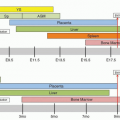
Globin gene mutations can increase the affinity of the hemoglobin molecule for oxygen and cause erythrocytosis. More than 90 high-oxygen-affinity variants have been reported in http://globin.cse.psu.edu/ and Wajcman and Galacteros.
1 Familial erythrocytosis is a valuable clue to the presence of a high-oxygen-affinity hemoglobin variant; isolated cases are caused by new mutations. These
α– or
β-globin chain mutations are dominant disorders, expressed clinically in the heterozygote. They may be lethal in homozygotes if they affect the
α-globin chain and are expressed in utero. One
γ-globin variant (HbF-Monserrato-Sassari,
HBG2 cys93arg) in a normal newborn and a possible
δ-globin variant (Hb Noah Mehmet Oesteurk,
HBD his143tyr) have been described.
Several homozygotes for
β-globin high-oxygen-affinity variants have been described and these individuals can have more severe disease.
2,
3,
4,
5 Compound heterozygotes with a high-oxygen-affinity hemoglobin and
β0-thalassemia have also been described, mimicking the homozygous state as normal adult hemoglobin A (HbA) is not present.
α-Globin Chain Variants
Because there are four α-globin genes, most stable α-globin variants form 25% or less of the total hemoglobin, compared with 40% to 50% for β-globin variants. As a result, the clinical effects of α-globin variants are less striking than those of β-globin variants. However, the coincident inheritance of a β-thalassemia gene can modulate the concentration of high-affinity α-variant hemoglobins and homozygosity for a high-oxygen-affinity variant affecting α-globin chains has been described.
Hb Chesapeake (
HBA arg92leu) was the first reported highaffinity hemoglobin variant.
11 It was discovered in an 81-year-old patient with erythrocytosis, an abnormal hemoglobin detected by hemoglobin electrophoresis, and erythrocytes with increased oxygen affinity. Fifteen members of the proband’s family were similarly affected. Hb Chesapeake represented ˜20% of the total hemoglobin. With a P
50 of 19 mm Hg (normal ˜26 mm Hg), Hb Chesapeake produced moderate erythrocytosis. The mutation affected an invariant residue that stabilizes the R state at the
α1β2 area of contact, making the T conformer less favored.
Hb Nunobiki (
HBA1 arg141cys), is one of four mutations of this invariant residue, all of which exhibit high oxygen affinity and moderate to mild erythrocytosis.
12 This group of mutations represents an interesting cluster of variants that illustrates the effects of different mutations at the same amino acid residue. As a mutant of the 3′-
HBA1 gene that is expressed to a lesser extent than the 5′-
HBA2 gene, Hb Nunobiki makes up ˜13% of the hemolysate and is accompanied by only mild erythrocytosis. High oxygen affinity is a result of the breaking of the C terminal-to-C terminal salt bridge that is indispensable for the stabilization of the T state, favoring the R state.
β-Globin Chain Variants
All possible single-base mutations of the β99 site disturbing the α1β2 area of contact have been described and include Hb Kempsey (HBB asp99asn), Hb Yakima (asp99his), Hb Radcliffe (asp99ala), Hb Ypsilanti (asp99tyr), Hb Hotel-Dieu (asp99gly), Hb Chemilly (asp99val), and Hb Coimbra (asp99glu). As expected for stable β-globin chain variants, all are present at 40% to 50% of the hemolysate, exhibit moderately high oxygen affinity, and are characterized clinically by erythrocytosis. Hbs Kempsey, Radcliffe, and Hotel Dieu have a decreased response to 2,3-DPG. Hbs Ypsilanti and Radcliffe form stable hybrid tetramers in the hemolysates in which the abnormal β chains coexist with normal β chains.
Six of the possible seven mutations of the C-terminal CAC (tyr) codon have also been described. One of them, Hb Cochin-Port Royal (tyr146arg), has nearly normal oxygen affinity but decreased 2,3-DPG interaction and Bohr effect.
13Three mutations of β82 lys have been described: Hb Rahere (lys82thr), Hb Helsinki (lys82met), and Hb Providence (lys82asn). All have moderately high oxygen affinity and moderate erythrocytosis.
These mutants have drastically reduced 2,3-DPG binding as a result of the elimination of one of the normal binding sites for this allosteric effector. Hb Porto Alegre (
HBB ser9cys) has high oxygen affinity and a tendency to aggregate, but erythrocytosis is not present.
14 Polymerization of Hb Porto Alegre is based on the formation of disulfide bonds in oxygenated samples and is different from HbS polymerization. Polymerization of this mutant diminishes heme-heme interaction and increases the oxygen affinity.
Hb Tak (
HBB 147(+AC), modified C-terminal sequence: 147thr-lys-leu-ala-phe-leu-leu-ser-asn-phe-157tyr-COOH), is elongated by 11 amino acid residues.
15,
16 It forms 40% of the hemolysate, has a very high oxygen affinity with no co-operativity, and no allosteric interaction with pH or 2,3-DPG. The C terminus of the
β-globin chain is actively involved in the conformational changes of the hemoglobin molecule by stabilizing the T state. By having these stabilizing interactions disrupted, Hb Tak is totally frozen in the R state. Hb Tak is also slightly unstable. In spite of these severe functional abnormalities, a heterozygous patient did not have erythrocytosis. The extreme biphasic nature of the hemoglobin-oxygen affinity curve observed in mixtures of Hb Tak and HbA suggests that hybrid tetramer (
α2βAβTak) formation is absent. The top portion of the oxygen equilibrium curve is normal, and it begins to be abnormal only at <40% saturation. Because physiologic oxygen exchange occurs most commonly above that level of saturation, the tissues may not be hypoxic, removing the stimulus for increased erythropoiesis.
Clinical Features
Patients with high-affinity hemoglobins and erythrocytosis have a benign clinical course and rarely have complications, apart from a ruddy complexion. Splenomegaly is typically absent. Hemoglobin concentration and hematocrit are increased variably, and usually only moderately, suggesting that modulation by variations in other genes might affect the physiologic response to hypoxia. Some patients with Hb Malmo (
HBB his97gln) have been reported to be symptomatic and to benefit from phlebotomy and the transfusion of normal blood, but this clinical course is an exception.
17Many cases of high-oxygen-affinity hemoglobins are diagnosed during a routine hematologic examination or when the family of a proband known to have erythrocytosis is examined. In very limited studies, exercise capacity in the laboratory and the indices of working capacity and cardiac tolerance were similar in patients with high-oxygen-affinity hemoglobins and in controls.
18 It has been suspected that carriers of these variants may have enhanced athletic performance under some circumstances, and this has led to the unfortunate and sometimes fatal use of erythropoietin or transfusion to enhance performance in competitive athletics.
In a population-based study of erythrocytosis, high-oxygen-affinity variants accounted for 3% of all cases.
19 By early diagnosis of high-affinity hemoglobins, unnecessary invasive diagnostic procedures and inappropriate therapeutic interventions, such as cardiac catheterization, can be avoided. Patients have received
32P treatment based on a mistaken diagnosis of polycythemia vera.
Increased morbidity or mortality in mothers with high-oxygen-affinity hemoglobins or their offspring has not been observed, suggesting that the affinity of the mother’s hemoglobin is irrelevant with respect to oxygen delivery to the fetus.
18 Low ambient pO
2, as in unpressurized airplanes and ascent to altitude, do not represent a risk, because high-affinity hemoglobins are avid for oxygen.
Hypothetically, carriers should be less prone to “the bends” during deep sea diving, because of slower oxygen release during ascension.