The optimal treatment of anaplastic gliomas is controversial. Options for treatment include radiation, chemotherapy or a combination of modalities. This article describes how treatment algorithms for anaplastic gliomas have evolved and interprets the results of recent studies. The available evidence indicates that patients can be treated with either chemotherapy or radiation as initial therapy, with use of the other treatment modality at relapse. Whether subpopulations exist for whom one treatment modality is superior to the other at initial diagnosis must be studied prospectively.
- •
Anaplastic gliomas have a unique natural history compared with glioblastomas and low-grade gliomas, but have historically been grouped together with either of these tumor types in treatment studies.
- •
Survival differences exist between anaplastic astrocytomas and anaplastic oligodendrogliomas, which are caused by the differing molecular features of these tumors.
- •
Current evidence indicates that there is no benefit to radiotherapy with concurrent or adjuvant chemotherapy in patients with anaplastic gliomas.
- •
Initial treatment with chemotherapy or radiation alone is an appropriate treatment strategy, and temozolomide is the first-line chemotherapy agent. The other treatment modality should be used when relapse occurs.
Introduction
Background
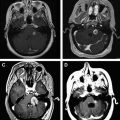
Anaplastic gliomas comprise World Health Organization (WHO) grade III astrocytomas, oligodendrogliomas, and oligoastrocytomas (referred to as mixed gliomas). Typical microscopic features of anaplastic gliomas include moderate hypercellularity, moderate cellular and nuclear pleomorphism, increased mitotic activity, and microvascular proliferation without necrosis. These features are in contrast with WHO grade II gliomas, which are low in mitotic activity, and WHO grade IV gliomas, referred to as glioblastomas, which show vascular proliferation and necrosis.
In most studies conducted before the year 2000, anaplastic gliomas were grouped with glioblastomas as high-grade gliomas or malignant gliomas. Patients with glioblastoma typically comprise most of the patients in these studies, causing difficulty in the interpretation of treatment results. Some studies have also grouped anaplastic gliomas as a single entity. However, it is now evident that anaplastic astrocytomas have a distinct prognosis compared with anaplastic oligodendrogliomas and mixed gliomas, which are more susceptible to chemotherapy and radiotherapy. In addition to tumor grade and histologic type of anaplastic glioma, other prognostic indicators of survival include patient age at diagnosis and the Karnofsky Performance Score (KPS) of the patient.
Although a widely accepted standard of care currently exists for the initial treatment of glioblastomas, the optimal treatment of anaplastic gliomas remains controversial. Options for treatment include radiotherapy, which is currently used in most patients diagnosed with an anaplastic glioma, as well as chemotherapy or a combination of modalities ( Table 1 ). This article describes how treatment algorithms for anaplastic gliomas have evolved and reviews the recent studies that have established the current standard of care.
| Author | Study Year | Tumor Type | Number of Patients | Initial Therapy | OS | P Value |
|---|---|---|---|---|---|---|
| Walker et al | 1980 | AG | 94 | RT | 9 | — |
| 92 | RT + BCNU | 12.75 | P = .108, vs RT alone | |||
| 91 | RT + MeCCNU | 10.5 | P = .668, vs RT alone | |||
| Cairncross et al RTOG 9402 | 2006 | AO | 142 | RT | 56.4 | — |
| 147 | RT + PCV | 58.8 | P = .26 | |||
| van den Bent et al EORTC 26951 | 2006 | AO | 183 | RT | 30.6 | — |
| 185 | RT + PCV | 40.3 | P = .23 | |||
| Wick et al NOA-04 | 2009 | AG | 139 | RT | 72.1 | — |
| 135 | PCV or TMZ | 82.6 | P = NS | |||
| Lassman et al | 2011 | AG | 200 | RT | 52.8 | — |
| 528 | RT + PCV or TMZ | 85.2 | P <.0001, vs RT alone | |||
| 201 | PCV or TMZ | 84 | P = .0008, vs RT alone |
Molecular Features
Important molecular differences exist between anaplastic astrocytomas and anaplastic oligodendrogliomas. Mixed gliomas typically share features of anaplastic oligodendrogliomas, as well as having a better prognosis compared with anaplastic astrocytomas. Important molecular features include 1p/19q codeletion, isocitrate dehydrogenase mutations (IDH1/IDH2), and O 6 -methylguanine-DNA-methyltransferase (MGMT) promoter methylation.
Loss of the short arm of chromosome 1 and long arm of chromosome 19, referred to as 1p/19q codeletion, is caused by an unbalanced chromosomal translocation resulting in a loss of genetic material. 1p/19q Codeletion is commonly found in anaplastic oligodendrogliomas and mixed gliomas and is associated with increased chemosensitivity and radiosensitivity of the tumor. The presence of 1p/19q codeletion has been found to be the most important prognostic factor associated with improved survival in patients with anaplastic oligodendrogliomas.
Mutation in the IDH1 and IDH2 genes currently has an unknown mechanism affecting tumor biology, and the presence of mutation is associated with a better prognosis. MGMT promoter methylation results in MGMT gene silencing and is commonly found in anaplastic gliomas. It is presumed to increase tumor susceptibility to alkylating chemotherapy agents, and is associated with a better prognosis.
Surgery
The diagnosis of an anaplastic glioma is made histologically. Although biopsy may suffice for diagnosis, maximal safe resection significantly improves both progression-free survival and overall survival. Quality of life is also improved in patients treated with maximal surgical resection. The use of agents to improve visualization of tumor, such as 5-aminolevulinic acid (which causes tumor fluorescence), can lead to an improvement in achieving gross total resection and improves progression-free survival. However, because of the infiltrative nature of anaplastic gliomas, surgical resection is not curative, and treatment with radiotherapy, chemotherapy, or both modalities is required for further treatment of the tumor.
Evolution of treatment strategies for anaplastic gliomas
Radiation
Radiotherapy volume (whole brain radiotherapy vs external beam radiotherapy)
Whole brain radiotherapy (WBRT) following surgery for anaplastic gliomas was developed in the early 1970s and used through the early 1980s. Studies evaluating WBRT for malignant gliomas consistently showed a survival benefit, albeit modest. However, radiotherapy can have serious long-term neurotoxic effects, particularly in large treatment fields such as WBRT. These effects can include a progressive neurodegenerative process characterized by neuronal loss and demyelination, as well as both small and large vessel disease. In patients with expected long-term survival, such as those with anaplastic gliomas, and particularly those with anaplastic oligodendrogliomas, radiotherapy-induced neurotoxicity must be considered when making treatment decisions.
In patients treated with WBRT, tumor recurrence was recognized to commonly develop within 2 cm of the original tumor site. Because of this observation, as well as the significant risk of neurotoxicity with WBRT, external beam radiotherapy (EBRT) was developed to maximize treatment to the tumor and minimize radiation to surrounding brain tissue. A study of 50 patients with malignant glioma randomized to receive either EBRT 50 Gy followed by a boost of 10 Gy, or WBRT 40 Gy followed by a boost of 20 Gy, found no 6-month overall survival benefit in the EBRT group (66.7% vs 50.7%, P >.1), but there was a significant improvement in the KPS of patients treated with EBRT (80% vs 56% improved, P <.01).
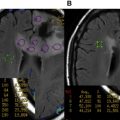
The development of neuroimaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI) has led to further refinement in the accuracy of EBRT. Using CT planning, three-dimensional (3D) conformal radiotherapy is now used to maximize radiotherapy to the tumor. Intensity-modulated radiotherapy (IMRT), in which radiation intensity is varied across the treatment field to further reduce the risk of radiation injury to critical adjacent brain structures, is also commonly used in many centers.
Radiotherapy dosing
The initial radiotherapy studies using WBRT typically used a treatment dosing of 50 to 60 Gy. Larger doses of radiotherapy were found to have higher toxicity rates with no improvement in survival. After EBRT became the accepted standard of care, a large trial of patients with malignant gliomas was conducted to establish the optimal radiotherapy dosing. In this study, 474 patients were randomized to receive either a low dose of 45 Gy in 20 fractions over 4 weeks or a high dose of 60 Gy in 30 fractions over 6 weeks. There was a significant increase in median survival in the high-dose group (12 vs 9 months, P = .007), establishing 60 Gy as the optimal target dose. The increase in survival was still evident in a subgroup analysis of patients with poor prognosis. More recent studies have confirmed that radiotherapy doses of more than 60 Gy do not confer a significant survival benefit for patients with anaplastic gliomas. A trial using a 3D conformal IMRT technique found no survival benefit in patients with malignant gliomas treated with 70, 80, or 90 Gy.
Fractionation schemes
Conventional fractionation refers to the once daily delivery of radiotherapy, typically with a dose of 1.8 to 2.0 Gy per day, for a total up to 60 Gy. Hyperfractionation refers to the delivery of 2 smaller doses of radiation per day, which can allow for an increase in the maximal dose of radiation that can be safely delivered. In a study of several hyperfractionation schemes with adjuvant carmustine, there was no survival benefit to patients with malignant gliomas treated to 72 Gy (with hyperfractionation of 1.2 Gy twice-daily dosing) compared with conventional radiotherapy at 60 Gy.
Additional smaller studies have also found no clear benefit to hyperfractionation versus conventional fractionation schemes. A review of fractionation schemes found that, although hyperfractionation can shorten the treatment time of radiotherapy for patients with malignant gliomas, it does not result in an improvement in overall survival.
Radiosensitizers
Radiosensitizers are compounds given concurrently with radiotherapy to increase the therapeutic effect of radiation. In the past 2 decades, several compounds have been investigated. However, none showed a clear benefit in survival.
In a small study of patients with recurrent malignant gliomas, α-difluoromethylornithine (DFMO), in combination with carmustine, was associated with a survival benefit. However, myelosuppression and hearing loss were dose-limiting toxicities. A larger study of 249 patients with anaplastic glioma randomized to receive either PCV (procarbazine, lomustine (1-(2-chloro-ethyl)-3-cyclohexyl-1-nitrosourea [CCNU]), and vincristine) chemotherapy or DFMO-PCV after surgery and radiotherapy found no difference in overall survival between the 2 groups, and a significant increase in gastrointestinal and hematologic toxicities in the DFMO-PCV group.
Other radiosensitizers include 5-bromo-2′-deoxyuridine (BrdU, bromodeoxyuridine) and misonidazole. BrdU was found to have no survival benefit, and likely worsened toxicity of radiation. Misonidazole was also found to trend toward worsened survival. At this time, radiosensitizers are not used in conventional therapy.
Current standard of care for radiation
Despite many years of research related to radiotherapy dosing and fractionation, there does not seem to be a significant benefit to any scheme other than EBRT given in conventional fractionation to a maximum dose of 60 Gy to a focal radiation field using 3D conformal planning techniques. Radiotherapy remains a frequent choice of the initial therapy for anaplastic gliomas, and this is discussed further later.
For slow-growing tumors such as anaplastic oligodendrogliomas, reirradiation may be considered for patients with an interval of at least several years since the prior radiotherapy. In a study of patients with recurrent glioma after cranial radiation treated with repeat radiotherapy at a median of 9 years, there was modestly improved overall survival, although most patients died of tumor progression before the onset of late effects from the reirradiation.
Chemotherapy
Carmustine
The earliest chemotherapy to show a survival benefit in anaplastic gliomas (included in trials of malignant gliomas) was carmustine ( N , N ′-bis(2-chloroethyl)- N -nitrosourea [BCNU]). From 1970 to 1990, no single chemotherapy agent or combination was found to confer a survival benefit that was superior to BCNU alone. However, BCNU has only a modest survival benefit, and a substantial risk of toxicity. In the German-Austrian Glioma (GAG) trial, patients with malignant glioma treated with surgery and WBRT were randomized to combination chemotherapy with BCNU plus teniposide or BCNU alone. There was no difference in overall survival and 36% of patients treated with BCNU experienced symptoms of pulmonary fibrosis within 12 months, in some cases after a single dose. The trial results are available, but are not published in peer-reviewed literature.
The high rate of pulmonary toxicity of BCNU in the GAG trial, as well as its modest efficacy, led to the study of alternative nitrosoureas. In the NOA-01 trial, patients with malignant glioma treated with surgery and EBRT were randomized to receive nimustine ((1-4-amino-2-methyl-5-pyrimidinyl)-methyl-3-(2-chloroethyl)-3-nitrosourea [ACNU]) plus teniposide or ACNU plus cytarabine. There was a modest overall survival advantage in both groups compared with historical controls in this trial, but, as with BCNU, ACNU has substantial toxicity and is not currently in clinical use in the United States. Lomustine (CCNU) also had modest efficacy and is currently the most commonly used nitrosourea, as a component of the PCV chemotherapy regimen.
PCV regimen
The PCV regimen consists of procarbazine, CCNU, and vincristine. In 1990, a trial of PCV versus single-agent BCNU in patients with malignant gliomas found a significantly improved overall survival in patients with anaplastic gliomas treated with PCV compared with BCNU (157 vs 82 weeks, P = .021). The study was small (only 36 and 37 patients in the PCV and BCNU arms, respectively) and it was not performed as an intention-to-treat analysis. Despite these limitations, this trial led to PCV replacing BCNU as the standard of care for chemotherapy, before the development of temozolomide.
As with radiotherapy, anaplastic oligodendrogliomas and mixed gliomas have a more favorable response to PCV compared with anaplastic astrocytomas in both progression-free and overall survival. However, PCV also has a substantial risk of toxicity. In a regimen using a dose-intense scheme of PCV, central neurotoxic side effects in combination with severe hematologic and hepatic toxicity were frequently observed. Many patients are thus unable to complete a full course of therapy.
Temozolomide
Temozolomide is an alkylating chemotherapy agent that has more recently been found to be effective in patients with anaplastic gliomas. In a retrospective analysis of 109 patients with anaplastic astrocytomas derived from 2 trials, adjuvant temozolomide was as effective as, and less toxic than, PCV. There was no significant difference in 2-year progression-free survival or median progression-free survival. However, temozolomide was discontinued less often than PCV because of toxicity (0% vs 37%).
Varying dose schedules of temozolomide have been evaluated in malignant gliomas. In one study, temozolomide was given daily for either 5 days (200 mg/m 2 /d) or 21 days (100 mg/m 2 /d), in 28-day cycles, up to 9 months. The 5-day-per-cycle dosing schedule had improved progression-free survival compared with the 21-day-per-cycle dosing (5.0 vs 4.2 months, P = .023), improved global quality of life (49% vs 19% improved, P = .005), and a trend toward improved overall survival (8.5 vs 6.6 months, P = .056). Temozolomide 5-day-per-cycle dosing also had improved progression-free survival compared with a standard PCV dosing regimen (5.0 vs 3.6 months, P = .038).
High-dose temozolomide (550 mg/m 2 ) in combination with BCNU (150 mg/m 2 ) given once in 42-day cycles was evaluated in a small study of patients with anaplastic gliomas. Nearly half of patients experienced grade 3 or 4 (according to National Cancer Institute Common Toxicity Criteria) hematologic toxicities. The complete and partial response rates were 2% and 27% respectively, and an additional 54% of patients had stable disease. This regimen was thought to be excessively toxic, without a strong survival benefit. Thus, temozolomide 5-day-per-cycle dosing is currently the standard dosing schedule.
In addition to efficacy as an initial treatment, temozolomide has been shown to have efficacy after recurrence of tumor. In one study, 38 patients with anaplastic oligodendrogliomas or mixed gliomas who were chemotherapy naïve, previously treated with surgery and radiation, were treated with temozolomide after tumor recurrence. More than half of patients had a complete (26.3%) or partial response to temozolomide. In another study, 67 patients with anaplastic oligodendrogliomas or mixed gliomas were treated with temozolomide after tumor recurrence. The overall response rate was 46.3%, with a higher response rate seen in patients with anaplastic oligodendrogliomas and tumors with 1p/19q codeletion.
In certain patient populations, for example extensively infiltrative gliomas affecting the dominant or both hemispheres, radiotherapy can be associated with significant morbidity, and monotherapy with temozolomide may be considered. Patients with 1p/19q codeletion have a longer progression-free survival, making temozolomide monotherapy an attractive option to avoid radiation-induced neurotoxicity. Temozolomide monotherapy may also be considered for elderly patients, because a significant number of patients can achieve a prolonged survival.
Salvage agents
Studies of patients with anaplastic oligodendroglioma have evaluated salvage chemotherapy with temozolomide and PCV. In one study, 48 patients with anaplastic oligodendrogliomas or mixed gliomas who had received previous radiation and PCV chemotherapy were treated with temozolomide, with an objective response rate of 43.8%, a median progression-free survival of 6.7 months, and a median overall survival of 10 months. PCV may also be used in recurrent anaplastic oligodendroglioma after radiation and temozolomide treatment.
Patients who have progressed on both PCV and temozolomide should be considered for a clinical trial. Newer agents, such as bevacizumab (a monoclonal antibody against vascular endothelial growth factor [VEGF]) are being evaluated for efficacy in anaplastic gliomas. A recent retrospective evaluation of single-agent bevacizumab was performed in 22 adults with recurrent 1p/19q codeleted anaplastic oligodendroglioma. Fifteen patients (68%) showed a partial radiographic response, with median time to progression of 6.75 months and median survival of 8.5 months. Other standard chemotherapy agents including irinotecan, carboplatin, paclitaxel, and etoposide plus cisplatin have failed to show survival benefit in patients with relapsed anaplastic gliomas.
Current standard of care for chemotherapy
For patients with anaplastic gliomas, temozolomide has been found to be at least as effective as the PCV regimen, with significantly less toxicity, improved ease of administration, and better tolerability. Because of this, temozolomide is now considered to be the first-line chemotherapy agent for anaplastic gliomas. The conventional dosing for temozolomide is 200 mg/m 2 /d once daily for 5 days in 28-day cycles, up to 9 months. If a patient has treatment failure with temozolomide, PCV or bevacizumab can be considered as salvage agents.
Evolution of treatment strategies for anaplastic gliomas
Radiation
Radiotherapy volume (whole brain radiotherapy vs external beam radiotherapy)
Whole brain radiotherapy (WBRT) following surgery for anaplastic gliomas was developed in the early 1970s and used through the early 1980s. Studies evaluating WBRT for malignant gliomas consistently showed a survival benefit, albeit modest. However, radiotherapy can have serious long-term neurotoxic effects, particularly in large treatment fields such as WBRT. These effects can include a progressive neurodegenerative process characterized by neuronal loss and demyelination, as well as both small and large vessel disease. In patients with expected long-term survival, such as those with anaplastic gliomas, and particularly those with anaplastic oligodendrogliomas, radiotherapy-induced neurotoxicity must be considered when making treatment decisions.
In patients treated with WBRT, tumor recurrence was recognized to commonly develop within 2 cm of the original tumor site. Because of this observation, as well as the significant risk of neurotoxicity with WBRT, external beam radiotherapy (EBRT) was developed to maximize treatment to the tumor and minimize radiation to surrounding brain tissue. A study of 50 patients with malignant glioma randomized to receive either EBRT 50 Gy followed by a boost of 10 Gy, or WBRT 40 Gy followed by a boost of 20 Gy, found no 6-month overall survival benefit in the EBRT group (66.7% vs 50.7%, P >.1), but there was a significant improvement in the KPS of patients treated with EBRT (80% vs 56% improved, P <.01).
The development of neuroimaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI) has led to further refinement in the accuracy of EBRT. Using CT planning, three-dimensional (3D) conformal radiotherapy is now used to maximize radiotherapy to the tumor. Intensity-modulated radiotherapy (IMRT), in which radiation intensity is varied across the treatment field to further reduce the risk of radiation injury to critical adjacent brain structures, is also commonly used in many centers.
Radiotherapy dosing
The initial radiotherapy studies using WBRT typically used a treatment dosing of 50 to 60 Gy. Larger doses of radiotherapy were found to have higher toxicity rates with no improvement in survival. After EBRT became the accepted standard of care, a large trial of patients with malignant gliomas was conducted to establish the optimal radiotherapy dosing. In this study, 474 patients were randomized to receive either a low dose of 45 Gy in 20 fractions over 4 weeks or a high dose of 60 Gy in 30 fractions over 6 weeks. There was a significant increase in median survival in the high-dose group (12 vs 9 months, P = .007), establishing 60 Gy as the optimal target dose. The increase in survival was still evident in a subgroup analysis of patients with poor prognosis. More recent studies have confirmed that radiotherapy doses of more than 60 Gy do not confer a significant survival benefit for patients with anaplastic gliomas. A trial using a 3D conformal IMRT technique found no survival benefit in patients with malignant gliomas treated with 70, 80, or 90 Gy.
Fractionation schemes
Conventional fractionation refers to the once daily delivery of radiotherapy, typically with a dose of 1.8 to 2.0 Gy per day, for a total up to 60 Gy. Hyperfractionation refers to the delivery of 2 smaller doses of radiation per day, which can allow for an increase in the maximal dose of radiation that can be safely delivered. In a study of several hyperfractionation schemes with adjuvant carmustine, there was no survival benefit to patients with malignant gliomas treated to 72 Gy (with hyperfractionation of 1.2 Gy twice-daily dosing) compared with conventional radiotherapy at 60 Gy.
Additional smaller studies have also found no clear benefit to hyperfractionation versus conventional fractionation schemes. A review of fractionation schemes found that, although hyperfractionation can shorten the treatment time of radiotherapy for patients with malignant gliomas, it does not result in an improvement in overall survival.
Radiosensitizers
Radiosensitizers are compounds given concurrently with radiotherapy to increase the therapeutic effect of radiation. In the past 2 decades, several compounds have been investigated. However, none showed a clear benefit in survival.
In a small study of patients with recurrent malignant gliomas, α-difluoromethylornithine (DFMO), in combination with carmustine, was associated with a survival benefit. However, myelosuppression and hearing loss were dose-limiting toxicities. A larger study of 249 patients with anaplastic glioma randomized to receive either PCV (procarbazine, lomustine (1-(2-chloro-ethyl)-3-cyclohexyl-1-nitrosourea [CCNU]), and vincristine) chemotherapy or DFMO-PCV after surgery and radiotherapy found no difference in overall survival between the 2 groups, and a significant increase in gastrointestinal and hematologic toxicities in the DFMO-PCV group.
Other radiosensitizers include 5-bromo-2′-deoxyuridine (BrdU, bromodeoxyuridine) and misonidazole. BrdU was found to have no survival benefit, and likely worsened toxicity of radiation. Misonidazole was also found to trend toward worsened survival. At this time, radiosensitizers are not used in conventional therapy.
Current standard of care for radiation
Despite many years of research related to radiotherapy dosing and fractionation, there does not seem to be a significant benefit to any scheme other than EBRT given in conventional fractionation to a maximum dose of 60 Gy to a focal radiation field using 3D conformal planning techniques. Radiotherapy remains a frequent choice of the initial therapy for anaplastic gliomas, and this is discussed further later.
For slow-growing tumors such as anaplastic oligodendrogliomas, reirradiation may be considered for patients with an interval of at least several years since the prior radiotherapy. In a study of patients with recurrent glioma after cranial radiation treated with repeat radiotherapy at a median of 9 years, there was modestly improved overall survival, although most patients died of tumor progression before the onset of late effects from the reirradiation.
Chemotherapy
Carmustine
The earliest chemotherapy to show a survival benefit in anaplastic gliomas (included in trials of malignant gliomas) was carmustine ( N , N ′-bis(2-chloroethyl)- N -nitrosourea [BCNU]). From 1970 to 1990, no single chemotherapy agent or combination was found to confer a survival benefit that was superior to BCNU alone. However, BCNU has only a modest survival benefit, and a substantial risk of toxicity. In the German-Austrian Glioma (GAG) trial, patients with malignant glioma treated with surgery and WBRT were randomized to combination chemotherapy with BCNU plus teniposide or BCNU alone. There was no difference in overall survival and 36% of patients treated with BCNU experienced symptoms of pulmonary fibrosis within 12 months, in some cases after a single dose. The trial results are available, but are not published in peer-reviewed literature.
The high rate of pulmonary toxicity of BCNU in the GAG trial, as well as its modest efficacy, led to the study of alternative nitrosoureas. In the NOA-01 trial, patients with malignant glioma treated with surgery and EBRT were randomized to receive nimustine ((1-4-amino-2-methyl-5-pyrimidinyl)-methyl-3-(2-chloroethyl)-3-nitrosourea [ACNU]) plus teniposide or ACNU plus cytarabine. There was a modest overall survival advantage in both groups compared with historical controls in this trial, but, as with BCNU, ACNU has substantial toxicity and is not currently in clinical use in the United States. Lomustine (CCNU) also had modest efficacy and is currently the most commonly used nitrosourea, as a component of the PCV chemotherapy regimen.
PCV regimen
The PCV regimen consists of procarbazine, CCNU, and vincristine. In 1990, a trial of PCV versus single-agent BCNU in patients with malignant gliomas found a significantly improved overall survival in patients with anaplastic gliomas treated with PCV compared with BCNU (157 vs 82 weeks, P = .021). The study was small (only 36 and 37 patients in the PCV and BCNU arms, respectively) and it was not performed as an intention-to-treat analysis. Despite these limitations, this trial led to PCV replacing BCNU as the standard of care for chemotherapy, before the development of temozolomide.
As with radiotherapy, anaplastic oligodendrogliomas and mixed gliomas have a more favorable response to PCV compared with anaplastic astrocytomas in both progression-free and overall survival. However, PCV also has a substantial risk of toxicity. In a regimen using a dose-intense scheme of PCV, central neurotoxic side effects in combination with severe hematologic and hepatic toxicity were frequently observed. Many patients are thus unable to complete a full course of therapy.
Temozolomide
Temozolomide is an alkylating chemotherapy agent that has more recently been found to be effective in patients with anaplastic gliomas. In a retrospective analysis of 109 patients with anaplastic astrocytomas derived from 2 trials, adjuvant temozolomide was as effective as, and less toxic than, PCV. There was no significant difference in 2-year progression-free survival or median progression-free survival. However, temozolomide was discontinued less often than PCV because of toxicity (0% vs 37%).
Varying dose schedules of temozolomide have been evaluated in malignant gliomas. In one study, temozolomide was given daily for either 5 days (200 mg/m 2 /d) or 21 days (100 mg/m 2 /d), in 28-day cycles, up to 9 months. The 5-day-per-cycle dosing schedule had improved progression-free survival compared with the 21-day-per-cycle dosing (5.0 vs 4.2 months, P = .023), improved global quality of life (49% vs 19% improved, P = .005), and a trend toward improved overall survival (8.5 vs 6.6 months, P = .056). Temozolomide 5-day-per-cycle dosing also had improved progression-free survival compared with a standard PCV dosing regimen (5.0 vs 3.6 months, P = .038).
High-dose temozolomide (550 mg/m 2 ) in combination with BCNU (150 mg/m 2 ) given once in 42-day cycles was evaluated in a small study of patients with anaplastic gliomas. Nearly half of patients experienced grade 3 or 4 (according to National Cancer Institute Common Toxicity Criteria) hematologic toxicities. The complete and partial response rates were 2% and 27% respectively, and an additional 54% of patients had stable disease. This regimen was thought to be excessively toxic, without a strong survival benefit. Thus, temozolomide 5-day-per-cycle dosing is currently the standard dosing schedule.
In addition to efficacy as an initial treatment, temozolomide has been shown to have efficacy after recurrence of tumor. In one study, 38 patients with anaplastic oligodendrogliomas or mixed gliomas who were chemotherapy naïve, previously treated with surgery and radiation, were treated with temozolomide after tumor recurrence. More than half of patients had a complete (26.3%) or partial response to temozolomide. In another study, 67 patients with anaplastic oligodendrogliomas or mixed gliomas were treated with temozolomide after tumor recurrence. The overall response rate was 46.3%, with a higher response rate seen in patients with anaplastic oligodendrogliomas and tumors with 1p/19q codeletion.
In certain patient populations, for example extensively infiltrative gliomas affecting the dominant or both hemispheres, radiotherapy can be associated with significant morbidity, and monotherapy with temozolomide may be considered. Patients with 1p/19q codeletion have a longer progression-free survival, making temozolomide monotherapy an attractive option to avoid radiation-induced neurotoxicity. Temozolomide monotherapy may also be considered for elderly patients, because a significant number of patients can achieve a prolonged survival.
Salvage agents
Studies of patients with anaplastic oligodendroglioma have evaluated salvage chemotherapy with temozolomide and PCV. In one study, 48 patients with anaplastic oligodendrogliomas or mixed gliomas who had received previous radiation and PCV chemotherapy were treated with temozolomide, with an objective response rate of 43.8%, a median progression-free survival of 6.7 months, and a median overall survival of 10 months. PCV may also be used in recurrent anaplastic oligodendroglioma after radiation and temozolomide treatment.
Patients who have progressed on both PCV and temozolomide should be considered for a clinical trial. Newer agents, such as bevacizumab (a monoclonal antibody against vascular endothelial growth factor [VEGF]) are being evaluated for efficacy in anaplastic gliomas. A recent retrospective evaluation of single-agent bevacizumab was performed in 22 adults with recurrent 1p/19q codeleted anaplastic oligodendroglioma. Fifteen patients (68%) showed a partial radiographic response, with median time to progression of 6.75 months and median survival of 8.5 months. Other standard chemotherapy agents including irinotecan, carboplatin, paclitaxel, and etoposide plus cisplatin have failed to show survival benefit in patients with relapsed anaplastic gliomas.
Current standard of care for chemotherapy
For patients with anaplastic gliomas, temozolomide has been found to be at least as effective as the PCV regimen, with significantly less toxicity, improved ease of administration, and better tolerability. Because of this, temozolomide is now considered to be the first-line chemotherapy agent for anaplastic gliomas. The conventional dosing for temozolomide is 200 mg/m 2 /d once daily for 5 days in 28-day cycles, up to 9 months. If a patient has treatment failure with temozolomide, PCV or bevacizumab can be considered as salvage agents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree