The diverse medical and neurologic complications of central nervous system (CNS) neoplasms or their treatment cause significant morbidity and mortality. Thus, their recognition and appropriate management by all members of the interdisciplinary team engaged in the care of patients with brain tumors is essential in optimizing quality of life and extending survival. Recognition of the acute, early delayed, and late complications of brain irradiation is essential to optimize management and mitigate their clinical impact.
- •
Recognition and appropriate treatment of complications of brain tumors, including vasogenic edema, venous thromboembolic disease, seizures, and the neurologic complications of radiation therapy, is essential to optimize quality of life and extend survival.
- •
Symptomatic peritumoral edema is treated with dexamethasone, tapered to the lowest dose that optimizes neurologic function, and seizures are treated with a newer antiepileptic drug (eg, levetiracetam) to minimize adverse effects and drug interactions; seizure prophylaxis is not indicated in patients who never had a seizure.
- •
Clinicians must maintain a high index of suspicion for pulmonary embolism or deep venous thrombosis in patients with brain tumors. Most patients with venous thromboembolism can be safely anticoagulated according to consensus guidelines for anticoagulation in patients with cancer, without undue risk of intracranial hemorrhage, obviating the need for inferior vena cava filtration devices.
- •
Complications of radiation therapy encompass diverse pathogenetic mechanisms and neurologic manifestations and are temporally defined as acute (during or shortly after), early delayed (weeks to 4 months), and late (more than 6 months) reactions.
- •
Symptomatic acute and early delayed radiation reactions are managed with corticosteroids; the early delayed reaction may mimic progression of disease (pseudoprogression), but is paradoxically associated with a favorable prognosis and should not lead to premature termination of effective therapy.
Introduction
Patients with central nervous system (CNS) neoplasms are at risk for an array of medical and neurologic complications of their disease or its treatment. These complications represent a significant cause of neurologic and systemic morbidity, and their recognition and appropriate management is essential in optimizing quality of life and extending survival for patients with brain tumors. Peritumoral edema, seizures, and thromboembolic disease are among the most common complications related to the underlying neoplasm, whereas complications of treatment include radiation-related toxicities and the adverse effects of medications, including corticosteroids, antiepileptic drugs, and chemotherapy.
This article discusses the clinical features and management of the common or serious tumor- and treatment-related complications of CNS neoplasms, including peritumoral edema, thromboembolic disease, seizures, and radiation-related toxicities.
Peritumoral edema
Pathophysiology
Cerebral edema is a significant cause of morbidity and mortality in patients with CNS neoplasms. The edema associated with primary and metastatic brain tumors is typically vasogenic, that is, due to increased vascular permeability associated with blood brain barrier (BBB) disruption, rather than cytoxic, that is, hypoxia induced by ischemia or trauma. BBB disruption allows passage of plasma fluid and proteins from the vascular compartment into brain parenchyma, resulting in edema and increased interstitial pressure within and around the tumor. Peritumoral edema correlates with histologic BBB abnormalities, including abnormal tight junctions, fenestrations, thickened basement membrane of the capillary endothelium, and diminished contact between pericytes and astrocytes.
Although the precise mechanism of BBB disruption is not fully understood, the pro-angiogenic peptide, vascular endothelial growth factor (VEGF), plays a central role. VEGF is over expressed and secreted by glial tumors, metastatic tumors, and meningiomas. In pre-clinical models, VEGF stimulates aberrant vascular proliferation and induces the histologic changes in capillary endothelium associated with BBB disruption. Levels of tumor-associated VEGF expression correlate with the grade of glial tumors. Thus, high-grade gliomas (anaplastic astrocytoma, oligodendroglioma, and glioblastoma) and metastatic lesions typically demonstrate peritumoral edema and enhancement on imaging, whereas low-grade gliomas do not.
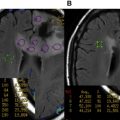
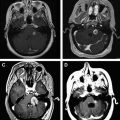
Imaging
Radiographically, disruption of the BBB is associated with contrast enhancement and edema. The most widely used magnetic resonance imaging (MRI) sequences to assess vascular permeability are the post-contrast (gadolinium) T1 sequences, which demonstrate parenchymal enhancement in areas of brain where disrupted BBB does not exclude gadolinium. Edema is best visualized on the noncontrast T2 and fluid-attenuated inversion recovery (FLAIR) sequences. These sequences show hyperintensity in areas of edema that are typically much more extensive than the enhancing area, although hyperintensity may also reflect infiltrative nonenhancing tumor or post-treatment gliosis. Other MRI sequences (diffusion-weighted, dynamic contrast-enhanced) have been explored to distinguish vasogenic edema from infiltrative tumor but have not proven definitive.
Clinical Presentation
At initial diagnosis, most patients with high-grade gliomas or brain metastases present with symptoms related to vasogenic edema. Vasogenic edema exacerbates focal neurologic symptoms related to tumor mass and causes nonfocal symptoms of increased intracranial pressure, including headache, lethargy, and confusion. Patients may experience near syncope or syncope due to “plateau waves” caused by transient increases in intracranial pressure from activities associated with the Valsalva maneuver or upon standing. Progressive, extensive vasogenic edema can lead to herniation and death.
Over the course of their disease, patients with brain tumors often develop symptomatic exacerbations of vasogenic edema. Common causes of increasing edema are steroid withdrawal, radiation effects (discussed later in this article), or tumor progression. Repeat brain imaging usually shows increasing edema and/or contrast enhancement, although it is not possible to distinguish increasing edema caused by tumor progression and pseudoprogression.
Treatment
Corticosteroids have been used to treat vasogenic edema for over 5 decades and are the mainstay of management. On imaging studies, corticosteroids decrease capillary permeability as early as 6 hours and decrease water content of peritumoral brain tissue 48 to 72 hours after administration. The mechanism of action of corticosteroids in stabilizing the BBB is uncertain. Pre-clinical studies suggest that corticosteroids downregulate VEGF and upregulate angiopoietin-1 production in glial tumors via the glucocorticoid receptor.
Corticosteroids are indicated in all patients with symptomatic vasogenic edema. Although there is a paucity of controlled studies, clinical experience over decades has established practice principles guiding the use of corticosteroids as follows : (1) Dexamethasone is preferred because of its relative lack of mineralocorticoid effects and long half-life compared with other corticosteroids, although other corticosteroids have similar efficacy in equipotent doses; (2) once maximum clinical benefit has been achieved with initial dosing, dexamethasone should be tapered slowly to the lowest dose needed to maintain optimum neurologic function; (3) patients must be closely monitored and treated for adverse effects; (4) asymptomatic patients do not require corticosteroids; (5) in the event of impending herniation from mass effect, emergent neurosurgical evaluation for surgical decompression or initiation of osmotherapy is indicated.
Dose, Duration, and Efficacy of Dexamethasone
Dexamethasone is often administered every 6 hours, although its half-life allows twice daily dosing. Intravenous dosing is not required, as oral absorption is excellent. Most patients receive an initial dose of 16 mg daily in divided doses. However, in patients with brain metastases not at risk for herniation, one randomized trial showed no advantage of 16 mg compared with 4 or 8 mg/d, with respect to improving Karnofsky performance status (KPS), whereas toxicities were substantially increased at the higher dose. Thus, in patients with mild symptoms, an initial dose of 4 to 8 mg/d is appropriate; for moderate or severe symptoms, 16 mg/d is recommended.
Most patients with symptomatic vasogenic edema experience an improvement in neurologic symptoms and KPS within hours of initiation of dexamethasone, although maximum benefit is usually not seen for several days. Once maximum clinical benefit is achieved, dexamethasone should be tapered to the lowest dose that optimizes neurologic function or discontinued, if tolerated. A slow taper is advised to avoid rebound edema, especially during radiotherapy. Decrements of no greater than 50% of the previous dose at intervals of no less than every 4 days are recommended. Because radiation may transiently increase vasogenic edema, continuation of dexamethasone during radiotherapy may be necessary.
Adverse Effects of Dexamethasone
The acute and chronic toxicities of corticosteroids are well known. In patients with brain tumors, acute and subacute toxic effects of dexamethasone are common and cause significant iatrogenic morbidity ( Table 1 ). The incidence of toxic effects correlates with the height of the daily dose, duration of treatment, and cumulative total dose. Thus, dexamethasone should be administered in the lowest possible daily dose for the shortest duration needed to optimize neurologic status.
| Systemic | Neurologic |
|---|---|
| Common, not serious | |
| Increased appetite | Insomnia |
| Weight gain | Tremor |
| Fluid retention | Emotional lability |
| Acne | Hiccups |
| Skin fragility, purpura | |
| Serious | |
| Myopathy | Delirium |
| Infections | Psychosis |
| Hyperglycemia, diabetes | |
| Hpokalemia | |
| Potentially life-threatening | |
| Pneumocystis pneumonia | Seizures (drug interactions) |
| GI bleeding | |
| GI perforation | |
In one large series of patients with brain metastases, the incidence of specific adverse effects of dexamethasone (16 mg/d for 7 or 28 days) was as follows: cushingoid facies 65%, proximal weakness 38%, peripheral edema 26%, hypertension 26%, gastrointestinal side effects 24%, mental status changes 21%, hyperglycemia 21%, and infectious complications 9%. The incidence and severity of adverse effects in patients with high-grade gliomas is generally higher than that in patients with metastases because of the longer duration of treatment (mean 4–6 months compared with <2 months). Complications of long-term corticosteroid use (eg, cataracts, glaucoma, osteopenia) are encountered infrequently because of the limited survival of patients with brain tumors requiring chronic dexamethasone.
Steroid-Induced Myopathy
Steroid myopathy is common in patients with brain tumors, causing significant debility in 10% to 40% of patients. In adult patients with primary brain tumors treated with dexamethasone for 2 or more weeks, 10% developed myopathy at a median of 11 weeks (range 4–48 weeks). The onset is subacute, over weeks, and usually not seen before 8 weeks of exposure. Myopathy can occur over a wide range of daily, continuous, and cumulative steroid dosing, although duration of treatment has the greatest impact on incidence. There is a positive correlation between myopathy and cushingoid body habitus and a negative correlation with concomitant use of phenytoin, possibly due to phenytoin-induced hepatic catabolism of dexamethasone.
Steroid myopathy is characterized by nontender, bilateral proximal muscle weakness affecting legs more than arms, with preservation of normal sensation, bowel and bladder function, and deep tendon reflexes. This complication has a significant negative impact on quality of life. All patients with steroid myopathy experience a decline in KPS, and 35% of previously ambulatory patients require assistance with ambulation.
Treatment is challenging, as recovery requires withdrawal or dose attenuation of corticosteroids and may take months. Anecdotal reports suggest that nonfluorinated corticosteroids are less likely to cause myopathy than dexamethasone, and thus, transitioning to prednisone is an option if dexamethasone withdrawal is impossible. Physical therapy is advised, although there are no controlled studies evaluating its efficacy. In patients with progressive or recurrent tumor, the prognosis for recovery is poor, because of inability to taper dexamethasone and tumor-related decline in function.
Pneumocytis Jiorvecci (Carinii) Pneumonia
Pneumocytis jiorveci (carinii) pneumonia (PCP) is a potentially fatal complication of corticosteroid therapy. Although PCP is rare in patients with brain tumors (<2%), the mortality is high (33%–40%). The risk of symptomatic PCP may be greatest as dexamethasone is tapered, but up to 50% of cases have occurred in patients on a stable steroid dose. Because lymphopenia is the major predisposing factor for PCP, the risk is particularly high in patients receiving dexamethasone while undergoing concurrent radiation and temozolomide. Thus, all patients should receive PCP prophylaxis during chemoradiotherapy with temozolomide. In addition, PCP prophylaxis is recommended in patients receiving protracted dexamethasone treatment (>1–2 months) or who have persistent absolute lymphopenia (<500 cells/mm 3 ).
Gastrointestinal Effects
Corticosteroids do not substantially increase the risk of symptomatic gastritis or peptic ulcer disease unless other risk factors are present. Thus, prophylactic therapy in patients on dexamethasone is restricted to those patients who are in the perioperative period, on high doses of dexamethasone (>16 mg/d), on concomitant nonsteroidal antiinflammatory drugs (NSAIDs), or with a history of gastritis or ulcer disease. When prophylaxis is indicated, proton pump inhibitors are recommended, as H2 receptor antagonists do not prevent NSAID-associated gastroduodenal disease.
Perforation of the bowel, especially of colonic diverticula, is a rare but potentially fatal complication in patients receiving corticosteroids. Because steroids can mask the clinical signs of peritonitis, resulting in delays in diagnosis and intervention, bowel perforation must be considered in any patient on high dose or chronic steroids who presents with abdominal pain, fever of unknown origin, or unexplained leukocytosis.
Role of Bevacizumab
Given the central role of VEGF in BBB disruption and vasogenic edema, targeting the VEGF pathway represents a rational corticosteroid-sparing treatment strategy. In preclinical xenograft models of glioblastoma, VEGF pathway inhibitors decrease vascular permeability and normalize tumor vasculature in association with decreased edema. The efficacy of this approach has been demonstrated in phase I/II studies in patients with recurrent glioblastoma treated with the VEGF inhibitor, bevacizumab, or the pan-VEGF receptor inhibitor, cedirinib. These agents dramatically reduce contrast enhancement on T1 sequences and vasogenic edema on T2/FLAIR sequences in most patients, and favorable radiographic changes are associated with clinical benefit, including reduction in dexamethasone dosage. Bevacizumab is approved for treatment of progressive glioblastoma, and in this setting, it is an effective agent for management of peritumoral edema. However, in other clinical settings, the use of bevacizumab or other angiogenesis inhibitors for treatment of vasogenic edema remains investigational.
Peritumoral edema
Pathophysiology
Cerebral edema is a significant cause of morbidity and mortality in patients with CNS neoplasms. The edema associated with primary and metastatic brain tumors is typically vasogenic, that is, due to increased vascular permeability associated with blood brain barrier (BBB) disruption, rather than cytoxic, that is, hypoxia induced by ischemia or trauma. BBB disruption allows passage of plasma fluid and proteins from the vascular compartment into brain parenchyma, resulting in edema and increased interstitial pressure within and around the tumor. Peritumoral edema correlates with histologic BBB abnormalities, including abnormal tight junctions, fenestrations, thickened basement membrane of the capillary endothelium, and diminished contact between pericytes and astrocytes.
Although the precise mechanism of BBB disruption is not fully understood, the pro-angiogenic peptide, vascular endothelial growth factor (VEGF), plays a central role. VEGF is over expressed and secreted by glial tumors, metastatic tumors, and meningiomas. In pre-clinical models, VEGF stimulates aberrant vascular proliferation and induces the histologic changes in capillary endothelium associated with BBB disruption. Levels of tumor-associated VEGF expression correlate with the grade of glial tumors. Thus, high-grade gliomas (anaplastic astrocytoma, oligodendroglioma, and glioblastoma) and metastatic lesions typically demonstrate peritumoral edema and enhancement on imaging, whereas low-grade gliomas do not.
Imaging
Radiographically, disruption of the BBB is associated with contrast enhancement and edema. The most widely used magnetic resonance imaging (MRI) sequences to assess vascular permeability are the post-contrast (gadolinium) T1 sequences, which demonstrate parenchymal enhancement in areas of brain where disrupted BBB does not exclude gadolinium. Edema is best visualized on the noncontrast T2 and fluid-attenuated inversion recovery (FLAIR) sequences. These sequences show hyperintensity in areas of edema that are typically much more extensive than the enhancing area, although hyperintensity may also reflect infiltrative nonenhancing tumor or post-treatment gliosis. Other MRI sequences (diffusion-weighted, dynamic contrast-enhanced) have been explored to distinguish vasogenic edema from infiltrative tumor but have not proven definitive.
Clinical Presentation
At initial diagnosis, most patients with high-grade gliomas or brain metastases present with symptoms related to vasogenic edema. Vasogenic edema exacerbates focal neurologic symptoms related to tumor mass and causes nonfocal symptoms of increased intracranial pressure, including headache, lethargy, and confusion. Patients may experience near syncope or syncope due to “plateau waves” caused by transient increases in intracranial pressure from activities associated with the Valsalva maneuver or upon standing. Progressive, extensive vasogenic edema can lead to herniation and death.
Over the course of their disease, patients with brain tumors often develop symptomatic exacerbations of vasogenic edema. Common causes of increasing edema are steroid withdrawal, radiation effects (discussed later in this article), or tumor progression. Repeat brain imaging usually shows increasing edema and/or contrast enhancement, although it is not possible to distinguish increasing edema caused by tumor progression and pseudoprogression.
Treatment
Corticosteroids have been used to treat vasogenic edema for over 5 decades and are the mainstay of management. On imaging studies, corticosteroids decrease capillary permeability as early as 6 hours and decrease water content of peritumoral brain tissue 48 to 72 hours after administration. The mechanism of action of corticosteroids in stabilizing the BBB is uncertain. Pre-clinical studies suggest that corticosteroids downregulate VEGF and upregulate angiopoietin-1 production in glial tumors via the glucocorticoid receptor.
Corticosteroids are indicated in all patients with symptomatic vasogenic edema. Although there is a paucity of controlled studies, clinical experience over decades has established practice principles guiding the use of corticosteroids as follows : (1) Dexamethasone is preferred because of its relative lack of mineralocorticoid effects and long half-life compared with other corticosteroids, although other corticosteroids have similar efficacy in equipotent doses; (2) once maximum clinical benefit has been achieved with initial dosing, dexamethasone should be tapered slowly to the lowest dose needed to maintain optimum neurologic function; (3) patients must be closely monitored and treated for adverse effects; (4) asymptomatic patients do not require corticosteroids; (5) in the event of impending herniation from mass effect, emergent neurosurgical evaluation for surgical decompression or initiation of osmotherapy is indicated.
Dose, Duration, and Efficacy of Dexamethasone
Dexamethasone is often administered every 6 hours, although its half-life allows twice daily dosing. Intravenous dosing is not required, as oral absorption is excellent. Most patients receive an initial dose of 16 mg daily in divided doses. However, in patients with brain metastases not at risk for herniation, one randomized trial showed no advantage of 16 mg compared with 4 or 8 mg/d, with respect to improving Karnofsky performance status (KPS), whereas toxicities were substantially increased at the higher dose. Thus, in patients with mild symptoms, an initial dose of 4 to 8 mg/d is appropriate; for moderate or severe symptoms, 16 mg/d is recommended.
Most patients with symptomatic vasogenic edema experience an improvement in neurologic symptoms and KPS within hours of initiation of dexamethasone, although maximum benefit is usually not seen for several days. Once maximum clinical benefit is achieved, dexamethasone should be tapered to the lowest dose that optimizes neurologic function or discontinued, if tolerated. A slow taper is advised to avoid rebound edema, especially during radiotherapy. Decrements of no greater than 50% of the previous dose at intervals of no less than every 4 days are recommended. Because radiation may transiently increase vasogenic edema, continuation of dexamethasone during radiotherapy may be necessary.
Adverse Effects of Dexamethasone
The acute and chronic toxicities of corticosteroids are well known. In patients with brain tumors, acute and subacute toxic effects of dexamethasone are common and cause significant iatrogenic morbidity ( Table 1 ). The incidence of toxic effects correlates with the height of the daily dose, duration of treatment, and cumulative total dose. Thus, dexamethasone should be administered in the lowest possible daily dose for the shortest duration needed to optimize neurologic status.
| Systemic | Neurologic |
|---|---|
| Common, not serious | |
| Increased appetite | Insomnia |
| Weight gain | Tremor |
| Fluid retention | Emotional lability |
| Acne | Hiccups |
| Skin fragility, purpura | |
| Serious | |
| Myopathy | Delirium |
| Infections | Psychosis |
| Hyperglycemia, diabetes | |
| Hpokalemia | |
| Potentially life-threatening | |
| Pneumocystis pneumonia | Seizures (drug interactions) |
| GI bleeding | |
| GI perforation | |
In one large series of patients with brain metastases, the incidence of specific adverse effects of dexamethasone (16 mg/d for 7 or 28 days) was as follows: cushingoid facies 65%, proximal weakness 38%, peripheral edema 26%, hypertension 26%, gastrointestinal side effects 24%, mental status changes 21%, hyperglycemia 21%, and infectious complications 9%. The incidence and severity of adverse effects in patients with high-grade gliomas is generally higher than that in patients with metastases because of the longer duration of treatment (mean 4–6 months compared with <2 months). Complications of long-term corticosteroid use (eg, cataracts, glaucoma, osteopenia) are encountered infrequently because of the limited survival of patients with brain tumors requiring chronic dexamethasone.
Steroid-Induced Myopathy
Steroid myopathy is common in patients with brain tumors, causing significant debility in 10% to 40% of patients. In adult patients with primary brain tumors treated with dexamethasone for 2 or more weeks, 10% developed myopathy at a median of 11 weeks (range 4–48 weeks). The onset is subacute, over weeks, and usually not seen before 8 weeks of exposure. Myopathy can occur over a wide range of daily, continuous, and cumulative steroid dosing, although duration of treatment has the greatest impact on incidence. There is a positive correlation between myopathy and cushingoid body habitus and a negative correlation with concomitant use of phenytoin, possibly due to phenytoin-induced hepatic catabolism of dexamethasone.
Steroid myopathy is characterized by nontender, bilateral proximal muscle weakness affecting legs more than arms, with preservation of normal sensation, bowel and bladder function, and deep tendon reflexes. This complication has a significant negative impact on quality of life. All patients with steroid myopathy experience a decline in KPS, and 35% of previously ambulatory patients require assistance with ambulation.
Treatment is challenging, as recovery requires withdrawal or dose attenuation of corticosteroids and may take months. Anecdotal reports suggest that nonfluorinated corticosteroids are less likely to cause myopathy than dexamethasone, and thus, transitioning to prednisone is an option if dexamethasone withdrawal is impossible. Physical therapy is advised, although there are no controlled studies evaluating its efficacy. In patients with progressive or recurrent tumor, the prognosis for recovery is poor, because of inability to taper dexamethasone and tumor-related decline in function.
Pneumocytis Jiorvecci (Carinii) Pneumonia
Pneumocytis jiorveci (carinii) pneumonia (PCP) is a potentially fatal complication of corticosteroid therapy. Although PCP is rare in patients with brain tumors (<2%), the mortality is high (33%–40%). The risk of symptomatic PCP may be greatest as dexamethasone is tapered, but up to 50% of cases have occurred in patients on a stable steroid dose. Because lymphopenia is the major predisposing factor for PCP, the risk is particularly high in patients receiving dexamethasone while undergoing concurrent radiation and temozolomide. Thus, all patients should receive PCP prophylaxis during chemoradiotherapy with temozolomide. In addition, PCP prophylaxis is recommended in patients receiving protracted dexamethasone treatment (>1–2 months) or who have persistent absolute lymphopenia (<500 cells/mm 3 ).
Gastrointestinal Effects
Corticosteroids do not substantially increase the risk of symptomatic gastritis or peptic ulcer disease unless other risk factors are present. Thus, prophylactic therapy in patients on dexamethasone is restricted to those patients who are in the perioperative period, on high doses of dexamethasone (>16 mg/d), on concomitant nonsteroidal antiinflammatory drugs (NSAIDs), or with a history of gastritis or ulcer disease. When prophylaxis is indicated, proton pump inhibitors are recommended, as H2 receptor antagonists do not prevent NSAID-associated gastroduodenal disease.
Perforation of the bowel, especially of colonic diverticula, is a rare but potentially fatal complication in patients receiving corticosteroids. Because steroids can mask the clinical signs of peritonitis, resulting in delays in diagnosis and intervention, bowel perforation must be considered in any patient on high dose or chronic steroids who presents with abdominal pain, fever of unknown origin, or unexplained leukocytosis.
Role of Bevacizumab
Given the central role of VEGF in BBB disruption and vasogenic edema, targeting the VEGF pathway represents a rational corticosteroid-sparing treatment strategy. In preclinical xenograft models of glioblastoma, VEGF pathway inhibitors decrease vascular permeability and normalize tumor vasculature in association with decreased edema. The efficacy of this approach has been demonstrated in phase I/II studies in patients with recurrent glioblastoma treated with the VEGF inhibitor, bevacizumab, or the pan-VEGF receptor inhibitor, cedirinib. These agents dramatically reduce contrast enhancement on T1 sequences and vasogenic edema on T2/FLAIR sequences in most patients, and favorable radiographic changes are associated with clinical benefit, including reduction in dexamethasone dosage. Bevacizumab is approved for treatment of progressive glioblastoma, and in this setting, it is an effective agent for management of peritumoral edema. However, in other clinical settings, the use of bevacizumab or other angiogenesis inhibitors for treatment of vasogenic edema remains investigational.
Thromboembolic disease
Venous thromboembolic disease is a widely recognized complication of malignancy, including primary and metastatic brain tumors. Historically, the risk of tumor-related intracranial hemorrhage (ICH) was considered a strong contraindication to the use of anticoagulation in patients with brain tumors. However, over the past 2 decades, clinical experience and retrospective studies have demonstrated that most patients with brain tumors are safely anticoagulated for venous thromboembolism (VTE), without increased risk of ICH. Thus, current treatment guidelines focus on identifying those patients who have an unacceptable risk of ICH, precluding anticoagulation, and treating all other patients according to consensus guidelines for management of VTE in malignancy.
Pathophysiology, Risk Factors, Incidence
Active malignancy is a recognized risk factor for VTE, and patients with malignant glial tumors have one of the highest rates of cancer-associated VTE, exceeded only by ovarian cancer. Hypercoagulability in patients with malignancy, including brain tumors, derives from complex alterations in homeostatic mechanisms of coagulation and fibrinolysis, related in part to tumor production of procoagulants and fibrinolytic inhibitors. Glioma cells constitutively produce abundant procoagulants, most notably tissue factor and cancer procoagulant. Biochemical evidence of activated coagulation, including elevated D-dimer levels, is often present in patients with glioma. In addition, aberrant fibrinolysis is apparent, with elevated circulating levels of plasminogen activator inhibitor-1, plasminogen, tissue plasminogen activator, and total fibrinolytic activity.
The reported incidence of VTE in patients with malignant glioma is approximately 30%, and up to 20% of patients with brain metastases or primary CNS lymphoma develop symptomatic VTE. The risk is highest in the post-operative period, but persists throughout the course of disease. Additional risk factors include paretic limb, glioblastoma histology, age more than 60 years, large tumor size, length of surgery, immobility, and administration of chemotherapy.
Given the incidence of VTE in patients with brain tumors, clinicians must maintain a high degree of suspicion for pulmonary embolism or deep venous thrombosis in this setting. Subtle respiratory symptoms, unexplained tachycardia or fatigue, or lower extremity edema always warrant consideration of VTE in this high-risk patient population.
Contraindications to Anticoagulation
Although most patients with brain tumor who develop VTE can be safely anticoagulated, there are defined subsets of patients at high risk of ICH in whom anticoagulation is not advised. However, it is important to recognize that contraindications to anticoagulation are relative, and careful assessment of risks and benefits is imperative in decision making in all patients with life-threatening VTE.
Contraindication to anticoagulation in patients with brain tumors is related to the risk of spontaneous symptomatic intratumoral hemorrhage. This risk is low in gliomas and in metastases from most solid tumors (eg, breast, lung, gastrointestinal) (<5%). However, brain metastases from melanoma, choriocarcinoma, thyroid carcinoma, and renal carcinoma have a high risk of spontaneous hemorrhage (up to 70%), and thus, anticoagulation is contraindicated in these 4 diagnoses until the metastases have been definitively treated. Other contraindications to anticoagulation unrelated to tumor type include prior history of ICH, bleeding diathesis including thrombopenia (usually <50,000), or ongoing life-threatening extracranial bleeding.
The incidence of VTE is particularly high in the post-operative period after craniotomy. The decision to anticoagulate is complicated by the uncertain risk of ICH in the post-operative period and must be made in consultation with neurosurgeons. Recent experience using continuous rather than bolus heparin indicates that anticoagulation does not increase the risk of ICH when initiated on post-op day 3 or 5. Importantly, the risk of ICH is high when anticoagulation is initiated less than 48 hours after surgery or exceeds therapeutic levels. Blood products in the resection cavity is a common post-operative finding on imaging and does not necessary preclude initiation of anticoagulation for VTE.
Treatment and Secondary Prevention
In the absence of specific contraindications (as described earlier), VTE in patients with brain tumors should be treated with anticoagulants according to standard consensus guidelines for management of VTE in patients with cancer. Multiple retrospective studies in patients with primary or metastatic brain tumors have shown that anticoagulation with warfarin or low-molecular-weight heparin (LMWH) is safe and not associated with an increased rate of ICH compared with patients without VTE. Placement of an inferior vena cava filter is a suboptimal intervention because of the high rate of recurrent VTE after filter placement alone, exceeding 60% in one series, and is appropriate only in patients in whom anticoagulation is contraindicated.
The need for neuroimaging to rule out occult brain metastases in patients with systemic cancer before initiation of anticoagulation is debated. In patients whose tumors are associated with a high risk of spontaneous hemorrhage (melanoma, renal, thyroid, choriocarcinoma), a pre-treatment noncontrast computed axial tomography scan or magnetic resonance imaging (MRI) is recommended, whereas the need for imaging with other diagnoses, in the absence of neurologic symptoms, is uncertain. In patients with known treated brain tumors (metastatic or primary), the need for a screening scan is also uncertain, in the absence of new neurologic symptoms.
Fixed dose of LMWH is the preferred agent for both initial therapy and long-term treatment. The use of LMWH simplifies initial management and facilitates outpatient treatment in suitable patients. For long-term anticoagulation, LMWH is more effective than warfarin in reducing risk of recurrent VTE in patients with malignancy, albeit with no overall survival benefit, and the risk of hemorrhage with LMWH is the same or reduced compared with warfarin. Based on these observations, LMWH is recommended for long-term anticoagulation of VTE in patients with brain tumors, although it has not been directly compared with warfarin specifically in this patient population. In addition to its superior efficacy, LMWH has the added advantage of absence of drug interactions or need for regular monitoring. In patients who do not tolerate daily injections, warfarin is an acceptable alternative, with the caveat that overanticoagulation may increase the risk of ICH. The optimum duration of anticoagulation after VTE is unresolved. However, because the risk of recurrent VTE after withdrawal of anticoagulation remains high in patients with active malignancy, indefinite anticoagulation is generally recommended in patients with brain tumors.
The use of bevacizumab in patients with primary or metastatic brain tumors has raised concerns about the safety of anticoagulants and concomitant bevacizumab. One series suggested no significant ICH in glioma patients treated with LMWH and bevacizumab. However, until more data are available, bevacizumab should be used with caution in patients with brain tumors requiring anticoagulation.
Primary Prevention
Despite the high incidence of VTE in patients with malignant glioma, an extended course of prophylactic LMWH beyond the immediate post-operative period is not recommended. Long-term primary VTE prophylaxis with LMWH was evaluated in a placebo-controlled trial in patients with newly diagnosed malignant gliomas. Although there was a nonsignificant decrease in VTE incidence with LMWH, there was an increase in ICH events and no difference in overall survival.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree