Adaptive Immunity
Under circumstances in which infectious organisms are not eliminated by innate immune mechanisms, adaptive immune responses ensue, with the generation of antigen-specific lymphocytes (effector cells) and memory cells that can prevent reinfection with the same organism. These responses (sometimes called adaptive immunity) are attributes of virtually every living organism in one form or another; adaptive immunity is a more specialized form of immunity. It developed late in evolution and is found only in vertebrates. As discussed in Chapter 2, the various elements that participate in innate immunity exhibit broad specificity against the foreign agents they encounter through their recognition of antigens that display molecules not found in the host (e.g., N-formylated peptides). By contrast, adaptive immunity always exhibits antigenic specificity. As its name implies, adaptive immunity is a consequence of an encounter with a foreign substance. The first encounter with a particular foreign substance that has penetrated the body triggers a chain of events that induces an immune response with specificity against that foreign substance. Details of how this happens within the B- and T-cell lineages will be presented in the chapters that follow.
Cells and Organs Involved in Adaptive Immunity
In contrast with innate immunity, adaptive immune responses develop only after exposure to or immunization with a given substance or antigen. As we have already discussed, the effector cells responsible for adaptive immune responses are the B and T cells. Unlike innate immune cells that use germline-encoded receptors to detect and respond to microbes and other foreign antigens, B and T cells express somatically generated antigen-specific receptors that are not germline encoded but rather are the translational products of multiple genes that are pieced together by gene rearrangements that occur during their development. B cells expressing antigen-specific B-cell receptors (BCRs) synthesize and secrete antibody into the bloodstream. This is often termed humoral immunity. T cells also exhibit antigen specificity by virtue of their expression of antigen-specific T-cell receptors (TCRs). In the case of T cells, their participation in adaptive immune responses is as varied as the T-cell subsets and cytokines they produce. Historically, T-cell mediated responses have been referred to as cell-mediated responses or cellular immunity.
Unlike B cells expressing BCRs that bind directly to antigens for which they are specific, T cells are incapable of binding to antigens directly. Instead, they recognize and bind to antigenic peptides when they come in contact with antigen-presenting cells (APCs) such as macrophages and dendritic cells that display processed, major histocompatibility complex (MHC)-bound peptides derived from the antigen (see Chapter 9). However, even this APC-dependent recognition of peptides is insufficient to activate the responding T cell. Indeed, two signals are required to activate T cells: (1) T-cell expression of peptide (epitope)-specific TCRs and, (2) ligation of T-cell expressed co-stimulatory molecules with complimentary membrane molecules expressed by APCs. The co-stimulatory signaling step initiates a cascade of intracellular and nuclear events that measurably change the behavior of responding T cells. Thus, T cells begin to express and release new gene products (e.g., cytokines), they undergo clonal expansion to increase the number of TCR-expressing cells within the T-cell repertoire, and they differentiate to create a pool of memory cells. These events occur in the secondary lymphoid organs (lymph nodes and spleen) as we will discuss in the next section of this chapter.
T-cell activation greatly facilitates the activation and differentiation of B cells responding to antigen. This is principally achieved by the action of T-cell–derived cytokines that bind to specific cytokine receptors expressed by B cells. Functional consequences of this T-cell help include B-cell proliferation, generation of memory B cells, and diversification of the kinds of immunoglobulins produced (immunoglobulin class switching). The recurring theme of cytokine involvement in normal immune responses is underscored by the fact that B cells are dependent on T cells for optimal antibody responses to most antigens. The term T-cell–dependent antigens is often used to characterize these antigens.
The Lymphatic Organs
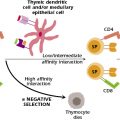
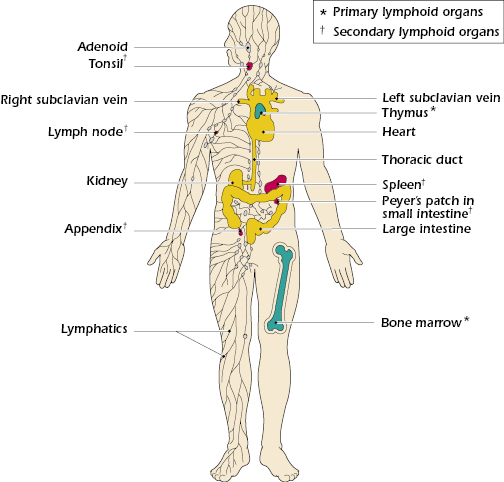
The lymphatic system includes organs in which lymphocyte maturation, differentiation, and proliferation take place. They are generally divided into two categories: (1) primary and (2) secondary organs. The primary or central lymphoid organs are those in which the maturation of B and T lymphocytes into antigen-recognizing lymphocytes occurs. In other words, these are the organs where gene rearrangements occur to generate functional antigen-specific BCR and TCR expressed by B and T cells, respectively. Mature B cells differentiate to fully mature cells within the bone marrow. Historically, the term “B cell” is derived from developmental studies in birds that demonstrated that antibody-forming lymphocytes differentiate within an organ unique to birds called the bursa of Fabricius (hence, “B” for bursa). In contrast, T cells differentiate only partially within the bone marrow. Precursor cells destined to become mature T cells undergo final maturation within the thymus gland (hence, “T” for thymus). Histological characteristics of the thymus are discussed in the next section.
Mature B and T cells migrate through the bloodstream and lymphatic system to the peripheral lymphoid tissues, including the lymph nodes and spleen. Collectively, these are referred to as the secondary lymphoid organs and this is where antigen-driven activation (proliferation and differentiation) of B and T cells takes place (Figure 3.1). Histological properties of the secondary lymphoid organs are also presented below.
Thymus Gland.
The thymus gland is a bilobed structure, derived from the endoderm of the third and fourth pharyngeal pouches. During fetal development, the size of the thymus increases. The growth continues until puberty. Thereafter, the thymus undergoes atrophy with aging.
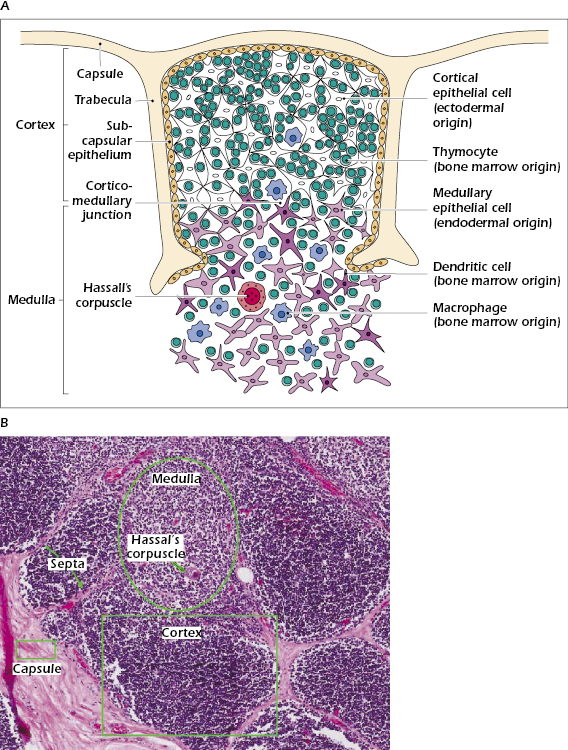
The thymus is a lymphoepithelial organ and consists of epithelial cells organized into cortical (outer) and medullary (central) areas that are infiltrated with lymphoid cells (thymocytes) (Figure 3.2A). The cortex is densely populated with lymphocytes of various sizes, most of which are immature, and scattered macrophages involved in clearing apoptotic thymocytes. Figure 3.2B shows a section through normal human thymus tissue.
Secondary Lymphoid Organs.
The secondary lymphoid organs have two major functions: (1) They are highly efficient in trapping and concentrating foreign substances, and (2) they are the main sites of production of antibodies and the induction of antigen-specific T lymphocytes. The major secondary lymphoid organs are the spleen and the lymph nodes. In addition, tonsils, appendix, clusters of lymphocytes distributed in the lining of the small intestine (Peyer’s patches), and lymphoid aggregates spread throughout mucosal tissue are considered secondary lymphoid organs. These secondary lymphoid organs are found in various areas of the body, such as the linings of the digestive tract, in the respiratory and genitourinary tracts, in the conjunctiva, and in the salivary glands, where mature lymphocytes interact with antigen and undergo activation. These mucosal secondary lymphoid organs have been given the name mucosa-associated lymphoid tissue (MALT). Those lymphoid tissues associated with the gut are gut-associated lymphoid tissue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree