.
The optimal duration of therapy is not known. A multicenter study compared continuing penicillin prophylaxis with placebo after the age of 5 years in 400 children with sickle cell anemia.38 Four (2%) of placebo recipients developed systemic infection
with S. pneumoniae as compared with 2 (1%) of those receiving penicillin prophylaxis, a result that was not statistically significant. The authors concluded that children with sickle cell anemia who have not had a prior severe pneumococcal infection or a splenectomy and are receiving comprehensive care may safely stop prophylactic penicillin at 5 years of age. However, the confidence limits around their estimates were wide, and it is possible that a larger trial would have demonstrated a statistically significant result. Many experts continue penicillin prophylaxis indefinitely.
with S. pneumoniae as compared with 2 (1%) of those receiving penicillin prophylaxis, a result that was not statistically significant. The authors concluded that children with sickle cell anemia who have not had a prior severe pneumococcal infection or a splenectomy and are receiving comprehensive care may safely stop prophylactic penicillin at 5 years of age. However, the confidence limits around their estimates were wide, and it is possible that a larger trial would have demonstrated a statistically significant result. Many experts continue penicillin prophylaxis indefinitely.
The duration of prophylaxis in persons with anatomic or functional asplenia of another cause has not been studied. The Red Book states only that prophylaxis be strongly considered for all asplenic children younger than 5 years of age and for at least 1 year after splenectomy (in patients of any age).39 However, a British working group stated that lifelong prophylaxis should be offered in all cases. They especially recommend prophylaxis in patients who meet any of the following criteria: patients in the first two years after splenectomy, patients younger than 16 years old, and patients who have underlying impaired immune function.
Whether the asplenic patient is on prophylactic antibiotics or not, patients and parents need to be made aware of the importance of seeking prompt medical care if the patient develops a fever. This is preferable to self-administration of antibiotics when patients develop fever, although this may be considered in unusual circumstances when the patient does not have quick access to a hospital or clinic.
Collagen Disease
Children with chronic collagen diseases often have fever or complications that are not infectious. Sometimes, corticosteroids or other immunosuppressive drugs are used, resulting in the same kinds of opportunistic infections found in children with transplants.
Systemic Lupus Erythematosus
Infection is a leading cause of morbidity and mortality in systemic lupus erythematosus (SLE).40 In a prospective study of 200 patients with SLE, 65 (32%) developed infection over a 2-year period.41 Disease activity was the only variable independently associated with infection.
Most patients with SLE do not have specific complement defects. However, the diagnosis of SLE in a young male patient should alert the clinician to the possibility of complement deficiency (especially C1q, C2, and C4),42 with the consequent predisposition to severe infection with encapsulated bacteria (Chapter 23).43,44 Some patients with SLE have a mutation in the gene for mannose-binding lectin, which is associated with both higher disease activity and increased risk of infection.45
In a review of 63 hospitalized adults with SLE and fever, about 60% of the fevers were caused by the disease itself and about 23% were caused by infections.46 Shaking chills, leukocytosis, neutrophilia, and normal levels of anti-DNA antibodies were observed more frequently in infectious episodes, whereas leukopenia was more likely to indicate a noninfectious process. Some studies report that an elevated C-reactive protein in a febrile patient with SLE is suggestive of infection,47,48 whereas other studies show it to be of poor predictive value.49,50
Granulocyte colony stimulating factor has been used to increase neutrophil counts in patients with SLE-associated neutropenia. Unfortunately, in one study 3 (33%) of 9 patients experienced serious adverse effects (exacerbation of CNS [central nervous system] symptoms in two and leukocytoclastic vasculitis in one).51
Juvenile Rheumatoid Arthritis (JRA)
Sometimes, septic arthritis occurs in adults with rheumatoid arthritis, but it is extremely rare in children. Platelet dysfunction, renal papillary necrosis, and, rarely, Reye syndrome may be related to aspirin therapy. Pericarditis and myocarditis occur, but are usually not of infectious origin.
Hemophagocytic lymphohistiocytosis (HLH), also referred to as hemophagocytic syndrome or macrophage activation syndrome,52,53 is a rare but potentially lethal complication of systemic onset JRA. Although HLH is not an infectious process per se, it appears that certain infectious agents (e.g., Epstein-Barr virus) may trigger it in susceptible hosts.54 In children with JRA, the presentation is dramatic, with acute onset of fever, lymphadenopathy, and hepatosplenomegaly.53 One or more cell lines are depressed, liver enzymes are elevated, and clotting abnormalities may occur. The ferritin level is usually extremely high, and the ESR (erythrocyte sedimentation rate) is often unexpectedly low. The diagnosis is made by bone marrow examination, which demonstrates phagocytosis of various cells by macrophages. Initial treatment is with high dose
corticosteroids, but some patients do not respond. Consultation with a pediatric rheumatologist or hematologist is critical.
corticosteroids, but some patients do not respond. Consultation with a pediatric rheumatologist or hematologist is critical.
Mixed Connective Tissue Disease (MCTD)
This disease resembles a mixture of SLE, systemic sclerosis, rheumatoid arthritis, and dermatomyositis, and produces a high titer of speckled antinuclear antibody. An immune response to ribonuclear protein (RNP) is the defining serologic feature of MCTD.55 The disease often presents with Raynaud’s phenomenon, followed by fever and arthralgia.56 Lymphadenopathy and parotid gland enlargement also can give it the appearance of an infectious disease. Patients may have hypergammaglobulinemia and a positive rheumatoid factor.56 Severe thrombocytopenia can occur, and fatal meningococcemia has been reported.57
In a review of 224 children reported in the literature over a 25-year period, common long-term problems included loss of joint function, restrictive lung disease, scleroderma-like skin changes, renal involvement, and esophageal dysmotility. Cardiovascular problems included cardiomyopathy, myopericarditis, and pulmonary hypertension. Seventeen (8%) of the 224 patients died. Infection (usually sepsis) was the most common cause of death and was implicated in seven patients.58
Reye Syndrome
Cystic Fibrosis
Cystic fibrosis is common, affecting approximately 30,000 persons in the United States. Mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene result in defective chloride transport in the epithelial cells of the respiratory, hepatobiliary, gastrointestinal, and reproductive tracts, as well as the pancreas.60 Multiple different mutations have been identified, and severity of the disease varies greatly among patients.61 The primary causes of morbidity and mortality are airway inflammation, bronchiectasis, and obstructive pulmonary disease, which occur as a direct result of persistent endobronchial bacterial infection.
Pathogenesis and Microbiology
In the lung, decreased transport of chloride, sodium, and water results in dehydrated, viscous secretions that cause airway obstruction and create a favorable environment for persistent bacterial colonization. Initially, the airways are colonized with S. aureus, and non-typable H. influenzae. However, by the end of the first decade, Pseudomonas aeruginosa gradually becomes the predominant pathogen. During the transition from intermittent infection to permanent colonization, P. aeruginosa transforms from a motile, nonmucoid phenotype to a nonmotile, highly mucoid phenotype.62 The mucoid P. aeruginosa forms a biofilm that makes it highly resistant to antibiotics. This chronic bacterial endobronchitis is associated with an intense neutrophilic inflammatory response that damages the airway and impairs local host-defense mechanisms. Other bacteria sometimes causing pulmonary infections in patients with cystic fibrosis include Burkholderia cepacia, Serratia marcescens, and Stenotrophomonas maltophilia. Fungi (especially Aspergillus spp.) and non-tuberculous mycobacteria also can contribute to disease.63,64
Clinical Manifestations and Therapy
Intermittent exacerbations of chronic lung infection are frequent in patients with cystic fibrosis. Such exacerbations are usually heralded by increased cough and sputum production. Physical examination may show an increased respiratory rate and new or increased crackles or wheezes. Chest radiography will often show a new or progressive infiltrate, and spirometry will demonstrate a decline in pulmonary function. Chronic sinusitis (with or without nasal polyposis) is common in children with cystic fibrosis and may require endoscopic sinus surgery in addition to antibiotics.65
The therapy of exacerbations should be based on the results of sputum culture and sensitivity. Although a relatively insensitive predictor of lower airway pathogens, throat culture testing is often used for children too young to produce sputum. Combination intravenous therapy with an antipseudomonal beta-lactam agent (such as ceftazidime or cefepime) and an aminoglycoside is usually
given for approximately 14 days. For milder exacerbations, an oral fluoroquinolone, such as ciprofloxacin, is sometimes given. Although not approved for use in children, fluoroquinolones are generally well-tolerated in children with cystic fibrosis,66 and the benefits of their use appear to outweigh the risks in this population.67 An inhaled antibiotic, such as tobramycin or colistin may also be used; however, they have not been studied in the setting of acute exacerbations.68 Recombinant human DNase can be given by inhalation to reduce the viscosity of the sputum69 and some variation of chest physiotherapy is performed to enhance clearance of pulmonary secretions.70 This aggressive approach to pulmonary exacerbations is believed to be a major reason for the increased life expectancy among patients with cystic fibrosis during the past few decades.
given for approximately 14 days. For milder exacerbations, an oral fluoroquinolone, such as ciprofloxacin, is sometimes given. Although not approved for use in children, fluoroquinolones are generally well-tolerated in children with cystic fibrosis,66 and the benefits of their use appear to outweigh the risks in this population.67 An inhaled antibiotic, such as tobramycin or colistin may also be used; however, they have not been studied in the setting of acute exacerbations.68 Recombinant human DNase can be given by inhalation to reduce the viscosity of the sputum69 and some variation of chest physiotherapy is performed to enhance clearance of pulmonary secretions.70 This aggressive approach to pulmonary exacerbations is believed to be a major reason for the increased life expectancy among patients with cystic fibrosis during the past few decades.
Chronic antibiotic therapy to prevent pulmonary exacerbations is controversial but should probably be avoided. A multicenter study of 119 children with newly diagnosed cystic fibrosis was conducted to determine if continuous therapy with cephalexin was superior to placebo. After 7 years, there were no significant differences between the two groups in pulmonary function, frequency of exacerbations, nutritional status, or chest radiography scores. Although children in the cephalexin group were less likely to be colonized with S. aureus, they were twice as likely to be colonized with P. aeruginosa.71 A retrospective study of 639 German children with cystic fibrosis also showed an increased risk of colonization with P. aeruginosa among those who had received antistaphylococcal prophylaxis.72
Intermittent inhaled tobramycin was recently studied in a placebo-controlled trial.73 A total of 520 patients were randomly assigned to receive either 300 mg of inhaled tobramycin or placebo twice daily for 4 weeks, followed by 4 weeks with no study drug. Patients received treatment or placebo in three on-off cycles for a total of 24 weeks. At the end of the study period, patients receiving tobramycin had improved pulmonary function, decreased density of colonization with P. aeruginosa, and a 26% lower rate of hospitalization for pulmonary exacerbation. The drug was well tolerated. However, several important questions remain. The drug is expensive, and it is possible that once-daily administration would be as effective. In addition, whether long-term intermittent use will increase the development of drug-resistant strains of P. aeruginosa is unknown. Because of this concern, some centers reserve its use for exacerbations, when one or more systemic antibiotics are given simultaneously.
Viral infections are a common predisposing factor for exacerbations of cystic fibrosis. Patients and their household contacts should receive the influenza vaccine yearly. Although S. pneumoniae is not a common cause of infection in patients with cystic fibrosis, it is reasonable to administer the pneumococcal vaccine as well.
Allergic Bronchopulmonary Aspergillosis (ABPA)
This condition is a hypersensitivity lung disease caused by bronchial colonization with Aspergillus fumigatus. The presence of colonization with A. fumigatus in patients with cystic fibrosis can be has high as 50%;74 however, less than 10% of patients develop ABPA.75,76 Standard diagnostic criteria were recently proposed by a consensus group.76 They require the presence of two of three major criteria (immediate skin test reactivity to A. fumigatus, precipitating antibodies to A. fumigatus, and total serum IgE greater than 1,000 IU/mL), and two of six minor criteria (A. fumigatus in sputum, bronchoconstriction, peripheral eosinophil count more than 1,000/mcL, pulmonary infiltrates, elevated serum IgE or IgG to A. fumigatus, and response to corticosteroids).
If untreated, irreversible bronchiectasis may result. Conventional therapy has consisted mainly of systemic corticosteroids that, although effective, have numerous side-effects (such as growth failure, diabetes mellitus, and osteoporosis). Although randomized trials are lacking, anecdotal reports suggest that itraconazole treatment is associated with fewer episodes of ABPA and allows for decreased steroid use.77 Aerosolized amphotericin B has also been used in this setting, but no data are available regarding its effectiveness.
Nontuberculous Mycobacteria
These organisms (especially M. avium complex and M. chelonae) are isolated from sputum cultures in 3–30% of patients with cystic fibrosis.64 A pathogenic role has not been established, but some patients appear to improve clinically after a course of antimycobacterial therapy. Such therapy should be considered for the patient with repeatedly positive
sputum cultures, persistent symptoms, and declining pulmonary function despite routine antibacterial—and in some cases, antifungal—treatment.
sputum cultures, persistent symptoms, and declining pulmonary function despite routine antibacterial—and in some cases, antifungal—treatment.
Extrapulmonary Manifestations
As expected from the pathophysiology, multiple other organ systems are involved in cystic fibrosis. Pancreatic exocrine deficiency occurs in about 80% of patients, diabetes mellitus in up to 20%, and obstructive biliary tract disease in 15–20% of patients.60 Recurrent arthritis occurs in some patients, occasionally accompanied by erythema nodosum.78
Outcome
The median life expectancy is now greater than 30 years, and it is projected that for newborn infants it will become more than 40 years.61 Lung transplantation is an option for some patients to further increase survival but is limited by the availability of donor organs. The 5-year survival rate for lung transplant recipients with cystic fibrosis is about 50%.79 Gene transfer therapy for cystic fibrosis is currently under investigation, but multiple hurdles to its successful implementation still remain.80
Down Syndrome
Children with Down syndrome have well-documented immunological alterations, including a lower number of B cells, lower numbers of IgG2 and IgG4 subclasses, inverted CD4/CD8 ratio, and decreased T-cell proliferative responses to mitogens.81,82 Although not well studied, it is apparent that children with Down syndrome have an increased incidence of viral and bacterial respiratory infections, especially pneumonia and otitis media. In one series of 100 children with Down syndrome who underwent surgical correction of their heart defects, 38% had postoperative pneumonia.83
Part of the predisposition to infections relates to anatomic abnormalities, such as pulmonary hypoplasia and collapsed eustachian tubes.84,85 Children with Down syndrome also frequently have stenotic ear canals, leading to difficulty visualizing the tympanic membrane and underdiagnosis and undertreatment of otitis media.86 When these children undergo frequent ear examinations by an otolaryngologist, as many as 80% will be found to have chronic otitis media.85 Although hearing loss in children with Down syndrome is common, recent studies suggest that it is largely preventable with early and aggressive management of chronic otitis media.85 Most children with Down syndrome will require placement of tympanostomy tubes in the first 2 years of life.
Endocrine Disease
Diabetes Mellitus
In patients with diabetes, acute infections lead to difficulty in controlling blood glucose levels and are the most common precipitant of ketoacidosis.87,88 Adult patients with diabetes have an increased susceptibility to certain infections,89 but whether this is true for children with diabetes is less clear. Adult diabetic patients have an increased frequency of candidiasis (especially vaginal), staphylococcal infections (especially boils), infected decubitus ulcers, rhinocerebral mucormycosis, and malignant otitis externa.89 These infections rarely occur in children with diabetes.
Neutrophils from patients with diabetes demonstrate decreased chemotaxis, phagocytosis, and killing,87 and this decreased neutrophil function is more pronounced in patients whose diabetes is poorly controlled.88 In addition, some organisms (such as Candida albicans and E. coli) are more virulent in a high-glucose environment.87
Polyendocrinopathies
Autoimmune polyendocrinopathy syndrome (APS) type 1 (also referred to as autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy or APECED) is an autosomal recessive disorder characterized by chronic mucocutaneous candidiasis, hypoparathyroidism, Addison’s disease and sometimes other features such as insulin-dependent diabetes mellitus (IDDM).90,91 Some patients have severe cell-mediated immune dysfunction, whereas others have few problems with infections. Symptoms usually begin in childhood. It is discussed in more detail in Chapter 23. APS type 2 is an association of Addison’s disease with autoimmune thyroid disease, IDDM, or both.
A rare X-linked syndrome called IPEX (immunodysregulation, polyendocrinopathy, enteropathy, X-linked) has recently been elucidated.92 Boys present early in life with variable combinations of IDDM, diarrhea, eczema, anemia, thrombocytopenia, lymphadenopathy, and hypothyroidism.93 It is usually lethal in infancy or childhood. No specific immune abnormality has been detected, but patients
are at high risk for infections, and sepsis is a common cause of death. Some patients respond to chronic immune suppressive therapy, and a few patients have undergone successful bone marrow transplanation.92
are at high risk for infections, and sepsis is a common cause of death. Some patients respond to chronic immune suppressive therapy, and a few patients have undergone successful bone marrow transplanation.92
Heart Disease
Congenital Heart Disease
Children with congenital heart disease (CHD) are at increased risk for pneumonia, particularly if the defect is associated with chronic pulmonary congestion. Children with CHD have a rate of hospitalization for RSV infection that is three-fold to five-fold higher than age-matched controls.94 Once hospitalized, they more frequently require mechanical ventilation (20%) and have a higher mortality rate (3%) than children without heart disease.95 A recent multicenter study compared monthly palivizumab during RSV season with placebo in 1,287 children younger than 2 years of age with CHD.96 The intervention was safe and effective. Among placebo recipients, the rate of RSV hospitalization was 10%; the rate among children receiving palivizumab was 5%. Children with CHD most likely to benefit from palivizumab are those who are less than 12 months old94 and who have congestive heart failure, pulmonary hypertension, or cyanotic heart disease.
22q11.2 Deletion Syndrome (Velocardiofacial Syndrome)
Between 10% and 30% of children with various conotruncal cardiac anomalies will be found to have 22q11.2 deletion syndrome (velocardiofacial syndrome). The syndrome has previously been referred to as DiGeorge syndrome or Catch 22. In addition to the heart defect, patients usually have hypotonia, palatal anomalies, and mild developmental delay. Anomalies of other organ systems may occur as well, including thymic hypoplasia. These children frequently have impairment in T cell production and function,97 which tends to improve over time (Chapter 23).98 Children with impaired T cell function or with low CD4 counts (Chapter 20 for levels based on age) should receive trimethoprim-sulfamethoxazole (TMP-SMX) for PCP (Pneumocystis jiroveci) prophylaxis.
Fever in a patient with congenital or rheumatic heart disease is discussed in the section on endocarditis (Chapter 18). Infections in cardiac transplant recipients are discussed later in this chapter.
Kidney Disease
This section reviews the infectious complications of nephrotic syndrome, uremia, hemodialysis, and peritoneal dialysis.
Nephrotic Syndrome
Nephrotic syndrome is characterized by edema, hypoalbuminemia, proteinuria, and hyperlipidemia. Viral respiratory infections appear to be a common trigger for exacerbations of nephrosis.99 Children with nephrotic syndrome are at increased risk of infection for several reasons. Partly due to protein loss in the urine, they have decreased serum levels of immunoglobulins.100 They also have decreased serum complement concentration,101 impaired lymphocyte blastogenesis,102 and splenic hypofunction.103 In addition, patients with nephrotic syndrome are frequently on corticosteroids or other immunosuppressive agents.
Peritonitis
The classic infection in children with nephrotic syndrome is spontaneous bacterial peritonitis (SBP) caused by S. pneumoniae. However, other gram-positive organisms such as Enterococcus and viridans streptococci are occasionally seen, as are gram-negative organisms (especially E. coli).104,105 Sepsis in patients with peritonitis is not uncommon and is occasionally fatal.104 Patients with one episode of peritonitis are at increased risk for a second episode.
Children with SBP usually present with the acute onset of fever and abdominal pain, although occasionally the onset is subacute and the symptoms are subtle. Abdominal tenderness is apparent in an older child but may be difficult to discern in an infant. If SBP is suspected, cultures of blood and peritoneal fluid should be obtained. The peritoneal fluid usually contains more than 250 neutrophils per mcL. Empiric broad-spectrum antibiotics should be given to cover the pneumococcus and gram-negative organisms. The combination of vancomycin and a third- or fourth-generation cephalosporin is reasonable initial coverage. In the severely ill patient, an aminoglycoside should probably be added. Antibiotics are tailored to susceptibility testing and are given for 10–14 days.
Other Infections
In addition to peritonitis and sepsis, cellulitis is more common in children with nephrotic syndrome.106 During therapy with corticosteroids or other immunosuppressive agents, the child with nephrotic syndrome is at risk for many of the infections described in the sections on leukemia and transplantation.
Prevention
Children with nephrotic syndrome should receive pneumococcal vaccination (Tables 22-2 and 22-3). Whether prophylactic penicillin is of benefit is unclear. In one study, there was no increase in pneumococcal peritonitis for the 7 years after the policy of penicillin prophylaxis was discontinued.105 Consideration should be given to the use of TMP-SMX for PCP prophylaxis in children receiving prolonged courses (more than 14 days) of high-dose prednisone (more than 20 mg per day or more than 2 mg/kg per day).107,108
Uremia
Patients with uremia are at increased risk for infections, which are a common cause of death in this population.109 Such patients have impaired neutrophil function secondary to excessive parathyroid hormone and elevated intracellular calcium.110 Use of calcium-channel blockers has been shown to improve neutrophil phagocytosis in uremic patients.110 However, whether this translates into decreased incidence of infection is unknown. Other mechanisms such as iron overload contribute to the increased risk of infection in patients with chronic renal failure.111 As discussed in the next section, the use of dialysis brings additional infectious risk.
In addition to the routine childhood vaccines, children with chronic renal failure should receive pneumococcal vaccination (Table 22-3) as well as yearly influenza vaccination.112
Peritoneal Dialysis
Peritonitis
Peritonitis is a common complication of peritoneal dialysis. In two studies of children on peritoneal dialysis, the rate of peritonitis varied from one episode per 5.6 patient-months113 to one episode per 13.2 patient-months.114 Infection can occur with any contaminating organism, particularly S. aureus and S. epidermidis.115 If a nephrectomy has been performed, gram-negative enteric rods are more common.116 Fungi, particularly Candida albicans, are less common.
The diagnosis of peritonitis is usually suspected when the effluent is cloudy, a much more reliable finding than fever or peripheral leukocytosis.117 Abdominal pain is common but not universal. Routine screening cultures of the dialysate are not useful.117 The skin sites rarely look infected. In general, the diagnosis of peritonitis requires the presence of at least two of the following three criteria: (i) organisms on gram stain or culture of peritoneal dialysis fluid; (ii) cloudy fluid (more than 100 white cells per mcL with more than 50% neutrophils); and (iii) symptoms of peritoneal irritation.118 False-negative gram stains are common. In about 20% of cases, the culture is negative as well, particularly if there has been prior antimicrobial therapy.119 Optimally, 50–100 mL of effluent should be centrifuged and gram stained. The concentrate should then be injected into blood culture bottles.120
For patients without systemic toxicity, intraperitoneal administration of antibiotics is usually sufficient and can usually be accomplished as an outpatient. If the patient is toxic appearing, intravenous antibiotics are administered with the doses adjusted for renal failure. The International Society for Peritoneal Dialysis has published detailed guidelines for the treatment of peritonitis in children receiving peritoneal dialysis.121 Initial empiric therapy should usually be with intraperitoneal cefazolin and ceftazidime. For continuous antibiotic therapy, which is preferred, both are given as a loading dose of 250 mg of the antibiotic in the first liter of dialysate, followed by 125 mg of antibiotic in each subsequent liter of dialysate. The peritoneal dialysis exchange containing the loading dose should dwell in the abdomen for 4–6 hours. For intermittent therapy, both are dosed at 15 mg/kg in a single peritoneal dialysis exchange every 24 hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree