Hypersensitivity: Type IV
Introduction
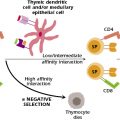
In contrast to antibody-mediated hypersensitivity reactions discussed in the previous two chapters, type IV hypersensitivity is T-cell mediated. In marked contrast with type I hypersensitivity mediated by IgE, which is immediately available to react with allergens, type IV responses involve the activation, proliferation, and mobilization of antigen-specific T cells. Thus, type IV hypersensitivity is delayed as compared with antibody-mediated hypersensitivity reactions, and it is often referred to as delayed-type hypersensitivity (DTH). Similar to the antibody-mediated hypersensitivity, DTH reactions can also result in damage to host cells and tissues. The harmful effects of DTH are initiated by the release of inappropriately large amounts of cytokines (including chemokines) by activated T cells. Chemokines attract and activate other mononuclear cells that are not antigen-specific, including monocytes and macrophages. The recruitment and activation of these antigen-nonspecific cells are mainly responsible for the eventual deleterious outcome of type IV hypersensitivity reactions.
DTH reactions are, therefore, cell-mediated immune responses. Depending on the antigen involved, they mediate beneficial (resistance to viruses, bacteria, fungi, and tumors) or harmful (allergic dermatitis, autoimmunity) aspects of immune function. Other antigens capable of eliciting DTH reactions include those expressed by foreign cells in transplantation settings or one of many chemicals (serving as haptens) capable of penetrating skin and coupling to body proteins that serve as carriers.
Cutaneous DTH reactions are initiated when CD4 memory T cells are activated by antigen-presenting cells in the skin (e.g., Langerhans cells). Upon activation, CD4+ T cells release inflammatory mediators that recruit effector cells to the site of antigen administration. While the monocyte/macrophage is thought to be the major effector cell in this model, CD8+ cytolytic T cells, and natural killer (NK) cells are also thought to serve as effector cells in DTH reactions. Activated effector cells mount an inflammatory response that results in the elimination of antigen and the extravasation of plasma accompanied by selling at the site of challenge. The magnitude of the response to the antigen is measured as an increase in swelling at the site of challenge (e.g., as seen during the development of a tuberculin skin reaction).
General Characteristics and Pathophysiology of DTH
The clinical features of type IV hypersensitivity reactions vary, depending on the sensitizing antigen and the route of antigen exposure. These variants include contact hypersensitivity, tuberculin-type hypersensitivity, and granulomatous hypersensitivity (see next section). In general, however, common pathophysiologic mechanisms account for each of these variants. The major events leading to these reactions involve the following three steps: (1) activation of antigen-specific inflammatory TH1 and TH17 cells in a previously sensitized individual; (2) elaboration of proinflammatory cytokines by the antigen-specific TH1 cells; and (3) recruitment and activation of antigen-nonspecific inflammatory leukocytes. These events typically occur over a period of several days (48–72 hours).
Mechanisms Involved in DTH
The mechanisms involved in the sensitization to DTH and the elucidation of the reaction following antigenic challenge are now well understood. It is important to underscore that, as with antibody-mediated hypersensitivity reactions, previous exposure to the antigen is required to generate DTH reactions. Such exposure (the sensitization stage) activates and expands the number of antigen-specific TH1 and TH17 cells that, when subsequently challenged with the same antigen, respond by producing cytokines that promote DTH reactions (the elicitation stage). During the elicitation phase, activated TH1 and TH17 cells mediate the activation and recruitment of innate immune cells (antigen-nonspecific inflammatory cells) to the area of the reaction, including the activation and recruitment of macrophages and NK cells, and neutrophils. These stages are shown diagrammatically in Figure 17.1. The sensitization stage typically occurs over a 1–2 week period during which normal mechanisms of T-cell activation occur (see Chapter 10). In contrast, the elicitation stage requires approximately 18–48 hours from time of antigenic challenge to recruit and activate these cells, a period that culminates in the histological and clinical features of DTH. The clinical manifestations of DTH can last for several weeks or, in some cases, can be chronic (e.g., DTH occurring in certain autoimmune diseases).
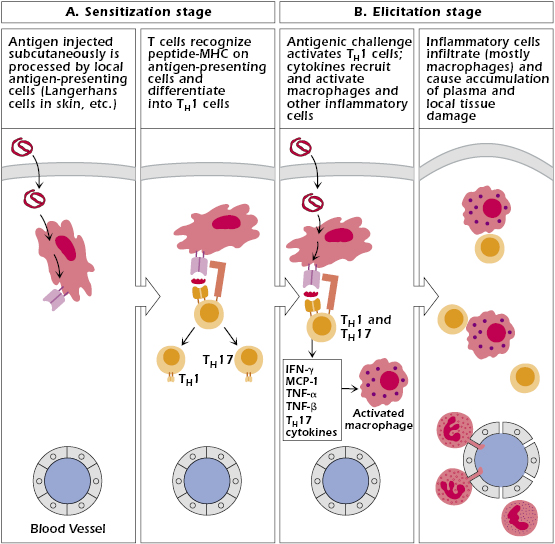
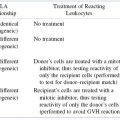
The antigen-challenged TH1 cells produce several cytokines during the elicitation stage, most notably chemokines and IFN-γ, which cause chemotaxis and activation of macrophages (Figure 17.2). The recruitment and activation of antigen-nonspecific cells by antigen-specific TH1 cells demonstrate the interaction between acquired and innate immunity discussed in Chapter 2. Another cytokine produced by these cells is IL-12. IL-12 suppresses the TH2 subpopulation and promotes the expansion of the TH1 subpopulation thereby driving the response to produce more TH1-synthesized cytokines that activate macrophages. Thus, IL-12 plays an important role in DTH. Table 17.1 summarizes the important cytokines involved in DTH reactions.
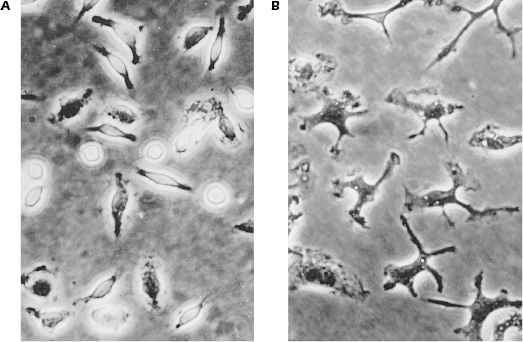
Table 17.1. Cytokines Involved in DTH Reactions
| Cytokinea | Functional Effectsb |
|---|---|
| IFN-γ | Activates macrophages to release inflammatory mediators |
| Chemokines | Recruit macrophages and monocytes to the site |
| MCP-1 | |
| RANTES | |
| MIP-1α | Influences neutrophil influx and preferentially attracts CD8+ T cells into the DTH reaction site |
| MIP-1β | Preferentially attracts CD4+ T cells into the DTH reaction site |
| TNF-α | Causes local tissue damage |
| TNF-β | Increases expression of adhesion molecules on blood vessels |
aMCP, membrane cofactor protein; MIP, macrophage inflammatory protein; TNF, tumor necrosis factor.
bAdditional functional effects are described in Chapter 12.
DTH reactions also involve CD8+ T cells, which are first activated and expanded during the sensitization stage of the response. These cells can damage tissues by cell-mediated cytotoxicity (see Chapter 11). Activation of CD8+ T cells occurs as a consequence of the ability of many lipid-soluble chemicals capable of inducing DTH reactions to cross the cell membrane (e.g., pentadecacatechol, which is the chemical that induces poison ivy). Within the cell, these chemicals react with cytosolic proteins to generate modified peptides that are translocated to the endoplasmic reticulum and then delivered to the cell surface in the context of MHC class I molecules. Cells presenting such modified self-proteins are subsequently damaged or killed by CD8+ T cells.
It should be apparent from the preceding discussion that many of the effector functions in DTH are performed by activated macrophages. In the most favorable circumstances, DTH results in destruction of an infectious organism (see below) that may have elicited the response in the first place. This destruction is believed to result predominantly from ingestion of the organism by macrophages, their activation by IFN-γ, followed by degradation by lysosomal enzymes, as well as by the by-products of the burst of respiratory activity, such as peroxide and superoxide radicals. Foreign tissues, tumor tissue, and soluble or conjugated antigens are dealt with in a similar manner.
Examples of DTH
Contact Sensitivity
Contact sensitivity (sometimes called contact dermatitis) is a form of DTH in which the target organ is the skin, and the inflammatory response is produced as the result of contact with sensitizing substances on the surface of the skin. Thus, it is primarily an epidermal reaction characterized by eczema at the site of contact with the allergen that typically peaks 48–72 hours after contact. The prototype for this form of DTH is poison ivy dermatitis (Figure 17.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree