Abstract
Most women treated for early-stage breast cancer will be long-term survivors. In 2016 more than 3.5 million breast cancer survivors were expected in the United States alone and millions more worldwide. Breast cancer and its treatment can have a heavy impact on a woman’s physical, psychological, social, vocational, and spiritual well-being beyond the immediate time frame of active therapy. After treatment of breast cancer, regular follow-up with a health care provider is prudent to ensure prompt recognition of recurrences or second primary cancers as well as to adequately assess for complications of treatment, foster adherence to recommended therapy and screening, and provide psychosocial and decision-making support. The recent recommendations for long-term follow-up and management are reviewed.
Keywords
surveillance for locoregional recurrences or new primary disease, detecting distant relapse, body image concerns, lymphedema and other local sequelae, osteoporosis, musculoskeletal complaints, chemotherapy-related amenorrhea, ovarian dysfunction, infertility, pregnancy, hormonal symptoms, sexual dysfunction, fatigue, cognitive impairment, psychosocial concerns, thrombosis, cardiac disease, treatment-related cancers, survivorship care planning
Most women treated for early-stage breast cancer will be long-term survivors. In 2016 more than 3.5 million breast cancer survivors were expected in the United States alone and millions more worldwide. Breast cancer and its treatment can have a heavy impact on a woman’s physical, psychological, social, vocational, and spiritual well-being beyond the immediate time frame of active therapy. After treatment of breast cancer, regular follow-up with a health care provider is prudent to ensure prompt recognition of recurrences or second primary cancers as well as to adequately assess for complications of treatment, foster adherence to recommended therapy and screening, and provide psychosocial and decision-making support. Relatively few studies have evaluated the risks and benefits, let alone cost-effectiveness, of surveillance and intervention modalities in breast cancer survivors. Nevertheless, several recommendations can be made based on available evidence and expert consensus. Box 81.1 details current recommendations for standard follow-up care based on an evidence-based review conducted by an expert panel convened by the American Society of Clinical Oncology (ASCO) and the American Cancer Society (ACS). These recommendations can also be adopted for men with a history of breast cancer, recognizing that data are limited in this population.
Target population: Female adult breast cancer survivors
Target audience: Primary care providers, medical oncologists, radiation oncologists, and other clinicians caring for breast cancer survivors
Methods: An expert panel was convened to develop clinical practice guideline recommendations based on a systematic review of the medical literature
Surveillance for Breast Cancer Recurrence
History and Physical Examination
Recommendation 1.1: It is recommended that primary care clinicians (a) should individualize clinical follow-up care provided to breast cancer survivors based on age, specific diagnosis, and treatment protocol and as recommended by the treating oncology team (LOE = 2A); and (b) should make sure the patient receives a detailed cancer-related history and physical examination every 3–6 months for the first 3 years after primary therapy, every 6–12 months for the next 2 years, and annually thereafter (LOE = 2A).
Screening the Breast for Local Recurrence or a New Primary Breast Cancer
Recommendation 1.2: It is recommended that primary care clinicians (a) should refer women who have received a unilateral mastectomy for annual mammography on the intact breast and, for those with lumpectomies, an annual mammography of both breasts (LOE = 2A); and (b) should not refer for routine screening with MRI of the breast unless the patient meets high-risk criteria for increased breast cancer surveillance as per ACS guidelines (LOE = 2A).
Laboratory Tests and Imaging
Recommendation 1.3: It is recommended that primary care clinicians should not offer routine laboratory tests or imaging, except mammography if indicated, for the detection of disease recurrence in the absence of symptoms (LOE = 2A).
Signs of Recurrence
Recommendation 1.4: It is recommended that primary care clinicians should educate and counsel all women about the signs and symptoms of local or regional recurrence (LOE = 2A).
Risk Evaluation and Genetic Counseling
Recommendation 1.5: It is recommended that primary care clinicians (a) should assess the patient’s cancer family history; and (b) should offer genetic counseling if potential hereditary risk factors are suspected (e.g., women with a strong family history of cancer [breast, colon, endometrial] or age 60 years or younger with triple-negative breast cancer; LOE = 2A).
Endocrine Treatment Impacts, Symptom Management
Recommendation 1.6: It is recommended that primary care clinicians should counsel patients to adhere to adjuvant endocrine (antiestrogen) therapy (LOE = 2A).
Screening for Second Primary Cancers
Cancer Screenings in the Average-Risk Patient
Recommendation 2.1: It is recommended that primary care clinicians (a) should screen for other cancers as they would for patients in the general population; and (b) should provide an annual gynecologic assessment for postmenopausal women on selective estrogen receptor modulator therapies.
Assessment and Management of Physical and Psychosocial Long-Term and Late Effects of Breast Cancer and Treatment
Body Image Concerns
Recommendation 3.1: It is recommended that primary care clinicians (a) should assess for patient body image/appearance concerns (LOE = 0); (b) should offer the option of adaptive devices (e.g., breast prostheses, wigs) and/or surgery when appropriate (LOE = 0); and (c) should refer for psychosocial care as indicated (LOE = IA).
Lymphedema
Recommendation 3.2: It is recommended that primary care clinicians (a) should counsel survivors on how to prevent/reduce the risk of lymphedema, including weight loss for those who are overweight or obese (LOE = 0); and (b) should refer patients with clinical symptoms or swelling suggestive of lymphedema to a therapist knowledgeable about the diagnosis and treatment of lymphedema, such as a physical therapist, occupational therapist, or lymphedema specialist (LOE = 0).
Cardiotoxicity
Recommendation 3.3: It is recommended that primary care clinicians (a) should monitor lipid levels and provide cardiovascular monitoring, as indicated (LOE = 0); and (b) should educate breast cancer survivors on healthy lifestyle modifications, potential cardiac risk factors, and when to report relevant symptoms (shortness of breath or fatigue) to their health care provider (LOE = I).
Cognitive Impairment
Recommendation 3.4: It is recommended that primary care clinicians (a) should ask patients if they are experiencing cognitive difficulties (LOE = 0); (b) should assess for reversible contributing factors of cognitive impairment and optimally treat when possible (LOE = IA); and (c) should refer patients with signs of cognitive impairment for neurocognitive assessment and rehabilitation, including group cognitive training if available (LOE = IA).
Distress, Depression, Anxiety
Recommendation 3.5: It is recommended that primary care clinicians (a) should assess patients for distress, depression, and/or anxiety (LOE = I); (b) should conduct a more probing assessment for patients at a higher risk of depression (e.g., young patients, those with a history of prior psychiatric disease, and patients with low socioeconomic status; LOE = III); and (c) should offer in-office counseling and/or pharmacotherapy and/or refer to appropriate psycho-oncology and mental health resources as clinically indicated if signs of distress, depression, or anxiety are present (LOE = I).
Fatigue
Recommendation 3.6: It is recommended that primary care clinicians (a) should assess for fatigue and treat any causative factors for fatigue, including anemia, thyroid dysfunction, and cardiac dysfunction (LOE = 0); (b) should offer treatment or referral for factors that may impact fatigue (e.g., mood disorders, sleep disturbance, pain, etc) for those who do not have an otherwise identifiable cause of fatigue (LOE = I); and (c) should counsel patients to engage in regular physical activity and refer for cognitive behavioral therapy as appropriate (LOE = I).
Bone Health
Recommendation 3.7: It is recommended that primary care clinicians (a) should refer postmenopausal breast cancer survivors for a baseline DEXA scan (LOE = 0); and (b) should refer for repeat DEXA scans every 2 years for women taking an aromatase inhibitor, premenopausal women taking tamoxifen and/or a GnRH agonist, and women who have chemotherapy-induced, premature menopause (LOE = 0).
Musculoskeletal Health
Recommendation 3.8: It is recommended that primary care clinicians (a) should assess for musculoskeletal symptoms, including pain, by asking patients about their symptoms at each clinical encounter (LOE = 0); and (b) should offer one or more of the following interventions based on clinical indication: acupuncture, physical activity, and referral for physical therapy or rehabilitation (LOE = III).
Pain and Neuropathy
Recommendation 3.9: It is recommended that primary care clinicians (a) should assess for pain and contributing factors for pain with the use of a simple pain scale and comprehensive history of the patient’s complaint (LOE = 0); (b) should offer interventions, such as acetaminophen, nonsteroidal anti-inflammatory drugs, physical activity, and/or acupuncture, for pain (LOE = I); (c) should refer to an appropriate specialist, depending on the etiology of the pain once the underlying etiology has been determined (e.g., lymphedema specialist, occupational therapist, etc; LOE = 0); (d) should assess for peripheral neuropathy and contributing factors for peripheral neuropathy by asking the patient about their symptoms, specifically numbness and tingling in their hands and/or feet, and the characteristics of the symptoms (LOE = 0); (e) should offer physical activity for neuropathy; and (f) should offer duloxetine for patients with neuropathic pain, numbness, and tingling (LOE = IB).
Infertility
Recommendation 3.10: It is recommended that primary care clinicians should refer survivors of childbearing age who experience infertility to a specialist in reproductive endocrinology and infertility as soon as possible (LOE = 0).
Sexual Health
Recommendation 3.11: It is recommended that primary care clinicians (a) should assess for signs and symptoms of sexual dysfunction or problems with sexual intimacy (LOE = 0); (b) should assess for reversible contributing factors to sexual dysfunction and treat, when appropriate (LOE = 0); (c) should offer nonhormonal, water-based lubricants and moisturizers for vaginal dryness (LOE = IA); and (d) should refer for psychoeducational support, group therapy, sexual counseling, marital counseling, or intensive psychotherapy when appropriate (LOE = IA).
Premature Menopause/Hot Flashes
Recommendation 3.12: It is recommended that primary care clinicians should offer selective serotonin-norepinephrine reuptake inhibitors, selective serotonin reuptake inhibitors, gabapentin, lifestyle modifications, and/or environmental modifications to help mitigate vasomotor symptoms of premature menopausal symptoms (LOE = IA).
Health Promotion
Information
Recommendation 4.1: It is recommended that primary care clinicians (a) should assess the information needs of the patient related to breast cancer and its treatment, side effects, other health concerns, and available support services (LOE = 0); and (b) should provide or refer survivors to appropriate resources to meet these needs (LOE = 0).
Obesity
Recommendation 4.2: It is recommended that primary care clinicians (a) should counsel survivors to achieve and maintain a healthy weight (LOE = III); and (b) should counsel survivors if overweight or obese to limit consumption of high-calorie foods and beverages and increase physical activity to promote and maintain weight loss (LOE = IA, III).
Physical Activity
Recommendation 4.3: It is recommended that primary care clinicians should counsel survivors to engage in regular physical activity consistent with the ACS guideline a
a Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:243-274.
and specifically: (a) should avoid inactivity and return to normal daily activities as soon as possible after diagnosis (LOE = III); (b) should aim for at least 150 minutes of moderate or 75 minutes of vigorous aerobic exercise per week (LOE = I, IA); and (c) should include strength training exercises at least 2 days per week and emphasize strength training for women treated with adjuvant chemotherapy or hormone therapy (LOE = IA).Nutrition
Recommendation 4.4: It is recommended that primary care clinicians should counsel survivors to achieve a dietary pattern that is high in vegetables, fruits, whole grains, and legumes; low in saturated fats; and limited in alcohol consumption (LOE = IA, III).
Smoking Cessation
Recommendation 4.5: It is recommended that primary care clinicians should counsel survivors to avoid smoking and refer survivors who smoke to cessation counseling and resources (LOE = I).
Care Coordination/Practice Implications
Survivorship Care Plan
Recommendation 5.1: It is recommended that primary care clinicians should consult with the cancer treatment team and obtain a treatment summary and survivorship care plan (LOE = 0, III).
Communication With Oncology Team
Recommendation 5.2: It is recommended that primary care clinicians should maintain communication with the oncology team throughout the patient’s diagnosis, treatment, and posttreatment care to ensure care is evidence-based and well-coordinated (LOE = 0).
Inclusion of Family
Recommendation 5.3: It is recommended that primary care clinicians should encourage the inclusion of caregivers, spouses, or partners in usual breast cancer survivorship care and support (LOE = 0).
Additional Resources
More information, including a data supplement with additional evidence tables, is available with the online version of this article at asco.org/guidelines/breastsurvivorship and asco.org/guidelineswiki ; patient information is available at onlinelibrary.wiley.com/doi/10.3322/caac.21319/pdf ; journal-based continuing education is available at acsjournals.com/ce
ACS, American Cancer Society; ASCO, American Society of Clinical Oncology; DEXA, dual-energy x-ray absorptiometry; GnRH, gonadotropin-releasing hormone; LOE, level of evidence.
Surveillance for Locoregional Recurrences or New Primary Disease
Monitoring for local recurrence or for development of a new primary breast cancer is an important component of follow-up care for breast cancer survivors. Unlike the rate of distant metastases, which peaks in the second year after diagnosis at 5% then it declined progressively until the eighth year, the rate of local recurrences remains steady for up to 10 years at 1% per year, especially with hormone receptor–positive disease. Risk factors include young age, lymphovascular invasion, multicentricity, and more advanced stage. In a meta-analysis of 12 studies with a total of 5045 women who underwent a mix of local and systemic therapies, more extensive lymph node involvement and more advanced stage of disease were associated with the 378 locoregional recurrences reported. Several studies have revealed the association between young age and increased risk of local recurrence. In one trial testing the utility of boost radiation, younger women were found to have higher risk of recurrence, with the absolute benefit from the addition of a boost found to be the greatest in the youngest patients. At 10 years’ median follow-up, boost radiation reduced risk of recurrence from 23.9% to 13.5% in those younger than 40 years of age, from 12.5% to 8.7% in those 41 to 50 years of age, and from 7.8% to 4.9% in those 51 to 61 years of age, and from 7.3% to 3.8% in those older than 60 years of age. The impact of patient age (≤45 years vs. >45 years) and the type of surgery were evaluated in a cohort of 813 Danish lymph node–negative breast cancer patients diagnosed between 1989 and 1998 and treated with mastectomy ( n = 515) or breast conservation therapy (BCT; lumpectomy with whole-breast radiation therapy; n = 298) and no adjuvant systemic treatment. Twenty-year local recurrence (LR) risk was 20% and developed throughout the entire 20-year period after BCT, whereas LR after mastectomy was 8.7% and developed within the first 10 years after mastectomy. Younger patients’ 20-year LR risk was higher than older patients’ (19% vs. 5%, p < .001) and was significantly associated with distant metastasis (DM; hazard ratio [HR] = 2.7, 95% confidence interval [CI] 1.8–4.2) and 20-year breast cancer mortality (HR = 2.7, 95% CI 1.7–4.4). BCT was associated with higher 20-year breast cancer mortality (HR = 1.5, 95% CI 1.0–2.4) and higher 20-year all-cause mortality (HR = 1.7, 95% CI 1.2–2.5) than mastectomy. In older patients, LR was not associated with DM, and breast cancer mortality was similar for BCT and mastectomy.
LRs, which account for only 10% to 30% of recurrences, are associated with reduced survival, especially in younger patients. The risk of death from breast cancer after ipsilateral breast tumor recurrence (IBTR) depends on the initial stage at diagnosis, with 15-year breast cancer mortality rate being at 16% for women with ductal carcinoma in situ, 32% for women with stage I, and 59% for women with stage II breast cancer. Several types of IBTR were described on the basis of the distance from the primary lumpectomy scar, the presence of in situ tumor, and the margin status. IBTRs close to the scar with in situ lesions and a negative surgical margin of the primary cancer behave as new primaries (NP) by this classification and have a distant disease–free survival similar to that of new primaries away from the scar or in the opposite breast. In contrast, IBTRs that occur close to the scar without in situ lesions (true recurrence) had significantly poorer prognosis than NP ( Table 81.1 ).
| Surgical Margin of Primary Cancer | In Situ Lesion of IBTR | Cause of IBTR | |
|---|---|---|---|
| IBTR occurred far from primary lumpectomy scar (FS group) | +/– | + | NP |
| +/– | – | TR | |
| – | + | NP | |
| IBTR occurred close to primary lumpectomy scar (CS group) | + | – | TR |
| – | TR |
However, it is not known whether earlier detection of recurrences lengthens life for these patients. Locoregional recurrences reflect either that the primary therapy failed to eradicate the cancer (in the majority of cases) or that, because of a predisposition, whether due to genetics or environmental exposure, an entirely new cancer has developed in the residual breast tissue. Patients with chest wall recurrences after mastectomy have very poor prognoses. After lumpectomy, new primaries are more likely in those who have BRCA1 or BRCA2 mutations, younger age at diagnosis, and possibly in those with lobular histology. Patients who have developed breast cancer after exposure to ionizing radiation (e.g., therapeutic mantle irradiation for Hodgkin disease) also carry a higher risk of new primary cancers in the radiation field. For the average breast cancer survivor, the risk of new contralateral breast cancer is doubled, making absolute risk 0.5% to 1% per year, which is reduced in women who receive adjuvant endocrine therapy. This risk is higher in premenopausal than postmenopausal women.
Given the evidence of benefit of screening mammography in lower risk women, annual mammogram of remaining breast tissue combined with regular history and physical examination is recommended for surveillance for locoregional recurrence and new primary disease in breast cancer survivors. Despite this recommendation, in a study of 391 women with early-stage breast cancer in Los Angeles; Washington, DC; and Kansas, it was found that 40% did not get a mammogram in the year after diagnosis.
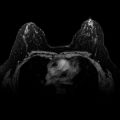
There has been interest in breast magnetic resonance imaging (MRI) in survivors. In a study of 969 women with a recent diagnosis of unilateral breast cancer without mammographic or clinical evidence of contralateral disease, breast MRI detected contralateral cancer in 30 women (3.1%). However, biopsies were conducted in 121 women, 75% of which were negative for cancer (9% of total number of women screened). There is no evidence that early detection with MRI improves outcomes, and false-positive findings using this expensive technology may be associated with significant physical and psychological morbidity. For women who are at greater than 20% risk of new primary disease, such as women with predisposing genetic mutation (e.g., BRCA1 or BRCA2 ) or history of radiation to the chest, MRI screening is recommended ( Table 81.2 ). MRI may also be considered for women with dense breasts and for those whose initial breast cancer was not seen on mammography, although there are no data to suggest that a woman whose first cancer was missed by mammography will have a second that is missed by mammography or that survival will be improved by MRI surveillance. The lack of evidence for benefit of MRI for early detection of future locoregional breast cancer events precludes recommending it as a standard surveillance modality in follow-up for average risk patients.
| Level of Recommendation for Annual MRI Screening | Population |
|---|---|
| Insufficient evidence to recommend a | Personal history of breast cancer |
| Heterogeneously or extremely dense breast on mammography | |
| Yes, based on evidence b | BRCA mutation, first-degree relative of BRCA carrier (herself untested) |
| Lifetime risk 20%–25% of breast cancer | |
| Yes, based on expert opinion c | Radiation to chest between 10 and 30 y of age |
| Li-Fraumeni, Cowden, and Bannayan-Riley-Ruvalcaba syndromes, as well as first-degree relatives with other rare genetic syndromes | |
| No, based on expert opinion | Women at <15% lifetime risk of breast cancer |
a Payment should not be a barrier. Screening decisions should be made on a case-by-case basis.
b Evidence from nonrandomized screening trials and observational studies.
The utility of high-resolution ultrasound (US) suffers from operator dependence, but one small study (27 patients) suggested a benefit when suspicious lesions are detected by examination or mammogram. When used in routine screening, US led to comparable cancer detection rate to mammography, with a greater proportion of invasive and node-negative cancers among US detections. However, false positives were more common with US screening. The addition of US to mammography in the evaluation of 2809 women, with at least heterogeneously dense breast tissue, yielded an additional 1.1 to 7.2 cancers per 1000 high-risk women, but it also increased the number of false positives. Hence, US should not be used in routine evaluation of woman with average risk. Recently tomosynthesis in combination with digital mammogram was associated with a decrease in recall rate and an increase in cancer detection rate and should be offered to patients whenever available.
Although breast self-examination did not improve survival in a large randomized study of unscreened healthy Chinese women, the efficacy of breast self-examination in survivors has not been rigorously evaluated. In light of the fact that the majority of locoregional recurrences are detected first by the patient herself, it is generally recommended that survivors consider regular breast self-examination, and at a minimum, be familiar with their own breasts and chest wall in order to be able to bring any concerns or changes to the attention of a health care provider.
The ASCO and the ACS updated their guidelines for follow-up of breast cancer survivors (see Box 81.1 ). Similar recommendations were suggested by the second international consensus guidelines for breast cancer in young women.
Detecting Distant Relapse
Distant relapse is more common than locoregional recurrence or second primary cancers. The occurrence of a distant relapse implies that the cancer had already spread by hematogenous, lymphatic, or serosal routes beyond the breast before definitive locoregional therapy, and that it was resistant to adjuvant therapy. Conventional predictors of risk of distant recurrence are similar to those for locoregional recurrence and include more advanced stage, higher grade and other markers of increased proliferation rate, hormone receptor negativity, HER2 positivity (although this is less clear now with the advent of trastuzumab adjuvant therapy), and younger age at diagnosis. More recently, evaluation of genetic signatures has provided additional prognostic and predictive information in some settings. Rates of distant recurrence are highest in the first few years after diagnosis but continue for at least 15 years, particularly for women with hormone receptor–positive disease. One study of 647 patients with stage II or III breast cancer found that the hazard curve for recurrence peaked at 3 years then fell abruptly for estrogen receptor (ER)-negative disease, but for ER-positive disease, peak recurrence rate was at 4 years and decline thereafter was slow. Specifically, 1-, 3-, 5-, and 10-year hazard rates for recurrence for ER-negative disease were 0.10, 0.10, 0.05, and 0.02, whereas rates for ER-positive disease were 0.05, 0.08, 0.06, and 0.03. Subtypes of breast cancer are also associated with location of recurrence. For example, HER2-positive metastatic disease is more likely to recur in the viscera and the central nervous system, whereas ER-positive recurrences are more likely to involve the bones, and lobular carcinomas may preferentially recur at serosal surfaces. ER-negative relapses tend to be visceral.
The majority of distant recurrences are detected by regular clinical evaluation (history and physical examination) or by patient reporting of symptoms prompting evaluation. When a patient reports new bone pain, dyspnea, jaundice, neurologic complaints, or any other symptom that may be attributable to metastatic disease, prompt evaluation for recurrence should be undertaken. The particular imaging used should be targeted to the symptom of concern. For example, in the setting of bone pain, a bone scan is a reasonable first step. If findings are suspicious of recurrent disease, additional imaging such as a chest, abdomen, and pelvic computed tomography (CT) scan or a positron emission tomography (PET)/CT can be done to assess the full burden of disease and evaluate for an optimal site to biopsy for confirmation of the diagnosis if possible. Blood work to evaluate for organ dysfunction should include complete blood count, chemistries including calcium, and liver function tests. When locoregional recurrence is detected, regardless of additional symptoms, thorough clinical staging is appropriate to assess for metastatic disease as the risk of synchronous metastatic disease is significant in this setting. In a medical record review of 2233 women treated in Milan in the 1970s and 1980s, local recurrence was found to be a risk factor for distant recurrence, especially when the local recurrence occurred in the first 2 years after diagnosis. In one older study, CT scanning of the chest revealed occult intrathoracic metastases in two-thirds of those with locoregional recurrence.
Two large randomized trials conducted in Italy have evaluated whether early diagnosis of metastatic disease affects survival. In the Interdisciplinary Group for Cancer Care Evaluation (GIVIO) study, 1300 women were randomized to receive either standard follow-up consisting of yearly mammograms as well as physical examinations every 3 months for 2 years and then every 6 months for the next 3 years or to receive standard follow-up plus blood tests at the time of each physical examination, annual bone scan and liver US, and chest x-ray every 6 months for 2 years and then annually. No difference was found between the groups in overall survival, disease-free survival, or health-related quality of life. In the second multicenter trial, 1243 women were randomized to either a control group that received the same standard follow-up procedures as in the GIVIO trial or to an intervention group that underwent screening chest x-ray and bone scan every 6 months in addition to standard follow-up. No difference was found in disease-free or overall survival between the two groups. A recent meta-analysis of five randomized trials involving a total of 4023 women supports these findings. None of these trials used newer imaging techniques such as CT or MRI, however, and none followed tumor markers. As more effective therapies for metastatic breast cancer (e.g., trastuzumab, aromatase inhibitors [AIs], and taxanes) are introduced into practice, it will be important to reinvestigate the role of more intensive imaging in the follow-up period. Modern imaging modality may allow early detection of relapse at a time when tumor burden is still small, which may help improve overall survival (OS) of these patients. Gioia and coworkers studied 813 patients with MRI and/or PET/CT and tumor markers (CEA and CA15-3) and were able to detect 29 MBC, 7 of which (24.1%) with limited disease (≤3 metastases to a single organ). Comparing overall survival in accordance to extent of MBC, the 3- and 5-year overall survival of patients with limited disease were 71.4% and 53.6%, and those with disseminated disease (56.7%) and (34.8%), respectively, but this difference was not significant.
At present, patients can be educated regarding the fact that any diagnostic test or procedure carries not only cost but also the 10% to 50% possibility of false-positive results, with ensuing anxiety, expense, and risk of complications from subsequent investigation. Therefore, routine screening for distant recurrence with imaging or blood work is not recommended, but patients are encouraged to report new symptoms.
Managing Long-Term and Late Effects of Cancer Treatment
The diagnosis of breast cancer and subsequent treatment may result in substantial long-term and late medical and psychosocial repercussions for survivors. Table 81.3 lists common late effects after surgery, radiation, and/or systemic therapy for early breast cancer. With careful follow-up, awareness, and attention to potential complications, patient health and comfort may be optimized, and psychological distress may be minimized. There are limited data regarding many of these potential sequelae of breast cancer therapy, particularly in the very long term and in younger patients, making survivorship research a priority for this population.
| Effect | Management Options |
|---|---|
| Surgical | |
| Cosmetic effects | Plastic surgery |
| Functional disability of arm or chest wall, pain | Physical therapy |
| Scarring/adhesions | Plastic surgery |
| Lymphedema | Physical therapy, avoid trauma to involved arm |
| Radiation | |
| Second malignancies | Image masses arising near radiation field |
| Xerophthalmia, cataracts | Regular visits to ophthalmologist |
| Hypothyroidism | Check thyroid-stimulating hormone if symptoms of hypothyroidism |
| Pneumonitis, pulmonary fibrosis | Symptomatic management |
| Cardiac damage | Lifestyle risk reduction (diet, exercise) |
| Lymphedema | As above |
| Systemic Therapy | |
| Second malignancies (myelodysplasia and leukemia) | Check complete blood count if symptoms of leukemia arise |
| Ototoxicity (e.g., cisplatin) | Symptomatic management |
| Cardiomyopathy (e.g., anthracyclines) | Symptomatic management |
| Renal toxicity (e.g., cisplatin) | Symptomatic management |
| Premature menopause and infertility (e.g., alkylating agents) | Referral to infertility specialist |
| Menopausal symptoms and sexual dysfunction | SSRI, SSNRI, gabapentin, counseling |
| Osteoporosis (e.g., hormonal therapy, chemotherapy) | Calcium, vitamin D, exercise, bisphosphonate |
| Neuropathy (e.g., taxanes and platinums) | Symptomatic management |
| Cognitive dysfunction, weight gain, fatigue | Exercise, rule out depression and anemia |
Lymphedema and Other Local Sequelae
Lymphedema of the upper extremity is a sequela of ipsilateral breast irradiation and of axillary surgery. Some women also suffer persistent chest wall pain after mastectomy, as well as continuing local difficulties subsequent to breast reconstruction. The risk of implant infection or skin breakdown declines over time, but discomfort may persist. Risk of lymphedema rises with increasing intensity of axillary surgery or radiation, obesity, and trauma to the arm. With the advent of sentinel node biopsies allowing many women to forgo full axillary dissections, the incidence of significant lymphedema has decreased. In the American College of Surgeons Oncology Group Z0011 prospective trial randomizing clinically node-negative women with positive sentinel lymph node biopsies to axillary dissection or no axillary dissection, there were higher rates of wound infections ( p = .0016), axillary seromas ( p = .0001), paresthesias ( p = .0001), and lymphedema ( p = .0001) in the group that received full axillary dissection. Reported 12-month rates of subjective lymphedema were 2% in those who underwent only sentinel node biopsy and 13% in those who also underwent full axillary dissection. By arm measurement, 12-month lymphedema rates were 6% versus 11%, respectively, again favoring sentinel node biopsy alone. The advent of a novel procedure that spares the lymph nodes draining the arm, Axillary reverse mapping (ARM), is promising for further decrease in the risk of lymphedema without compromising the quality of the evaluation of axillary lymph nodes. Other investigators were not able to confirm these results, however.
Management of lymphedema may include elevation of an affected body part, compression garments, massage and physical therapies, and, more rarely, surgery and diuretics. Before beginning any treatment for lymphedema, it is important to consider and evaluate for the possibility of tumor recurrence, infection, or venous thrombosis in the axilla. To minimize the chances of lymphedema, protection of the affected limb from infection, compression, venipuncture, exposure to intense heat, and abrasion may be prudent, although the utility of such measures has not been formally evaluated. Furthermore, because obesity is a risk factor for lymphedema, maintenance of a healthy weight and weight loss as needed may prevent or treat lymphedema. Ongoing studies are evaluating the role of local compression (i.e., compression sleeves) and exercise for lymphedema prevention.
Osteoporosis
Postmenopausal women on AIs and premenopausal women who become amenorrheic due to chemotherapy or who are receiving hormonal therapy are at risk for osteoporosis. In a randomized trial of exemestane versus placebo in 147 postmenopausal women with early breast cancer, the femoral neck bone density loss was 2.72% per year in the exemestane group and only 1.48% per year in the placebo group. In the National Cancer Institute of Canada Clinical Trials Group MA.17 trial of letrozole versus placebo after 5 years of tamoxifen, prevalence of lumbar spine osteoporosis after 2 years was 4.1% in those receiving letrozole versus 0% in those on placebo ( p = .064), but these results are confounded by the fact that more women in the placebo group were treated with bisphosphonates. In the Anastrozole and Tamoxifen Alone or in Combination (ATAC) trial, median 5-year changes in lumbar spine bone mineral density were –6.08% in the anastrozole group and +2.77% in the tamoxifen group.
Although tamoxifen appears to improve bone density in postmenopausal women via its proestrogenic effects, in premenopausal women, it has been associated with decreased bone mineral density. Ovarian suppression reduces bone mineral density in premenopausal women as well. However, the clinical significance of reduced bone mineral density in premenopausal women remains unclear because most studies have been done in the postmenopausal population. It has been recommended that bone density be monitored in survivors at risk for osteoporosis at baseline and every 1 to 2 years, although definitive evidence regarding the optimal frequency of monitoring is not available. Lifestyle modifications, including weight-bearing exercise, smoking cessation, and supplementation of dietary calcium and vitamin D, are also recommended for those at risk for osteopenia.
Bisphosphonate (BP) therapy has been demonstrated not only to reduce fractures in those with osteoporosis but also to limit bone loss in patients with normal bone mineral density who are starting on AIs. It is standard of care that anyone with osteoporosis receives bisphosphonate therapy, but prophylactic bisphosphonate treatment for those on AIs is more controversial because of the potential side effects, including jaw osteonecrosis. Despite encouraging results in postmenopausal or ovarian-suppressed women from many clinical trials suggesting a protective effect of BPs against recurrent or new primary breast cancer, they have not become widely used. The use of oral BP in women treated with tamoxifen showed no protective effect in a large database from Kaiser Permanente. Another large database study showed improvement in breast cancer–specific survival in postmenopausal women who used oral BP for at least 18 months after the diagnosis of breast cancer. The role of BP was reviewed by the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) in a meta-analysis that included 26 trials and 18,766 participants. Using BP therapy had no apparent effect on any outcome in premenopausal women, but among 11,767 postmenopausal women, it produced significant reductions in recurrence (relative risk [RR] 0.86, 95% CI 0.78–0.94; 2 p = .002), distant recurrence (0.82, 0.74–0.92; 2 p = .0003), bone recurrence (0.72, 0.60–0.86; 2 p = .0002), and breast cancer mortality (.82, 0.73–0.93; 2 p = .002). On the basis of these data, a panel of European experts recommended the use of BP (intravenous zoledronic acid or oral clodronate) in postmenopausal women as a part of the adjuvant therapy for early-stage breast cancer, but no similar recommendations have been made in the United States to date.
Although raloxifene, a selective estrogen receptor modulator like tamoxifen, is used to prevent and treat osteoporosis in women without breast cancer and also to prevent breast cancer in those who have never previously been afflicted, it is not used in breast cancer survivors because it has not proven as effective as tamoxifen in treating breast cancer. Furthermore, raloxifene is not used in conjunction with tamoxifen because its action is so similar and may interfere with benefits or exacerbate risks of tamoxifen.
Musculoskeletal Complaints
Chemotherapy-induced neuropathy (CINP) is common during and after treatment with taxanes or platinum agents. Permanent hearing loss can occur with cisplatin, and peripheral neuropathy is particularly frequent with taxane therapy. Prevention clinical trials of the antiepileptic agents gabapentin, lamotrigine, and the antidepressants nortriptyline and amitriptyline have shown modest to no effect. Treatment options are limited, although physical therapy can help improve function, and there have been reports of some success with lessening neuropathy with glutamine and amitriptyline. Available data support the use of duloxetine, but they are inconclusive regarding tricyclic antidepressants (such as nortriptyline), gabapentin, and a compounded topical gel containing baclofen, amitriptyline HCL, and ketamine. However, considering the paucity of options for CINP, these agents may be offered on the basis of data supporting their utility in other neuropathic pain conditions.
Joint pains and generalized aches can continue after treatment with cytotoxic agents and are a tremendous problem for some women on hormonal therapies, especially AIs. Arthralgias due to AIs are usually symmetrical; often involve the hands, arms, knees, feet, pelvic bones, and back; and may be more severe in the morning. It is not known whether rates are higher with certain members of this drug class than others. Exercise and analgesics may improve arthralgia, and pain usually resolves within weeks of stopping an AI. A recent cross-sectional survey of 200 women receiving adjuvant AI therapy found that 47% reported joint pain and 44% reported joint stiffness. Body mass index of 25 to 30 kg/m 2 and prior tamoxifen therapy were found to be associated with a reduced likelihood of joint symptoms. Patients who had previously received a taxane were four times as likely as those who had not to report joint symptoms.
Chemotherapy-Related Amenorrhea, Ovarian Dysfunction, and Infertility
Infertility is a dreaded consequence of breast cancer treatment for some young women with the disease. It is recommended that providers address the possibility of infertility with patients treated during their reproductive years soon after their diagnosis and be prepared to discuss possible fertility preservation options or refer appropriately. For young women with breast cancer, adjuvant cytotoxic chemotherapy carries a risk of chemotherapy-related amenorrhea (CRA), associated ovarian dysfunction, and permanent cessation of menses (menopause) that increases with increasing patient age. Rates of CRA also vary based on regimen, with higher doses of alkylating agents increasing the likelihood of ovarian damage. A prospective study of 25- to 40-year-old women with breast cancer found that menstrual cycles persisted more often after regimens containing lower cumulative doses of cyclophosphamide. For women concerned about their risk of infertility, fertility-sparing efforts are available, including embryo cryopreservation, gonadotropin-releasing hormone agonists, and other techniques including cryopreservation of oocytes or ovarian tissue. Embryo freezing and oocyte cryopreservation require ovarian stimulation and may delay cancer treatment. Unfortunately, all these methods suffer from limited efficacy and safety issues.
Many young breast cancer survivors are interested in determining their menopausal status and their fertility potential in follow-up. Available measures for ovarian function in breast cancer survivors are limited and imprecise. Although the presence or absence of regular menses may reflect whether ovulation is occurring, some women menstruate without ovulating, and others ovulate without menstruating. There is also evidence that some women who initially regain menses after adjuvant chemotherapy go on to experience premature menopause in a few years. Less often, some women who assume they are postmenopausal after adjuvant chemotherapy because they do not menstruate for several years later resume menstruating. In a study of 45 women who were treated with an AI after at least 6 months of CRA at the Royal Marsden Breast Unit, 10 resumed menses while taking the AI, 1 became pregnant, and 1 had a biochemical recovery of plasma estradiol to greater than 1500 pmol/L. It is therefore important not to transition women from tamoxifen to AI on the basis of CRA alone. Ovarian ultrasounds to measure antral follicle count and ovarian volume may play a role in determining whether follicular development is occurring, as may measurement of serum hormones such as estradiol, follicle-stimulating hormone, and luteinizing hormone, although these parameters also fluctuate substantially in survivors. Newer markers of ovarian reserve, including anti-müllerian hormone and inhibin B, may be more reliable measures of potential fertility.
Pregnancy
Many women diagnosed during childbearing years may be interested in having a subsequent pregnancy after breast cancer. There have been concerns that pregnancy increases the risk of recurrence of hormone receptor–positive tumors because of the high hormonal levels surrounding a pregnancy. However, the available evidence does not reveal any negative effect of subsequent pregnancy on the prognosis of young women with breast cancer. A Finnish study compared the survival of 91 women who had given birth more than 10 months after breast cancer diagnosis with 471 controls (matched by year of diagnosis, stage, and age). The controls were found to be 4.8 times (95% CI 2.2–10.3) more likely to have died in the years after the breast cancer diagnosis than were those who had given birth to a live child. Likewise, a comparison of more than 400 American women who gave birth more than 10 months after their breast cancer diagnosis to nearly 3000 matched controls who did not give birth after their diagnosis found that the pregnancies were associated with a decreased risk of death (RR 0.54, 95% CI 0.41–0.71). A similar trend was found in the Danish Breast Cancer Cooperative Group evaluation of outcomes of all women who became pregnant out of 5725 women younger than 45 years of age with breast cancer with 35,067 total patient-years of follow-up. The 173 women with subsequent pregnancy had a statistically nonsignificant trend toward reduction in risk of death compared with those who did not become pregnant (RR 0.55, 95% CI 0.28–1.06). Moreover, a study of the International Breast Cancer Study Group database reported that 94 patients who had a total of 137 pregnancies after breast cancer at 35 years of age or younger had better 5- and 10-year survival rates than 188 age-matched controls (92 ± 3% vs. 85 ± 3% for the 5-year data and 86 ± 4% vs. 74 ± 4% for the 10-year data). There were recurrences in 23% of those who became pregnant and in 54% of those who did not. A meta-analysis of 14 retrospective or population studies confirmed that women who become pregnant after breast cancer diagnosis had a 41% reduced risk of death compared with women who did not become pregnant (RR: 0.59, 90% confidence interval 0.50–0.70). This difference was seen particularly in women with history of node-negative disease. All of these studies may suffer from the “healthy mother bias,” which reflects the fact that the women who become pregnant may be at lower risk of recurrence at baseline than women who do not become pregnant. At present, women who do desire future pregnancies can be reassured by the lack of harm found in the existing limited data. Prospective research is ongoing.
It is commonly recommended that women wait at least 2 years after breast cancer treatment is completed before attempting conception to get through the period of highest risk of disease recurrence. Women who are taking tamoxifen or other hormonal therapy are urged to complete 5 years of therapy, during which pregnancy is contraindicated. Because rates of recurrence are significant long beyond the 2-year point and fertility wanes with aging, some women, particularly those at low risk of recurrence, may elect to pursue pregnancy soon after cancer treatment is completed. Young BRCA mutation carriers who are planning prophylactic oophorectomy in the future may be particularly eager to complete childbearing. Although it is important that providers and patients approach decisions about fertility preservation with caution, for some young women with breast cancer, a threat to the possibility of having a future biologic child has major psychosocial and developmental consequences. Many young women with breast cancer struggle with the competing interests of optimizing personal survival and the desire to become pregnant. Oncology providers should strive to provide accurate unbiased information and psychosocial assistance to young survivors facing such challenging situations.
There is no evidence for an increased rate of congenital abnormalities in children conceived from the eggs of patients exposed to chemotherapy in the past. In three large studies including nearly 4000 offspring of both male and female survivors of childhood cancer, when clearly hereditary cancers such as retinoblastoma were excluded, no statistically significant increase in cancers or malformations was detected in the offspring. Recently, a report from the Childhood Cancer Survivor Study that analyzed cases of congenital anomalies among 4699 children of female and male childhood cancer survivors, showed that the children of cancer survivors are not at significantly increased risk for congenital anomalies from their parent’s exposure to mutagenic cancer treatments. It is generally recommended that there be a minimum of several months between last dose of chemotherapy and conception.
Hormonal Symptoms and Sexual Dysfunction
Menopausal symptoms, including hot flashes, genitourinary problems, and sexual difficulties are common among breast cancer survivors due to the use of hormonal agents, development of CRA, and concerns about hormone replacement therapy in women who have been treated for breast cancer. In postmenopausal women after breast cancer therapy, a survey regarding menopausal symptoms revealed rates for the following conditions: hot flashes 65%, vaginal dryness 48%, night sweats 44%, difficulty sleeping 44%, depression 44%, and dyspareunia 26%. In a survey of 371 women who had been treated for breast cancer at or under 40 years of age, 77% of whom were premenopausal and 49% of whom were taking tamoxifen, responders reported the following menopausal symptoms: hot flashes 46%, vaginal dryness 51%, night sweats 46%, early awakening 52%, and dyspareunia 39%. It is important for physicians to ask women about dyspareunia and libido as well as about hot flashes and vaginal dryness. A randomized controlled trial of usual care versus treatment with assessment, education, counseling, and interventions directed at severe menopausal symptoms in 76 breast cancer survivors found that the treatment group reported improved menopausal symptoms ( p = .004) and sexual functioning ( p = .04) compared with the usual care group. Hormone replacement is not a recommended option for treatment of bothersome symptoms in these women. A Swedish randomized, noninferiority trial (HABITS) compared hormone replacement therapy with nonhormonal management. After a median follow-up of 4 years, 39 of the 221 women in the hormonal therapy arm and 17 of the 221 women in the control arm experienced a new breast cancer event (HR = 2.4, 95% CI = 1.3–4.2). Even in those with hormone receptor–negative disease, there is concern that the likelihood of a second primary cancer may be increased by hormonal exposure. Furthermore, even in prospectively randomized healthy women, the overall health risks of exogenous hormones have been shown to exceed benefits.
Nonestrogenic treatments for hot flashes and night sweats are believed to be safer than hormonal replacement. Among nonhormonal treatments, antidepressants (serotonin and norepinephrine reuptake inhibitor [SNRIs], selective serotonin reuptake inhibitor [SSRIs]), clonidine, gabapentin, and pregabalin have been proven to be efficacious in randomized controlled trials. Antidepressants, such as the SNRI venlafaxine, significantly reduce hot-flash frequency and intensity in women with breast cancer compared with a placebo. Venlafaxine (37.5–150 mg/day), paroxetine (10–20 mg/day), or citalopram (10–30 mg/day) are the most effective in reducing hot-flash frequency (from 14% to 58%) and severity compared with placebo. Some SSRIs, such as paroxetine, may deleteriously reduce serum levels of the active metabolite of tamoxifen, but venlafaxine and citalopram do not appear to affect these levels significantly. Gabapentin (300–900 mg), pregabalin (50–150 mg) and clonidine (0.1 mg) have also been shown to reduce hot flashes substantially. In addition, vitamin E has been shown to have modest effectiveness on vasomotor symptoms in women with breast cancer, but the placebo effect is also significant in most of these studies. Black cohosh and different formulas containing various phytoestrogens were tested in randomized trials with no proven benefit in controlling hot flashes in breast cancer patients.
For vaginal dryness caused by treatment-induced menopause or AI therapy, water-based lubricants are the first-line therapy. Women with vaginal atrophy or stenosis may benefit from vaginal dilatation as well as lubricants. Intravaginal estrogen therapy with estrogen creams or estrogen-impregnated rings may relieve genitourinary symptoms and may be associated with minimal systemic absorption of estrogen, but the potential risk that this estrogen therapy may increase likelihood of recurrence of a hormone receptor–positive tumor has not been well explored. Vaginal lubrication may improve libido indirectly, and behavioral counseling and psychotherapy may also be helpful. Transdermal testosterone was not found to improve libido in one randomized trial of postmenopausal female cancer survivors.
Fatigue
Fatigue is a common complaint in breast cancer survivors. Cancer-related fatigue (CRF) is often underreported, underdiagnosed, and undertreated. A multicenter study by Eastern Cooperative Oncology Group, designed to describe the prevalence and severity of CRF and its interference with daily living showed 52% incidence of moderate to severe fatigue in breast cancer survivors less than 5 years from treatment and 18% incidence in those who are more than 5 years from their treatment. ASCO and National Comprehensive Cancer Network, recommend screening for CRF after completion of primary therapy, as clinically indicated and at least annually. Evaluation and treatment of potential causes of fatigue, including pain, malnutrition, hypothyroidism, anemia, insomnia, and depression, is recommended. In those for whom no treatable cause is found, nonpharmacologic interventions such as energy conservation, exercise, psychotherapy, mindful meditation, and yoga are preferred over pharmacologic interventions. mindfulness-based stress reduction has been shown to improve mood, quality of life, and well-being more effectively than standard care in a randomized trial. Yoga has shown to improve sleep quality and reduce sleep medicine use in a randomized controlled trial. Psychostimulants such as modafinil and dextroamphetamine have shown mixed results in individual randomized studies, though Cochrane based review showed a small but significant improvement in fatigue with methylphenidate over placebo. Finally, a large meta-analysis was recently published by Mustian and colleagues that included 113 unique studies and enrolled 11,525 participants. Exercise, psychological, and exercise plus psychological interventions improved CRF during and after primary treatment, whereas pharmaceutical interventions did not.
Cognitive Impairment
Cognitive impairment during and after chemotherapy is of significant concern to many women. In a comparison of 31 women receiving chemotherapy, 40 women who had received chemotherapy in the past, and 36 healthy control participants, impaired cognition was found more frequently in women on active treatment than in control participants. Another study of cognitive dysfunction 2 years after chemotherapy was completed showed that rates were higher in the 34 who had received high-dose chemotherapy (32%) than the 36 who received standard-dose chemotherapy (17%), with the lowest rates (9%) seen in the 34 who never received chemotherapy. Interestingly, although more patients in the chemotherapy groups complained of difficulty with concentration, memory, thinking, or language, there was no significant correlation between self-report and objective measures of cognitive dysfunction in this study. A study of patients who received chemotherapy or local therapy for breast cancer (n = 70) or lymphoma (n = 58) 5 years earlier suggests that cognitive deficits may not completely resolve over time. Neuropsychiatric test scores were lower in those treated with chemotherapy in the past ( p < .04), especially with regard to verbal memory and psychomotor functioning. However, most deficits were subtle, with scores still in the normal range. A meta-analysis of cognitive functioning in breast cancer survivors who were treated with chemotherapy showed that observed cognitive deficits are small in magnitude and limited to the domains of verbal ability and visuospatial ability. The rate and severity of cognitive impairment experienced by breast cancer survivors may vary based partly on the type of treatment received.
Nonpharmacologic and pharmacologic treatments have been tried to improve cognitive functioning and quality of life in cancer survivors. A recent systematic review concluded that current evidence does not favor the pharmacologic management of cognitive alterations associated with breast cancer treatment. A single-arm pilot study of a cognitive-behavioral treatment called Memory and Attention Adaptation Training (MAAT) found that 29 women complaining of difficulties with memory and attention at a mean of 8 years after chemotherapy for stage I or II breast cancer experienced improvements in their symptoms immediately after the intervention and at 2-month and 6-month follow-ups. MAAT consisted of four monthly visits, a telephone call in between each visit, and a workbook. Cognitive function, quality of life, and standard neuropsychological test scores rose as women were educated regarding memory attention, taught self-awareness and self-regulation (relaxation, scheduling, and pacing), and instructed in compensatory strategies. A randomized controlled trial evaluated the efficacy of training in memory or speed of processing for improving cognitive function in breast cancer survivors. Both interventions improved self-reported measures of cognitive function, symptom distress, and quality of life. There are limited data on efficacy of central nervous system stimulants in improving cognitive impairment. Agents that are under study include l-carnitine, modafinil, bupropion, and SSRIs. Preliminary data suggest that modafinil may lessen symptoms of “chemo brain,” such as memory problems and difficulties concentrating. In a randomized study examining the effects of modafinil on fatigue, a secondary analysis to assess the effect of modafinil on cognitive function was performed. The results showed that modafinil improved cognitive performance in breast cancer survivors by enhancing some memory and attention skills. However, a multicenter randomized controlled trial in brain cancer patients showed that modafinil did not exceed the effect of placebo and double-blind randomized trial of d -methylphenidate during chemotherapy was found to have no beneficial effect on cognitive functioning.
Psychosocial Concerns
It is common for breast cancer survivors to experience psychosocial distress in follow-up. Distress can result from the fear of recurrence or secondary to physical, psychological, or social, problems. In a study of rates of depressive and anxiety disorders in 202 early-stage breast cancer patients younger than 60 years of age, prevalence of one or both conditions averaged 48% over the first year after diagnosis, twice that in the general population. After the first year, rates were found to return to the same as in the general population. Risk factors for psychosocial distress in women with breast cancer include young age at diagnosis and menopausal transition with therapy. Other risk factors include history of psychiatric disorders, cognitive impairment, and social problems like family or caregiver conflict or financial problems. Protective factors against persistent psychological strain in survivors of a variety of cancers have been found to include emotionally supportive relationships, active coping strategies, and emotional expression. Whether surveillance visits themselves provide psychological benefit is controversial and probably patient specific. Fear of recurrence is often a dominant psychological sequela to cancer. However, the inconvenience and often discomfort of surveillance testing, as well as the stress of waiting for test results and visits with clinicians can themselves generate anxiety. Randomized trials of surveillance after breast cancer have not found any overall positive psychological effects with more intensive surveillance strategies.
Antidepressant and antianxiety medications, individual and group psychotherapy, and relaxation and meditation therapy have all been found to improve psychosocial distress in survivors of cancer. Management of patients with clinical psychiatric diagnoses such as anxiety, depression, or posttraumatic stress disorder is generally similar to that in patients without a history of cancer. An important component of follow-up care for breast cancer survivors is evaluation for distress as well as referral to counseling, support groups, stress management, or mental health providers when appropriate.
Thrombosis
Tamoxifen predisposes to clots, particularly in postmenopausal women. The risk of venous thromboembolism (VTE) is increased approximately threefold by tamoxifen, and some, but not all, studies have reported an increased risk of stroke as well. In a large breast cancer cohort comprising 13,202 patients, Walker and coworkers showed that VTE risk is the highest in the first 3 months after initiation of tamoxifen (a significant fivefold increased risk compared with non–tamoxifen users) then it drops to a nonsignificant twofold thereafter. Aromatase inhibitors are not associated with increased risk of VTE. Therefore a history of VTE or stroke is a relative contraindication to the use of tamoxifen and an indication for an AI. In the same study, the adjusted HR for VTE during chemotherapy was 10.8 (95% CI 8.2–14.4) compared with no chemotherapy and dropped to 8.4 (95% CI 4.9–14.2) in the month afterward. The risk of surgery-related VTE is 2.2 compared with patients who do not undergo surgery, regardless of the type of surgery. Because of the additionally elevated risk of clot after an operation, some providers ask patients to stop taking tamoxifen for 2 weeks before an elective surgery, particularly if there will be a substantial period of inactivity after the surgery.
Cardiac Disease
Mortality from breast cancer and cardiovascular disease (CVD) in women treated for breast cancer was compared in a cohort of 1413 breast cancer patients matched with same age controls. Compared with women without breast cancer, survivors of breast cancer are at higher risk for CVD-related mortality, but this risk seems to be time-dependent. Indeed, the authors of this study found that the risk of CVD death was lower among breast cancer survivors in the first 7 years (HR: 0.59, 95% CI 0.40–0.87; p < .001), whereas breast cancer survivors had nearly twice the risk of CVD mortality compared with those without breast cancer (HR: 1.9, 95% CI 1.4–2.7) after 7 years of their treatment. Because this study excluded anthracycline-induced cardiomyopathy the question of the other causes that may have been responsible was raised. Early menopause, with its associated lipid and clotting abnormalities, is one of the most important factors, which explains well the higher incidence of CVD in premenopausal women. However, other studies do not support this view. Coronary artery disease, conduction system disease, and valvular disease may result from chest wall radiation, although cardiac exposure is much reduced by newer techniques of irradiation. Studies using old radiation techniques in the 1970s and 1980s showed a significant association between radiation and cardiovascular mortality. These techniques exposed more of the heart and carried a 20% to 30% increased risk of cardiovascular disease. With current breast irradiation techniques including optimizing cardiac shielding, rates of cardiac compromise due to radiation are thought to be much lower. A recent large Surveillance, Epidemiology, and End Results/Medicare study found no increased risk of myocardial infarction in women diagnosed with left-sided versus right-sided breast cancers between 1992 and 2000, suggesting that modern radiation does not significantly add to cardiac toxicity. Some large European studies of patients treated in the 1990s concurred with these conclusions, but others from the United States and Europe found no difference between the rate of radiation-induced cardiac disease in those treated before or after 1990 and slight increase of risk in those who received radiation to the left breast especially if fields were accidentally set too deep (which occurred more often with those who had a body mass index >25).
The risk of congestive heart failure (CHF) with anthracyclines is well known to be cumulative dose–dependent, with risk approximately 5% at 400 mg/m 2 , 16% at 500 mg/m 2 , and 26% at 550 mg/m 2 (from a retrospective review of three clinical trials done during 1980–1990). These rates are significantly higher than what was previously reported on studies done in the 1970s by Von Hoff and colleagues. Lower cumulative doses of 200 to 300 mg/m 2 are associated with a risk of CHF in 0.5% to 2% of patients. CHF occur relatively early in the first 5 years after treatment. Late CHF is uncommon. In a published analysis of 10- to 13-year follow-up data from Southwest Oncology Group S8897, breast cancer patients who had received doxorubicin-containing chemotherapy no longer demonstrated reduced ejection fractions compared with the 5- to 8-year follow-up evaluation. Similar results on incidence of late left ventricular dysfunction (LVD) after more than 10-year follow-up on breast cancer patients were published by Murtagh and coworkers. Although a drop of left ventricular ejection fraction (LVEF) was observed in 1.9% of the patients, no LVD was seen. These data may underestimate rates of cardiac damage, however, because those studied were a selected observational subgroup consisting only of those who were alive and without recurrence.
Risk factors for anthracycline-induced cardiomyopathy are lifetime cumulative dose (exceeding 400–550 mg/m 2 of doxorubicin and 900–1000 mg/m 2 of epirubicin), age, radiation therapy to the chest, preexisting coronary and hypertensive heart disease, diabetes mellitus, peripheral vascular disease, and chronic obstructive pulmonary disease. Careful patient selection before anthracycline administration, liposomal formulation of doxorubicin, the use of less cardiotoxic anthracyclines (epirubicin), and continuous monitoring of heart function are likely to decrease the incidence of these toxicities. Slow infusion of doxorubicin instead of bolus infusion remains controversial. Recently, several investigators suggested the use of genetic testing to identify the patients at increased risk for doxorubicin-induced cardiac toxicity.
Trastuzumab heightens the risk of cardiac toxicity. In a meta-analysis including eight studies and involving 11,991 patients, Moja and colleagues found that trastuzumab significantly increased the risk of CHF defined as New York Heart Association class III or IV (2.5 vs. 0.4%; RR 5.11; 90% CI 3.00–8.72; p < .00001) and LVEF dysfunction (range 7.1%–18.6%; RR 1.83; 90% CI 1.36–2.47, p = .0008). Older age, lower ejection fraction at beginning of therapy, and antihypertensive medications predicted higher risk of cardiac dysfunction in the trastuzumab-treated patients. When trastuzumab was combined with paclitaxel or docetaxel, the incidence of CHF did not exceed 0.5% and 0.4%, respectively. All these studies suggested that trastuzumab-induced heart failure might be reversible. The standard protocol used to monitor heart function during trastuzumab treatment consists of a baseline evaluation of LVEF that is repeated every 3 months. Trastuzumab treatment is held if there are symptoms of heart failure, if LVEF drops below normal limits, or there is a drop of 16 or more percentile points. If LVEF returns to baseline on follow-up, it is considered safe to resume the treatment with close surveillance. The current surveillance guidelines during treatment were recently called into question because they do not have a strong evidence to support their use, nor is there any proof to support their utility. No screening or prophylaxis for cardiac damage is currently recommended in the follow-up period, and management of heart failure or coronary disease is the same as that in people who do not have a history of cancer. All patients should be advised to exercise regularly, avoid tobacco, and control lipid and blood pressure.
Treatment-Related Cancers
Breast cancer survivors are at risk for several types of treatment-related cancers such as myelodysplasia (MDS) or acute myeloid leukemia (AML) due to chemotherapeutics; uterine cancer, including endometrial cancer, or, more rarely, sarcoma due to tamoxifen; and lung cancer or angiosarcoma secondary to chest radiation.
Chemotherapy-induced MDS and AML are well known long-term side effects of chemotherapy, especially alkylating agents and topoisomerase II inhibitors. AML associated with topoisomerase-II inhibitors occurs within 5 years after treatment and is frequently associated with 11q23 cytogenetic abnormality, whereas AML after alkylating agents is often associated with abnormalities in chromosomes 5 and 7 and typically develops after 5 years of completing the treatment and has a poor prognosis. Anthracyclines (doxorubicin, epirubicin, and mitoxantrone) have both alkylating and topoisomerase-II inhibition functions to different degrees, which explains their variable leukemogenic potential. A large case-control study showed that the risk of mitoxantrone-containing regimens is dose dependent and significantly much higher than the other anthracycline-containing regimens. The risk was the highest in women younger than 65 years of age, with 4-year leukemia rate of 0.63% for cumulative doses of mitoxantrone less than 12 mg/m 2 and 3.89% for cumulative doses greater than 56 mg/m 2 . These regimens are no longer in use these days. The risk of the other anthracyclines is lower but nonetheless real. Five of 2305 breast cancer patients (0.2%) treated with doxorubicin and cyclophosphamide at different doses developed leukemia within 5 years of therapy in the National Surgical Adjuvant Breast and Bowel Project B-22 study. A higher rate was seen in another trial, in which 5 of 351 patients receiving high doses of cyclophosphamide-epirubicin-fluorouracil developed acute leukemia within 5 years of chemotherapy. Patients who were administered cumulative doses of epirubicin and cyclophosphamide higher than those used in standard regimens (≤720 and ≤6300 mg/m 2 , respectively) had an 8-year cumulative probability of developing AML/MDS of 4.97% (95% CI 2.06–7.87) compared with 0.37% (95% CI 0.13–0.61) for patients who received standard doses of these drugs. Furthermore, the addition of radiation therapy increases the risk of leukemia. In 3093 women who underwent curative breast surgery for cancer between 1982 and 1996, 12 women developed leukemia, all of whom had received radiotherapy and 10 of whom had also received chemotherapy. Thus the true rate of anthracycline-induced AML or MDS has been estimated to be 0.1% to 1.5% at 5 to 10 years, with radiation adding to the risk. Taxanes have the safest profile. No or rare cases of leukemia were reported with docetaxel- or with paclitaxel-containing regimens. The leukemogenic effect of granulocyte colony-stimulating factor (G-CSF) remains controversial. A systematic review of the effect of G-CSF in 25 randomized controlled trials showed an estimated RR of AML/MDS at 1.92 (95% CI 1.19–3.07; p = .007) in breast cancer patients treated with high-intensity therapy with growth factor compared with the less intense regimens and no growth factor. The relative contribution of dose intensity and growth factors is difficult to sort out in this context.
The risk of type 1 uterine cancer is also heightened by 2.5-fold due to the estrogen-agonistic property of tamoxifen in postmenopausal women. Type 1 endometrial cancer is the most common type and is estrogen dependent contrary to the uncommon type 2. The condition of the endometrium before initiation of tamoxifen was thought to determine the response of the endometrium to the drug. Thin endometrium (consistent with inactive atrophic histology) suggests a low chance of stimulation, whereas the presence of a benign endometrial polyp increases the incidence of atypical endometrial hyperplasia. However, the association of benign endometrial polyps with endometrial cancer was not found to be higher than with other benign conditions of the uterus. Hence, the presence of benign hyperplastic endometrial polyp should be considered a surrogate marker for endometrial activity rather than a precursor of cancer. The risk of tamoxifen-associated endometrial cancer is increased by the length of the treatment and does not abate after its cessation.
The notion that tamoxifen-associated endometrial cancer has a good prognosis has been called into question in recent years with long-term follow-up studies. Large retrospective studies (39,451 patients) have suggested a greater risk of aggressive uterine sarcomas (malignant mixed müllerian tumors [MMMT]) on tamoxifen relative to other histologic types of endometrial cancer. More recent and larger studies (85,930 patients) have refuted this notion and showed that there is increased risk of MMMTs in breast cancer patients in general regardless of the treatment with tamoxifen. However, in the absence of prospective assessment of this rare cancer, the issue remains unsettled, with studies showing results to support both assertions. Considering the role of estrogen and estrogen-like compounds in promoting endometrial cancer, it is recommended to use an AI instead of tamoxifen whenever possible and switch patients who received tamoxifen to an AI after 3 to 5 years of treatment to minimize the risks of this complication.
Menstrual cycle irregularities are common on tamoxifen, and cessation of periods may occur with or without continued ovarian function. The patient should be advised to use a reliable nonhormonal contraceptive method even if periods have ceased. Vaginal bleeding in postmenopausal women should be investigated by a gynecologist and with vaginal US. Routine regular screening has been proposed in asymptomatic patients on tamoxifen. However, the false-positive rate of vaginal US in this population is unacceptably high, and thus it is not recommended. Breast cancer therapy is not known to increase rates of ovarian cancer, but tamoxifen can cause benign ovarian cystic growths in postmenopausal women. Women who have strong family histories of breast or ovarian cancer or who are known to carry a BRCA mutation are at increased risk of ovarian cancer, and prophylactic oophorectomy is considered.
A larger cohort of 16,705 women treated for nonmetastatic breast cancer between 1981 and 1997 found significantly more sarcomas and lung cancers in the 13,472 who had received radiation compared with the 3233 who had not ( p = .02). In a recent overview of the published literature on radiation-induced sarcoma (RIS), the incidence rate was low at 0.2% of women with breast cancer treated with radiation. The treatment consists of wide surgical excision to negative margins with or without radiation. No adjuvant therapy is available nowadays for this cancer.
Age-appropriate routine cancer screening (e.g., for cervical and colon cancer) is recommended for breast cancer survivors, but no additional screening for non–breast cancers is recommended in a breast cancer survivor unless she is known to carry a genetic cancer mutation (such as BRCA ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree