(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
The urinary bladder can be the site of primary malignant tumors requiring its resection. It also can be invaded by soft tissue sarcomas of the pelvis, adenocarcinomas of the rectum, or gynecologic malignancies that, when extensive, necessitate the en bloc resection of the entire bladder or the bulk of it. In such cases, reconstruction is needed in order to restore the function of the urinary tract.
A segment of ileum is usually selected about 10–15 cm from the ileocecal valve. From this point, the appropriate length of ileum (15–20 cm) is chosen such that the distal end of the segment will reach without tension the skin of the right lower quadrant of the abdomen midway between the umbilicus and the right anterior superior iliac spine, where the urostoma will be constructed. Because the dimensions of the abdominal cavity and the thickness of the abdominal wall vary considerably between patients, it is best to estimate the length of the ileal segment by a trial of placing the provisional ileal loop from the base of the lower descending mesocolon to the site of the abdominal wall, around the mobilized cecum, to determine whether the loop will go through to the designated site of the urostoma. An umbilical tape may also be used to measure the distance between the left ureteral stump, across the retroperitoneum, and around the cecum to the skin site of planned urostoma.
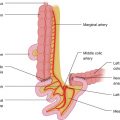
The cut ends of the right and left ureters should be exposed and mobilized sufficiently for their respective anastomoses to the planned ileal loop bladder. The exposure of the distal ureters renders more accurate the estimation of the length of the ileal loop that will be required for reconstruction. The bowel is divided proximally and distally at the designated points, taking into consideration the vascular arcade in the mesentery. In thin people, it is easy to see the mesenteric branches; in obese people, these branches can be delineated with the help of transillumination and palpation. It is critical to ascertain the excellence of blood supply to the two ends of the ileal loop as evidenced by pink color, bleeding at the edges, and pulsatile flow near the two ends. In the mesentery, branches from the superior mesenteric artery are vertically disposed toward the mesenteric border of the bowel and are connected to each other by arcades disposed in a parallel fashion to the mesenteric border of the bowel. At the proximal end of the loop, it is necessary to divide the mesentery only to a depth of about 5 cm, requiring the ligation and division of the most peripheral arcade at that point, as the proximal end of the bowel requires only enough mobility to be anastomosed anterior to the mesentery of the loop to the distal ileal end in restoring the continuity of the alimentary tract. The distal end of the ileal conduit needs greater mobilization so that it can come around the cecum and through the abdominal wall opening without tension. The distal end of the loop, therefore, before it is divided by stapling through it, is chosen to be over a corresponding mesentery with a wide distance between two adjacent vertical branches, allowing an incision deep in the mesentery with division of only the most peripheral arcade, if any.
The ends of the two ureters are then anastomosed to suitable openings made in the ileal loop close to the antimesenteric border. Interrupted sutures using a single layer of 4-0 or 5-0 polyglactin or other absorbable material are placed between the edge of the ureteral end and that of the ileal opening, with the knot on the outside. A suture is placed through the middle of the posterior edge of the ureteral and ileal openings, and an additional suture is similarly placed on each side of the posterior midline suture. The midline suture is tied first, followed by the two others on either side. The suturing is continued to the lateral corner on each side of the anastomosis. The stapled distal end of the ileal loop is opened, and a ureteral stent is placed through it and through the left ureteroileal anastomosis into the left ureter, up to the left renal pelvis. The anterior row of sutures is then placed, with each suture tagged with a mosquito clamp, one of the openings of its handles passing over a long clamp to maintain the order of placement of the sutures. The sutures are all placed close enough to achieve a watertight anastomosis. We have not seen any problems with close placement of sutures as long as the ureteral ends have good blood supply, achieved by avoiding dissection too close to their surface in the initial mobilization of the ureters.
The right ureteroileal anastomosis is made in a similar manner, again passing a stent through the anastomosis up the right ureter to the right renal pelvis. The distal opening of the ileal loop is then passed through the opening in the abdominal wall, the loop itself passing around the mobilized cecum. The opening in the abdominal wall should be wide enough for the end of the ileal loop to pass through comfortably. Seromuscular sutures with 3-0 silk are used to fasten the wall of the loop to the surrounding peritoneum at the deep side of the abdominal wall opening. Interrupted absorbable sutures are placed between the opening of the loop and the surrounding skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree