Abstract
Epidemiologic studies demonstrate that, overall, pregnancy is associated with a reduced lifetime risk of developing breast cancer. Yet this protective effect is not constant or immediate. Although uncommon, the development of breast cancer during the gestational or lactational period has traditionally been attributed a poor prognosis. With a tendency to delayed childbearing, an increase in the incidence of pregnancy-associated breast cancer is possible.
This review outlines a tailored approach to the evaluation, diagnosis, and management of breast cancer during pregnancy. The majority of breast masses during pregnancy are benign, but the index of suspicion for cancer must be high for women who present with a breast mass during this period. Ultrasound and core biopsy are the fundamental diagnostic means. Many of the management strategies mirror those used in the treatment of breast cancer outside of pregnancy, with some important differences. Surgery and systemic chemotherapy, either in the neoadjuvant or adjuvant settings, are feasible options for most women during pregnancy. Chemotherapy is contraindicated in the first trimester of pregnancy, but after this, dose-dense regimens, including anthracyclines and taxanes, have been used with limited risk for both the mother and the fetus. Where patient and tumor factors allow, breast-conserving surgery followed by postpartum radiotherapy is appropriate. For axillary staging, the radiocolloids used for sentinel node mapping are safe to use given the locoregional administration.
Recent advances have improved oncologic outcomes in patients with breast cancer, but not all of these have been adapted for pregnant patients. With serious adverse events on both the pregnancy and fetus, prolonged exposure to trastuzumab should be avoided. Further research, potentially through case registries with rigorous follow-up, is required to evaluate outcomes with pregnancy-associated breast cancer.
Keywords
breast cancer, pregnancy, gestational breast cancer, chemotherapy
Pregnancy-associated breast cancer is defined as the diagnosis of breast cancer during the gestational period, within 1 year of pregnancy or anytime during lactation. It is the second most common malignancy occurring in pregnancy, after carcinoma of the cervix. The incidence of pregnancy-associated breast cancer is 1.3 to 3.7 per 10,000 deliveries. The estimated probability of developing breast cancer within the next 10 years is 1 in 225 for a woman 30 years of age, increasing sharply to 1 in 69 for a woman 40 years of age. The median age at diagnosis of breast cancer in pregnancy is 33 years.
Epidemiologic studies have shown that pregnancy is associated with a reduced lifetime risk of developing breast cancer. However, this protective effect is neither immediate nor constant. These studies have shown that the greatest degree of protection is conferred by pregnancy at a younger age. As women delay childbearing for a variety of personal and professional reasons, the possibility of encountering the diagnosis of breast cancer occurring during pregnancy increases. A transient increase in breast cancer risk seen after pregnancy is more conspicuous in women with late age at first birth.
The diagnosis and treatment of breast cancer during pregnancy encompasses many diagnostic and therapeutic dilemmas, and the input from a multidisciplinary team is of paramount importance for therapeutic planning during this difficult time.
Prognosis and Historical Perspective
Reports of outcomes after treatment for pregnancy-associated breast cancer from the early decades of the 20th century were dismal. Five-year survival rates of 17% were reported by Kilgore and Bloodgood in 1929, and of 15% by Harrington and coworkers in 1937.
Over the next several decades, published studies began reporting variations in outcomes stratified by differences in nodal status at presentation. More than 70% of patients with pregnancy-associated breast cancer in these studies presented with axillary nodal metastases. The prognosis associated with pregnancy-associated breast cancer was worse overall, both in node-positive and node-negative patients.
Studies in the 1980s and 1990s were mostly single institution and retrospective that collected patients over several decades. These case-control studies compared pregnancy-associated breast cancer cases with nonpregnant controls. When these patients were grouped by stage, there was no statistical difference identified between pregnant and nonpregnant patients. Petrek and colleagues compared 56 stage I–III pregnancy-associated breast cancers with nonpregnant controls treated between 1960 and 1980. Sixty-one percent of the patients with pregnancy-associated breast cancer had positive nodes, compared with 38% of the nonpregnant controls. Overall, 5-year survival for node-negative patients was identical for both groups at 82%. All patients had a radical or modified radical mastectomy. For node-positive patients, the 5-year overall survival of 47% for pregnancy-associated breast cancer was not statistically inferior to the 59% seen in nonpregnant patients. A delay in diagnosis because of pregnancy is thought to play an important factor in the late stage at presentation of many of these patients, thus accounting for the worse prognosis.
However, both meta-analyses and data from national cancer registries point toward a poorer prognosis for patients with pregnancy-associated breast cancer. A 2012 meta-analysis incorporated studies from 1969 to 2009 and—as expected given the disparate definitions, matching criteria, and outcome reports—significant heterogeneity was noted in the pooled analyses. After a series of adjustments, an estimated hazard ratio of 1.4 was calculated for the negative effect of pregnancy on overall survival. On subgroup analysis, patients diagnosed in the postpartum period had a clearer trend toward worse overall survival. Reports from US and Swedish cancer studies bolster this finding, as both identified that patients with a diagnosis of breast cancer within 1 year of giving birth had a lower overall survival. Neither of these studies adjusted for differences in tumor subtypes.
More recent studies, including a large international registry of German and Belgian patients, provide some grounds for optimism. With contemporary multimodality therapy, when adjusted for stage, patients with pregnancy-associated breast cancer did not have a worse prognosis than age- and stage-matched nonpregnant patients. This cohort of 311 patients reported a 5-year overall survival of 78%.
Diagnostic Evaluation and Staging During Pregnancy
During pregnancy, the breasts undergo physiologic hypertrophy and proliferative changes in response to high levels of estrogen and progesterone that stimulate and prepare the breast for lactation. These changes mean that physical examination of the breasts becomes gradually more difficult as the pregnancy progresses due to increases in both breast mass and density. These changes continue into the postpartum period in women who are breastfeeding. The ideal time for a thorough examination of the breasts is during the first trimester when the breasts have undergone the least change. Any abnormality encountered should be promptly evaluated at this time.
Delays in diagnosis are thought to play a significant role in pregnancy-associated breast cancers, and the often late stage at diagnosis that is encountered. A multiinstitutional study of 192 patients in Japan found that the average time from symptom development to diagnosis was just over 6 months, 1 month longer than in a series of age-matched controls. In keeping with other reports, patients with pregnancy-associated breast cancer had larger primary tumors and a higher burden of axillary nodal disease compared with the nonpregnant patients. These characteristics all contributed to an overall worse prognosis in patients diagnosed during pregnancy or lactation. Contemporary reports continue to point to delays in presentation as a common occurrence in pregnancy-associated breast cancer. These delays can be on the part of the patient not bringing a palpable mass to medical attention or on the part of the physician due to a reluctance to proceed with imaging and biopsy during pregnancy for fear of complications.
Imaging Studies During Pregnancy
The index of suspicion for cancer must be high for women who present with a breast mass during the gestational or lactational period. The majority of these breast lumps will prove benign. The differential diagnoses encompass a spectrum of benign and lactating entities, including, but not limited to, fibroadenoma, lactating adenoma, galactocele, cystic disease, lobular hyperplasia, breast abscess, and lipoma.
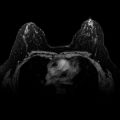
Mammograms are typically not obtained during pregnancy despite the fact that the average glandular dose to the breast for a two-view mammogram of 0.4 HmSv equates to a negligible radiation exposure to the developing fetus. The radiation exposure to the fetus can be further reduced by up to 50% by abdominal lead shielding. However, the increased parenchymal density of the breasts that accompanies the pregnant state reduces the sensitivity of mammography. Mammography may be useful in determining the extent of disease including multifocality and multicentricity and should be considered in any patient with a highly suspicious mass seen on ultrasound or when a diagnosis of pregnancy-associated breast cancer has been made. Lactating patients should be encouraged to nurse or express immediately before mammography to decrease parenchymal density related to retained milk products. Ultrasound is more sensitive than mammography in evaluation of a solid mass in pregnancy or lactation and should be the first modality used in evaluating a pregnant or lactating patient who presents with a breast mass. Ultrasound in this setting has a high reported negative predictive value for exclusion of malignancy and also allows for prompt biopsy of any suspicious lesions identified.
Although magnetic resonance imaging (MRI) has been used in the obstetric patient both for fetal imaging and for evaluation of maternal conditions such as appendicitis, its reported use for breast evaluation in pregnancy is limited. Breast MRI requires contrast-enhanced imaging with gadolinium. The use of gadolinium contrast agents is avoided during pregnancy because of the potentially long half-life in the fetus, its association with teratogenicity in animal studies, and the paucity of data on its safety in pregnancy. Its use may be considered in women who are postpartum, even if lactating, at the time of diagnosis if it is felt that additional information beyond that provided by mammography and ultrasound is required. The American College of Radiology guidelines do not require that patients discontinue breastfeeding. Images obtained on MRI may be difficult to interpret during the pregnant or lactating state. Increased enhancement from hypervascularity may pose a challenge when trying to differentiate lactational changes from suspicious findings.
Once the diagnosis of breast cancer has been made, many routine systemic staging studies use ionizing radiation. The most sensitive period for radiation-associated malformations is in the first 8 weeks of the pregnancy (organogenesis). As noted earlier, pregnancy-associated breast cancer tends to present at a later stage, but the indications for systemic staging should follow National Comprehensive Cancer Network guidelines as for nonpregnant patients. Patients with clinical stage III (cT3N1 or any ≥ N2) or stage IV disease or symptoms suggestive of distant metastases should prompt a systemic evaluation. The risks and benefits of obtaining these imaging examinations during pregnancy need to be carefully evaluated.
Chest x-rays are considered to be safe during pregnancy because the dose with abdominal lead shielding is relatively low. Chest or abdominal computed tomography (CT) scans are generally avoided because of the large cumulative radiation dose. Although less sensitive than MRI or CT, ultrasound is a safe first-choice modality for liver imaging in the pregnant patient. If brain metastases are suspected, MRI is the most sensitive imaging technique. Bone remains the most common site of breast cancer metastases. Alkaline phosphatase levels increase during normal pregnancy and cannot be used as an indicator of bone metastases. Bone scintigraphy is reported as safe during pregnancy and is associated with a 0.02-cGy dose of radiation exposure to the fetus. Modifications of the technique, including adequate maternal hydration, that result in a lower fetal radiation exposure have been described. The use of positron emission tomography (PET) in pregnancy is very limited. Estimates of fetal radiation dose from 18 F fluorodeoxyglucose ( 18 F-FDG) have been provided, but there is no evidence to support its use. The amounts of 18 F-FDG excreted in breast milk after a PET scan are low, and guidelines would suggest the only adjustments that a nursing mother should make after a PET scan are to avoid close contact with the infant for up to 12 hours.
Breast Biopsy During Pregnancy
Any breast mass during pregnancy that is suspicious on either clinical or ultrasound evaluation requires biopsy. Core biopsy is the most accurate means of establishing a diagnosis. These biopsies can be performed under local anesthesia with subcutaneous lidocaine, and patients should be reassured that this has no known harmful fetal effects. The formation of a milk fistula after core needle biopsy has been reported, but the literature contains only sporadic case reports, and it would therefore appear that the overall rate of milk fistula formation is low. The risk is higher with an open surgical biopsy and for more centrally placed lesions.
Fine-needle aspiration (FNA) can be used for the diagnostic evaluation of a breast mass in pregnancy. However, reports have highlighted the difficulties of interpreting the cytologic findings. There are potential pitfalls in the cytologic interpretation of even physiologic changes in the breast. Because of the increased cellularity and frequent mitosis that can be seen accompanying pregnancy, it is important to have an experienced cytopathologist who is familiar with the cytologic appearances of physiologic changes of breast in pregnancy. One study of 214 aspirates from pregnant or lactating women noted that none of the patients with a benign biopsy developed cancer in the follow-up period of 1.5 to 2 years. All cases of cancer on cytology were confirmed on surgical excision.
In the postpartum period, risks of milk fistula formation, bleeding, and infection can be minimized by the cessation of breastfeeding before the biopsy, prophylactic antibiotics, and ensuring adequate hemostasis.
Pathologic Findings
As in nonpregnant women, the majority of pregnancy-associated breast cancers are invasive ductal carcinomas. Clinically, women with pregnancy-associated breast cancer are more likely to have larger tumors and present with axillary nodal metastasis. Pregnancy-associated breast cancers exhibit a range of pathologic features that underline their propensity for a more aggressive course. These tumors are frequently of high nuclear grade (approximately 50%) and exhibit lymphovascular invasion (LVI); more than 60%).
The receptor profile also differs with a shift toward tumors that are estrogen and progesterone receptor negative. It should be acknowledged that breast cancers in younger women who are not pregnant also exhibit many of these unfavorable pathologic characteristics such as high grade and hormone receptor negativity. Two retrospective, national case-control studies from France and Japan have included age-matched controls. The cumulative rate of estrogen receptor negative tumors in the pregnancy-associated breast cancer patients was 55% compared with 40% in the nonpregnant patients. Both studies also found consistently lower rates of progesterone receptor positivity in pregnancy-associated breast cancer. Only a handful of studies have examined human epidermal growth factor receptor 2 (HER2) positivity in women with pregnancy-associated breast cancer. The average rate of HER2 positivity in eight recent reports with a total of 275 patients with pregnancy-associated breast cancer is 31%. This is almost identical to the 32% HER2 positivity reported in a 2013 International Registry study that included 311 pregnant patients. These studies have not included age-matched controls, so no adequate conclusions can be reached regarding whether HER2 positivity is more prevalent in pregnancy-associated breast cancer. Most recent case series have not found an increase in the rate of inflammatory breast cancer in pregnant or lactating patients.
A full family history is an important part of assessment for these patients. Given the aforementioned tendency toward estrogen receptor–negative disease in a young age group, genetic counseling should certainly be offered to patients with a pregnancy-associated breast cancer. The probability of detecting a germline mutation in a young patient with a triple-negative breast cancer is approximately 20%.
Treatment
Surgery
Historically, mastectomy was considered the standard surgical procedure for the local management of pregnant patients with breast cancer. However, mastectomy is not mandatory, and when appropriate patient and tumor factors are taken into consideration, breast-conserving therapy may be appropriate if lumpectomy is performed in the third trimester and radiotherapy is given postpartum. A delay in postoperative radiotherapy has been associated with increases in local recurrence in nonpregnant patients, and thus lumpectomy in the first or early second trimester with long delays to radiotherapy are often not advised. Recent commentary has suggested that because the majority of these patients will receive chemotherapy—some in the neoadjuvant setting—incorporation of this time period may allow consideration of breast conservation for patients in the second trimester without a delay to radiotherapy if the patient is being treated with neoadjuvant chemotherapy. In patients in the third trimester or those who are postpartum, this potential delay to radiotherapy is not an issue. Therefore a breast-conserving operation is an option if the same factors that determine suitability for breast-conserving therapy in nonpregnant patients apply, such as tumor size, tumor location, and tumor-to-breast–size ratio as well as adjuvant therapy. A number of small studies support the safety and feasibility of breast conservation in terms of local control.
General anesthesia during pregnancy is of concern because of the physiologic changes that accompany pregnancy in the later stages of pregnancy. General anesthesia has not been reported to increase the risk of congenital anomalies in published reports. Spontaneous abortion has been reported in women undergoing surgery in the first and early second trimesters of pregnancy. All general anesthetic drugs cross the placenta. The anesthetic management of pregnant patients requires a balanced consideration of both maternal and fetal physiology, as well as pharmacology. Avoidance of maternal hypoxia or hypotension are key tenets in ensuring a favorable outcome for both mother and fetus.
In nonpregnant patients, sentinel lymph node biopsy (SLNB) is the gold standard axillary staging procedure. Recent studies suggest SLNB can be performed safely for both the mother and the fetus. The use of isosulfan blue dye in pregnancy (a US Food and Drug Administration category C drug) as a mapping agent is not recommended because of the low but potentially very harmful underlying risk of a maternal anaphylactic reaction as well as very limited data on potential teratogenic effects of isosulfan blue.
Although the radiocolloids used for sentinel node mapping do emit a radiation dose, the administration of the agent is locoregional as opposed to systemic. Studies have demonstrated that the doses absorbed by the fetus are less than the National Council on Radiation Protection and Measurements limit for a pregnant woman. It is advisable to inject the technetium radiocolloid on the morning of surgery to minimize the exposure to radiation. A number of studies have demonstrated accurate and safe lymphatic mapping in pregnant patients with the use of 99m-Tc, including the description of a low-dose technique for lymphoscintigraphy.
In patients who are deemed node positive preoperatively, on the basis of either clinical assessment or ultrasound, an axillary lymph node dissection should be performed.
To date, only one report has documented short-term outcome with immediate breast reconstruction after mastectomy in pregnancy-associated breast cancer. No major surgical complications were noted in 13 patients who underwent a two-stage procedure with tissue expander insertion. In all cases, the final implant exchange took place after delivery and completion of adjuvant chemotherapy and radiotherapy. The authors concluded that it was best to allow a longer time (median 15 months) from insertion to final implant exchange. In that manner, it enabled the size and shape of the contralateral breast to stabilize, and 7 of the 13 patients underwent a contralateral symmetrizing procedure at the time of implant exchange.
Systemic Chemotherapy
Many of the agents used for the systemic treatment of breast cancer in nonpregnant women are safe to administer after the first trimester of pregnancy. Systemic chemotherapy for primary breast cancer is typically recommended in premenopausal women with node-positive breast cancer or when the primary tumor size is larger than 1 cm. Therefore a large number of women with pregnancy-associated breast cancer would qualify for adjuvant systemic therapy. The decision for chemotherapy should be taken based on the tumor biology and prognostic factors taken into consideration in nonpregnant patients.
Although administering chemotherapy during pregnancy may trigger concerns, the clinician should caution the patient against delaying therapy, especially in cases of locally advanced or poor-prognosis breast cancer, as delays in starting chemotherapy are associated with significantly worse outcomes.
Pregnant women receive weight-based doses of chemotherapy that are similar to the doses received by women who are not pregnant. There is little published information on specific pharmacokinetics of cytotoxic agents in the pregnant patient. A number of physiologic changes of pregnancy, such as increased blood volume coupled with brisker renal and hepatic clearance, may be anticipated to reduce effective drug concentrations. Reduced albumin levels may increase the levels of the unbound drug, an effect that may be offset by the actions of estrogen increasing other plasma proteins. The absorption of orally administered drugs may be affected by the decreased gastric motility that accompanies pregnancy.
The use of chemotherapy is contraindicated in the first trimester of pregnancy due to a well-established higher risk of fetal malformations. This critical period of organogenesis carries the greatest risk for development of congenital abnormalities, chromosomal abnormalities, stillbirth, and miscarriage. The reported rate of major malformations in the general population is 3%. The studies that have recorded outcomes after first trimester exposure to chemotherapy have estimated the rate fetal malformation between 14% and 18%. Initiation of chemotherapy should not be before 14 weeks gestation.
Chemotherapy in the second or third trimester is associated with a risk of fetal malformation of less than 2%, the same as population norms, but is still linked to other adverse outcomes such as intrauterine growth restriction, prematurity, and low birth weight.
Anthracyclines, cyclophosphamide, and taxanes are the standard adjuvant or neoadjuvant combinations used in nonpregnant patients. The most commonly used regimens in pregnant women with breast cancer are doxorubicin plus cyclophosphamide (AC) or 5-fluorouracil, doxorubicin, and cyclophosphamide (FAC). The limited studies of administration of chemotherapy in the second and third trimesters suggest that the major cause of undesirable fetal outcome appears to be from premature delivery rather than from a direct chemotherapy effect. Hahn and colleagues reported a study of 57 pregnant breast cancer patients treated with FAC in the adjuvant (n = 32) or neoadjuvant (n = 25) setting. All patients who delivered had live births with follow-up identifying one child with Down syndrome and 2 with congenital anomalies (club foot; congenital bilateral ureteral reflux). Of 162 exposures to doxorubicin across a number of cancers, including some in the first trimester, complications included preeclampsia, midtrimester miscarriage, and transient neonatal neutropenia with sepsis and intrauterine growth restriction. Doxorubicin is favored over other anthracyclines such as epirubicin that have been associated with neonatal cardiotoxicity ( Table 78.1 ).
| Author | Year | Country | No. of Patients | Regimens Used | Patients Treated With NACT, % | Median Gestation at Start of Chemotherapy | Median No. of Cycles | Median GA at Delivery (Weeks) |
|---|---|---|---|---|---|---|---|---|
| Ring | 2005 | UK | 24 | AC (46%), EC, CMF | 30% | 20 | 6 | 37 |
| Hahn | 2006 | US | 57 | FAC | 44% | 23 | 4 | 37 |
| Azim | 2008 | Italy | 26 | Anthracycline Most E | 35% | Second trimester | 4 | 35 |
| Peccatori | 2009 | Italy | 20 | Epirubicin | 0% | 19 | 12 | 35 |
| Cardonick | 2010 | US, Europe, Australia | 120 | AC (59%) Others: FAC, FEC, single-agent T | 23% | 20 | 4 | 36 |
| Meisel | 2013 | US | 74 | AC (8% with T) | 22% | 81% second trimester | 4 | 56% <37 |
| Amant | 2013 | Europe | 311 | 47% T | 32% | — | — | — |
| Murphy | 2012 | US | 99 | 83% anthracycline 66% T | — | — | — | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree