(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
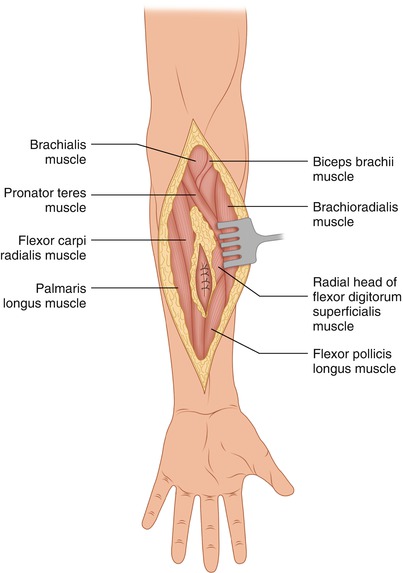
The illustrations in this chapter depict the dissection of a soft tissue sarcoma in the ventral aspect of the forearm (Fig. 5.1). The previously used biopsy incision is included within a long elliptical incision. Obviously, if an open biopsy is performed, the biopsy site should be over the middle of the underlying tumor, reached through a longitudinal incision. The elliptical incision is carried out around the previous biopsy site and made sufficiently long to allow proximal and distal identification and dissection of the various anatomical structures (Fig. 5.2). In surgery for an extremity sarcoma, development of very wide flaps on the basis of external palpatory findings alone should be avoided, as they may be unnecessarily wide. Instead, the surgeon should begin with modest dissection of the flaps, to be further extended following entry into the tissues and planes proximal and distal to the tumor mass, which should further guide the precise extent of the necessary development of either or both of the two flaps.
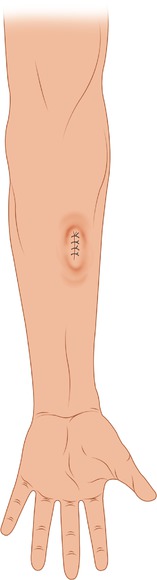
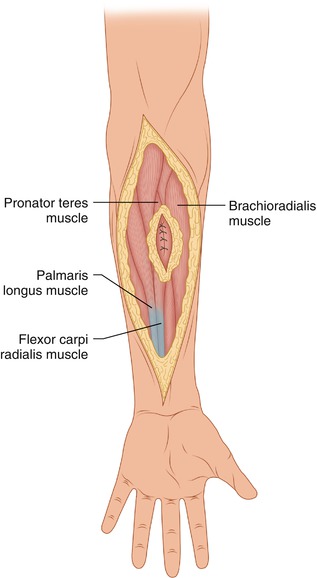
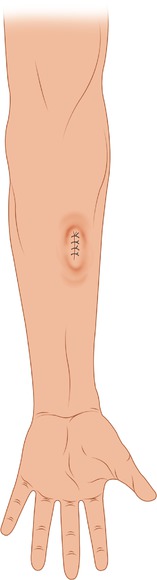
Fig. 5.1
A longitudinal biopsy incision has been made over the middle of the tumor protuberance
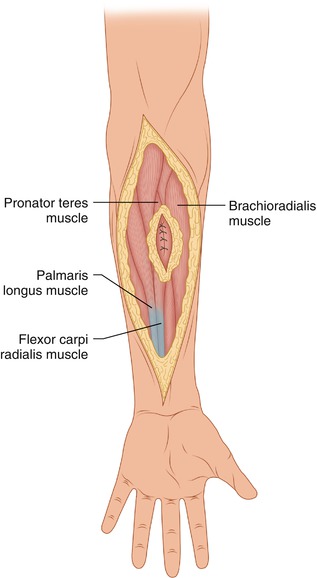
Fig. 5.2
Flaps have been developed and the deep fascia has been incised, exposing the underlying muscles
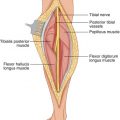
The brachioradialis muscle and extensor carpi radialis longus and brevis are exposed at their origin from the lateral supracondylar ridge and lateral epicondyle of the humerus. Although these muscles are visible and often are dissected with tumors of the ventral aspect of the forearm, anatomically they belong to the posterior antebrachial muscles in the extensor aspect of the forearm. If necessary, a portion of the brachioradialis or the entire muscle, as well as the extensors of the wrist, can be removed without significant functional deficit. By incising the fascia at the level of the antecubital fossa, the brachial artery and (medial to that) the median nerve are exposed. The brachial artery at this point bifurcates into the radial branch, which courses in front of the pronator teres in a lateral direction, and the ulnar artery. The radial branch assumes a position under the brachioradialis muscle, lying successively on the surface of the pronator teres, the radial head of the flexor digitorum superficialis, and the flexor pollicis longus. Lateral to the radial artery, the superficial branch of the radial nerve is visible. This branch, about 5 cm above the styloid process of the radius, passes under the brachioradialis and the radial extensor tendons of the wrist, descends toward the “anatomical snuff-box,” and divides into five dorsal digital nerves. Two of these supply the thumb and three run to the fingers, supplying the skin of the lateral two thirds of the back of the hand and the skin of the back of the thumb, forefinger, middle finger, and lateral half of the ring finger as far as the end of the proximal phalanx. More proximally in the antecubital fossa, as the radial nerve emerges between the brachioradialis and brachialis muscles, it bifurcates into the superficial branch of the radial nerve and the deep branch (posterior interosseous nerve). The posterior interosseous branch pierces the supinator muscle and enters the back of the forearm. The median nerve courses between the humeral and ulnar heads of the pronator teres and then beneath the flexor digitorum superficialis to run on its posterior surface. In the case presented, the tumor was laterally separated from the radial artery by ligating and dividing small branches supplying the radial side of the tumor, but if the artery is involved, it can be sacrificed by ligating it proximal and distal to its area of involvement. The ulnar artery, a branch of the brachial artery, proceeds under the pronator teres and flexor digitorum superficialis to descend on the surface of the deep muscles of the forearm. It is joined on the medial side by the ulnar nerve, which courses behind the medial epicondyle of the humerus between the two heads of the flexor carpi ulnaris, enters the same space, and assumes a position medial to the ulnar artery. Lateral to the tumor mass, the muscle fibers of the radial head of the flexor digitorum superficialis were exposed and divided close to their origin (Fig. 5.3). As the muscle fibers of the flexor digitorum superficialis are divided, care is exercised to avoid injury to the median nerve, which lies directly underneath (Fig. 5.4). Removal of the tumor mass in the case presented involved resecting also the radial head and a portion of the humeroulnar head of the flexor digitorum superficialis (Fig. 5.5). Incising the radial head of the flexor digitorum superficialis provides a good approach when necessary to expose the median nerve and the deep muscles (i.e., the flexor pollicis longus, flexor digitorum profundus, and pronator quadratus).