EPSTEIN-BARR VIRUS
SUSAN E. HOOVER, JEFFREY P. ROSS, AND JEFFREY I. COHEN
ETIOLOGY
Epstein-Barr virus (EBV) is a member of the herpesvirus family (1) and, like other herpesviruses, contains a double-stranded DNA core surrounded by a nucleocapsid. A tegument layer containing several proteins envelops the nucleocapsid, which is surrounded by an outer lipid envelope studded with viral glycoprotein spikes.
EBV infects B lymphocytes and epithelial cells in the oropharynx (2). Infection of epithelial cells results in lytic infection with production of virions, lysis of the cell, and release of infectious virus. During virus replication, multiple EBV proteins are expressed including the EBV early antigens (EAs), DNA polymerase (the target of acyclovir), viral capsid antigen (VCA), and viral glycoproteins. Infection of B lymphocytes usually results in latent infection and immortalization of the cells in vitro, without production of infectious virus. These latently infected cells express only the EBV-encoded RNAs (EBER-1 and EBER-2), nuclear proteins (EBNA-1, -2, -3A, -3B, -3C, and LP), and latent membrane proteins (LMP-1, -2A, and -2B).
EBV has a worldwide distribution, and the vast majority of adults show serologic evidence of past infection. Primary EBV infection is usually asymptomatic or mildly symptomatic in early childhood; in contrast, symptomatic infectious mononucleosis is more common in individuals who become infected with EBV after the first decade of life. Transmission of EBV probably occurs most often by exposure to saliva from asymptomatic individuals who shed the virus. Serologic studies suggest that EBV is commonly spread among susceptible siblings within a family. EBV-associated infectious mononucleosis has been transmitted by blood transfusion.
The incubation period for symptomatic infectious mononucleosis is 30 to 50 days. During the first few weeks of the illness, peripheral lymphocytosis occurs, with a marked increase in T cells and natural killer cells; many of these cells appear as “atypical lymphocytes” on the peripheral blood smear. Most of the clinical features associated with infectious mononucleosis are manifestations of the vigorous cellular immune responses to EBV infection rather than to direct cytotoxic effects of the virus. B cells are also increased in number, and up to 20% may express EBV nuclear antigen during the first week of illness.
DIFFERENTIAL DIAGNOSIS
Other infectious or noninfectious diseases can produce the syndrome of infectious mononucleosis. Acute infection with cytomegalovirus (CMV), Toxoplasma gondii, human immunodeficiency virus type 1 (HIV-1), human herpesvirus type 6, or hepatitis viruses can result in fever, lymphadenopathy, sore throat, and atypical lymphocytes. Acute leukemia, lymphoma, and reactions to certain drugs (e.g., phenytoin and sulfonamides) can also produce a syndrome resembling infectious mononucleosis.
Other herpesviruses also produce neurologic symptoms similar to EBV. Infection with varicella-zoster virus also can result in encephalitis, myelitis, or neuropathy in nonimmunocompromised persons. Although encephalitis or radiculoneuropathy can occur in patients with CMV infection, these patients are usually immunocompromised, and the disease is progressive. Encephalitis due to herpes simplex virus (HSV) is usually localized to the temporal lobes.
CLINICAL MANIFESTATIONS
Infectious Mononucleosis
EBV-associated infectious mononucleosis is an acute illness characterized by fever, pharyngitis, lymphadenopathy, and mononuclear leukocytosis with atypical lymphocytes (3). Symptoms of infectious mononucleosis commonly include sore throat, headache, and malaise in more than 50% of patients, and myalgias, anorexia, nausea, and abdominal discomfort in 10% to 20% of individuals. Physical examination shows lymphadenopathy, pharyngitis, and splenomegaly in most patients, whereas 10% have hepatomegaly, jaundice, palatal enanthem, or rash. Posterior cervical lymphadenopathy is most often noted; however, any group of lymph nodes may be involved. A pruritic maculopapular eruption develops in nearly all patients after the administration of ampicillin. Important complications of infectious mononucleosis include splenic rupture, autoimmune hemolytic anemia, thrombocytopenia, hepatitis, myocarditis, airway obstruction from enlarged tonsils, and neurologic abnormalities. Neurologic complications are cited as the leading cause of death resulting from infectious mononucleosis, followed by secondary infection and splenic rupture. Fatalities occur in fewer than 0.03% of cases of infectious mononucleosis.
Rare individuals infected with EBV develop a chronic active infection, persisting >6 months and characterized by persistent adenopathy and hepatosplenomegaly and involvement of the lungs, eyes, or nervous system with EBV-infected lymphocytes. EBV infection of patients with the X-linked lymphoproliferative disorder results in a fatal disease characterized by lymphoid infiltration of organs, lymphomas, and opportunistic infections. Immunocompromised patients may develop EBV-associated lymphomas.
Neurologic Complications of Acute Epstein-Barr Virus Infection
Involvement of the nervous system in infectious mononucleosis is more common than generally appreciated. About 50% of patients have headache on presentation. Neck stiffness without meningitis is a common finding. In one study, about 25% of patients (43 of 162) had more than five cells per cubic millimeter in the cerebrospinal fluid (CSF) (4). Many of these patients had no symptoms of meningitis. Abnormal electroencephalograms (EEGs), which most often reveal diffuse slowing patterns, have also been reported in patients with infectious mononucleosis, but without clinically significant central nervous system (CNS) disease (4).
Significant neurologic complications of acute infectious mononucleosis are rare, occurring in fewer than 0.5% of more than 4,300 cases of infectious mononucleosis in one review (5). Neurologic complications, however, are an important cause of morbidity in infectious mononucleosis and have been reported in 6% to 7% of patients hospitalized with infectious mononucleosis (6,7,7a). A study of children admitted to the hospital with new neurologic symptoms found acute EBV infections in 4% of patients and reactivated infections in 17% of patients (8).
CNS symptoms may occur shortly before, during, or after infectious mononucleosis or following acute EBV infection in the absence of symptomatic infectious mononucleosis. Cases of neurologic symptoms associated with infectious mononucleosis before the 1970s, when EBV-specific serologic tests were developed, must be regarded with caution because a number of other infectious agents can produce the clinical syndrome of mononucleosis. Only 1 of 14 cases of neurologic complications associated with primary EBV infection reported by Grose et al. (9) presented with clinical infectious mononucleosis. Similarly, only 1 of 21 children with EBV encephalitis identified prospectively at the Hospital for Sick Children in Toronto had infectious mononucleosis; the others had nonspecific symptoms of fever and headache (9a).
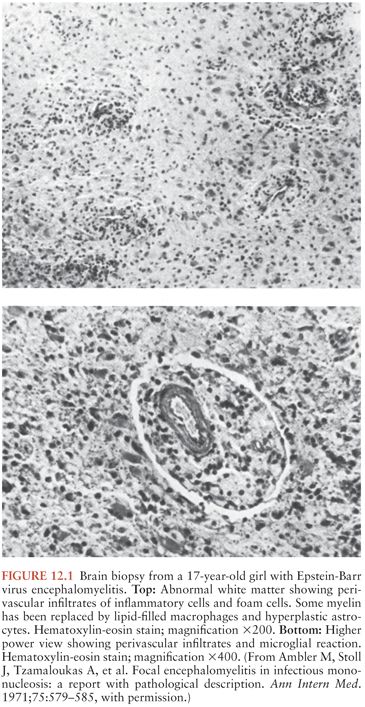
Examination of biopsy or autopsy specimens suggests that immunologic mechanisms are probably more important in the pathogenesis of neurologic complications than active viral replication. Perivascular lymphocytic infiltrates, which may include atypical lymphocytes, are often found in the leptomeninges, CNS parenchyma, nerve roots, and peripheral nerves (10) (Fig. 12.1). Additional findings include parenchymal edema and microglial proliferation (11). Inflammatory demyelinating lesions similar to those found in multiple sclerosis or “postinfectious” encephalomyelitis or neuritis have also been described (10,12). A report of antineuronal antibodies in the serum of a patient with EBV-associated acute cerebellar ataxia, but not in patients with other neurologic diseases, provides support for an immune-mediated mechanism for CNS disease (13).
These studies indicate that the pathogenesis of EBV-associated neurologic disease is different from that of HSV CNS disease. Although viral proteins are present in the brain of patients with herpes simplex encephalitis, brain biopsies from patients with EBV encephalitis do not show viral nucleic acids or proteins (14). Thus, autoimmune mechanisms are probably responsible for the pathogenesis of EBV-associated CNS disease.
Aseptic Meningitis
Aseptic meningitis is the most common neurologic complication of primary EBV infection. Patients present with headache, malaise, stiff neck, and occasionally photophobia (15). The CSF usually shows a mild to moderate lymphocytic pleocytosis, occasionally with atypical lymphocytes. The CSF protein concentration is normal or mildly elevated, and the glucose concentration is usually normal (15,16). Although the CSF opening pressure is usually normal or slightly elevated, in some patients, it is markedly increased, and repeated lumbar puncture provides symptomatic relief (17). Aseptic meningitis associated with EBV has a good prognosis and usually resolves without CNS sequelae.
Encephalitis
Patients having encephalitis associated with acute EBV infection may present with seizures, coma, personality changes, distortions of perception, cerebellar ataxia, or focal brainstem or cerebral findings. These complications usually occur 1 to 3 weeks after the onset of clinical infectious mononucleosis, but they have occurred shortly before, during, or after other symptoms of infectious mononucleosis (15,16,17a). Alternatively, they may be the only symptom of acute infection with EBV (6,18,19). Patients usually present with fever and headache progressing to encephalitis over a few days. Most cases occur in older children and young adults.
Generalized seizures, as well as coma and other signs of diffuse encephalopathy, may occur without focal neurologic findings (5,7,15,16). Patients have presented with new onset of seizures and only later have been found by serology to have recent EBV infection (20). EEGs in patients with diffuse encephalopathy show generalized slowing with occasional sharp wave activity, but they may reveal periodic discharges in patients with seizures (20).
Focal neurologic findings in EBV-associated encephalitis include localized seizures, hemiparesis, and unilateral Babinski reflexes. In a large prospective study of encephalitis by the Collaborative Antiviral Study Group, in which focal neurologic findings were required for entry, 2% of patients (8 of 432) were found to have EBV encephalitis (21).
Although EBV encephalitis may involve any area of the brain, the cerebellum is commonly involved. Numerous cases of cerebellitis, usually manifested as acute cerebellar ataxia, have been reported (13,21a). Most patients present with abnormalities of gait. A complete recovery is usual, but severe cases with tonsillar herniation and death have been reported (21b). Other commonly involved areas include the basal ganglia and cerebral hemispheres, with many patients having involvement of multiple areas (21c–21e). Several cases of increased intracranial pressure associated with ischemic lesions of the corpus callosum have been reported, two requiring decompressive craniectomy (17a,21f,22). Encephalitis resulting from EBV infection has been reported as a cause of acute hemiplegia in children and young adults (23). Some patients present with a typical history of infectious mononucleosis followed by psychosis and personality changes. Children with EBV encephalitis may present with metamorphopsia, the so-called “Alice in Wonderland” syndrome, in which affected individuals have perceptual distortions of personal body image, size, and spatial relationships (8,18). Movement disorders indicative of extrapyramidal involvement have been reported. These include cogwheel rigidity and athetosis (24), Parkinson-like syndrome (25,21d,21e), and Sydenham-type chorea (26). Brainstem encephalitis with cranial nerve and long-tract signs (27) and the “locked-in” syndrome have been described. Acute psychosis (28) and transient global amnesia (29) may be the only neurologic manifestation of EBV infection. Unusual complications of EBV encephalitis include acute aqueductal stenosis (30) and the syndrome of inappropriate antidiuretic hormone secretion (31). Reye syndrome, acute fatty degeneration of the liver accompanied by encephalopathy, has followed primary EBV infection in a number of reported cases (32).
Rare cases of relapsing or chronic encephalitis associated with acute EBV infection have been reported. Tolly, Wells, and Sty (33) described a 10-year-old girl with waxing and waning neurologic symptoms associated with EBV infection that occurred over 3 months. Magnetic resonance imaging (MRI) showed rapidly changing CNS lesions that correlated with the fluctuating neurologic examination results (Fig. 12.2).
Myelitis
Spinal cord lesions can accompany encephalitis and present as paraplegia, quadriplegia, or other motor or sensory losses (5,34). The CSF shows a mononuclear pleocytosis with elevated levels of protein, but the glucose level is often normal. Isolated transverse myelitis with sensory and motor loss in the absence of encephalopathy has also been reported (6,9), with viral DNA being detected in the CSF (35,36). Most cases of myelitis occur in older children and young adults and eventually resolve without residua, although several cases in older adults have resulted in long-term sequelae such as muscle weakness and sensory deficits (34).
Cranial and Peripheral Neuritis
Although any of the cranial nerves may be affected during EBV infection, palsies of cranial nerve VII are most common. Numerous cases of unilateral or bilateral Bell palsy have been reported in the setting of acute infectious mononucleosis (5,6,15). With the advent of specific EBV serologic tests, increased numbers of cases of Bell palsy have been attributed to otherwise asymptomatic EBV infection (9). Other forms of cranial nerve involvement include anosmia (37); Fisher syndrome, involving multiple cranial nerves (38); bilateral sensorineural hearing loss (39); unilateral hearing loss with ipsilateral involvement of cranial nerves V and VII (40); vestibular neuritis with oscillopsia; hypoglossal (XII) nerve palsy (41); vocal fold paralysis due to vagal (X) nerve palsy (41); extraocular muscle palsies involving cranial nerves III (42), IV, or VI (6); and acute optic neuritis (15,43). Other ocular complications include papilledema, retrobulbar neuritis, chiasmic neuritis, ptosis, uveitis, episcleritis, and opsoclonus (44,45).
Among peripheral nerves that are affected during EBV infection, the brachial plexus and its branches are most commonly involved. Brachial plexopathy in the setting of infectious mononucleosis usually presents with shoulder pain followed by paralysis of the serratus anterior for weeks to months (7,46). Five patients with lumbosacral radicular plexopathy and one patient with femoral neuropathy were described who had serologic evidence of recent EBV infection (47). Acute autonomic neuropathy has also been reported with acute EBV infection (48).
Guillain-Barré Syndrome
Guillain-Barré syndrome, or acute inflammatory demyelinating polyneuropathy, is characterized by progressive motor weakness of more than one limb and areflexia. Guillain-Barré syndrome usually presents several days to weeks after the onset of infectious mononucleosis, or it may present in patients with otherwise asymptomatic EBV seroconversion. Grose et al. (9) found evidence of acute EBV infection in 12 of 24 patients with Guillain-Barré syndrome. None of these patients had symptomatic infectious mononucleosis before the onset of Guillain-Barré syndrome. Dowling and Cook (49) reported that 8 of 100 patients with Guillain-Barré syndrome had an immunoglobulin M (IgM)–positive test result for EBV, indicative of recent infection. A prospective study found evidence of acute EBV infection in only 2 of 99 patients with Guillain-Barré syndrome, with a similar frequency (2%) in age-matched controls (50). However, the lack of association of Guillain-Barré syndrome with EBV may have been a consequence of the older age of the patients studied, because most older individuals are already seropositive for EBV. A case–control study from the Netherlands found evidence of acute EBV infection in 16 (10%) of 154 patients with Guillain-Barré, compared with 1% of age-matched controls with other neurologic diseases (51).
Epstein-Barr Virus–Associated Central Nervous System Lymphoma
EBV has been associated with CNS lymphomas in patients without any apparent immunodeficiency or, more commonly, in patients with underlying immunodeficiencies. Although some studies of immunologically normal individuals have demonstrated EBV DNA in up to 46% (11/24 patients) of B-cell CNS lymphomas by in situ hybridization (52), most primary CNS B-cell lymphomas in nonimmunocompromised persons do not contain EBV genomes.
EBV-associated CNS lymphomas have been reported in patients receiving solid organ or bone marrow transplants and in patients with leukemia, X-linked lymphoproliferative disease, and acquired immunodeficiency syndrome (AIDS) (53). From 10% to 25% of lymphomas in patients with heart, heart–lung, liver, kidney, or bone marrow transplants involve the CNS and contain EBV genomes (54).
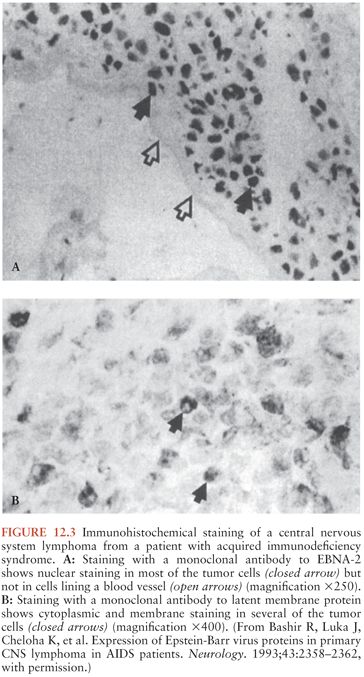
EBV has been detected in virtually 100% of CNS lymphomas in patients with AIDS (54–56). Nearly all EBV-positive lymphomas in human immunodeficiency virus (HIV)–positive patients express the EBV latency-associated proteins EBNA-2 and LMP-1 (57,58) (Fig. 12.3). Viral DNA is present in the lymphoma, not in neuronal cells (55). EBV-associated CNS lymphoma in patients with AIDS occurs more often in patients with very low CD4 cell counts. HIV patients who later developed CNS lymphomas lacked EBV-specific CD4 T cells (58a). CNS lymphomas are more often monoclonal and lack c-Myc translocations when compared with systemic (not involving the CNS) lymphomas in patients with AIDS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree