Abstract
Bisphosphonates are osteoclast inhibitors used to treat osteoporosis. In oncology, bisphosphonates are used to prevent or treat skeletal-related events such as pathologic fractures and hypercalcemia of malignancy. In early breast cancer, these drugs have been used to prevent or treat bone loss associated with the use of aromatase inhibitors. It is thought that bisphosphonates also exert an anticancer effect by altering the tumor microenvironment in the bone. Individual clinical trials of adjuvant bisphosphonates were inconclusive, although few of these trials generated the hypothesis that such an anticancer effect is limited to postmenopausal women. An individual patient-level data meta-analysis of 26 clinical trials including 18,766 women with early breast cancer, treated with bisphosphonates or control, found borderline significant reductions with the use of bisphosphonates for distant recurrence, bone recurrence, breast cancer mortality, and all-cause mortality. A subgroup analysis noted lack of benefit in premenopausal women. In postmenopausal women, there were significant reductions in bone recurrences and breast cancer mortality. Therefore all postmenopausal women (natural or induced), especially those on antiestrogen therapy, should be considered for adjuvant bisphosphonate treatment, and decision to treat should be individualized.
Keywords
postmenopausal, bisphosphonates, clodronate, ibandronate, zoledronate, meta-analysis
Bisphosphonates inhibit osteoclast-mediated bone resorption. As a result, bisphosphonates have several therapeutic roles. Primarily, they were used as an antiosteoporosis medications. Later these drugs were used to prevent or delay skeletal-related events such as fractures and bone pain in patients with metastatic cancers with disease in bones. Bisphosphonates are also used to prevent bone loss associated with aromatase inhibitors, which are used for adjuvant management of breast cancer in postmenopausal women and result in bone loss and hastened osteoporosis. Therefore in breast oncology, bisphosphonates are important supportive care medications in two indications: prevent or delay skeletal-related events in metastatic breast cancer involving bones, and prevent or treat aromatase inhibitor-induced bone loss.
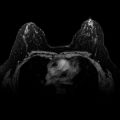
Bone is the commonest site of distant metastatic disease in breast cancer. Tumor microenvironment plays an important role in cancer proliferation. Bisphosphonates alter the bone microenvironment and may have an anticancer effect. Backed by preclinical studies that showed such an effect, secondary analyses of several adjuvant bisphosphonate clinical trials were conducted. In this chapter, we summarize these clinical trials ( Table 57.1 ) and discuss the findings of an individual patient-level data meta-analysis aimed to evaluate the anticancer role of adjuvant bisphosphonates.
| Study Details | Study Population | Study Arms | Primary End Point | Conclusions |
|---|---|---|---|---|
| Clodronate 1600 mg PO | ||||
| Diel et al. 1998 | Pre and postmenopausal (n = 302) a | Clodronate vs. standard care for 2 y | Incidence of distant metastasis | At 3 y of follow-up, distant metastases rate was 13% in clodronate group vs. 29% in control group ( p < .001) |
| Powles et al. 2002 | Pre and postmenopausal (n = 1069) | Clodronate vs. placebo for 2 y | Incidence of bone metastasis | At 6-y follow-up, there was no difference in bone metastasis rates between the two groups |
| Saarto et al. 2004 | Pre and postmenopausal b (n = 299) | Clodronate vs. standard care for 3 y | Not specified | At 10-y follow-up, disease-free survival was lower in clodronate group vs. control ( p = .01) |
| Paterson et al. 2012 NSABP B-34 trial | Pre- and postmenopausal (n = 3323) | Clodronate vs. placebo for 3 y | DFS | At 7.5-y follow-up, there was no difference in DFS between two groups; subgroup analyses found benefit in older patients (≥50 y) with the secondary end points such as DFS and bone metastasis–free interval favoring clodronate arm of the study |
| Ibandronate 50 mg PO | ||||
| Von Minckwitz et al. 2013 GAIN study | Pre- and postmenopausal (n = 2994) c | Ibandronate vs. standard care for 2 y | DFS | At 3-y follow-up, there was no difference in DFS between two groups |
| Zoledronate 4 mg IV | ||||
| Gnant et al. 2015 ABCSG-12 study | Premenopausal (n = 1803) d | Zoledronate vs. standard care for 3 y | DFS | Final analysis after 8-y follow-up, showed improvement in DFS with the use of zoledronate ( p = .042). These results were statistically significant at 5-y follow-up as well |
| Brufsky et al. 2012 Z-FAST trial | Postmenopausal (n = 602) | Zoledronate: upfront vs. delayed for 5 y e | BMD f | At 5-y follow-up, disease recurrence or death rates were similar between the upfront vs. delayed groups (9.8% vs. 10.5%; p = .63) g |
| Coleman et al. 2013 ZO-FAST trial | Postmenopausal (n = 1065) | Zoledronate: upfront vs. delayed for 5 y e | BMD f | At 5-y follow-up, upfront group had a decrease in incidence of DFS events vs. delayed zoledronate group ( p = .0375) |
| Coleman et al. 2014 AZURE trial | Pre- and postmenopausal (n = 3360) h | Zoledronate vs. standard care for 5 y i | DFS | At 5 y, there was no difference in DFS between the two groups ( p = .30); zoledronate reduced the incidence of bone metastases and improved DFS in postmenopausal women |
a All patients had tumor cells in bone marrow.
b Approximately 50% of patients received adjuvant chemotherapy.
c All patients received adjuvant chemotherapy.
d All patients received goserelin to suppress ovarian function, approximately 5% of patients received adjuvant chemotherapy.
e Delayed therapy was initiated when patient become osteopenic or develops pathologic fracture or has an asymptomatic vertebral fracture.
f Change in lumbar spine BMD, DFS was secondary end point.
g Approximately 25% of patients in the delayed group received zoledronate by 5 years.
h Approximately 95% patients received chemotherapy.
i Zoledronate 4 mg intravenous was given every 3 to 4 weeks for six cycles, then every 3 months for eight doses, followed by every 6 months for five cycles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree