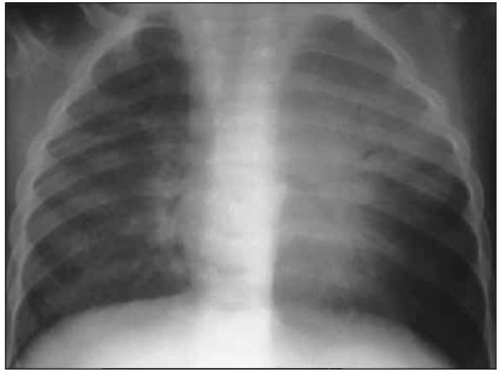
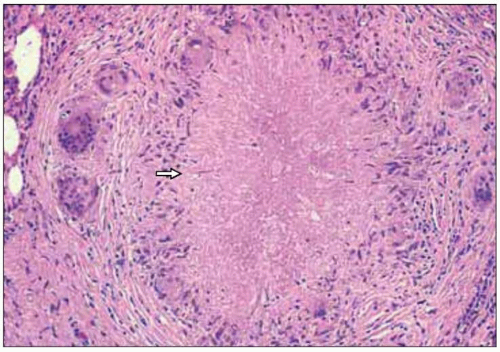
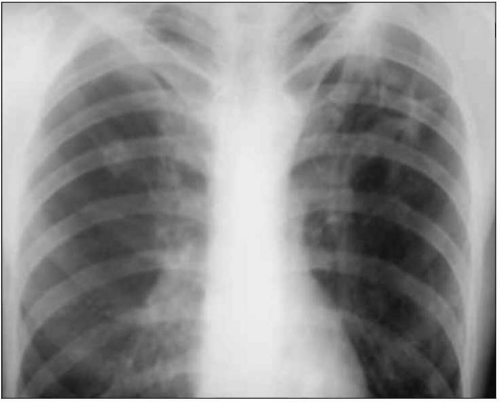
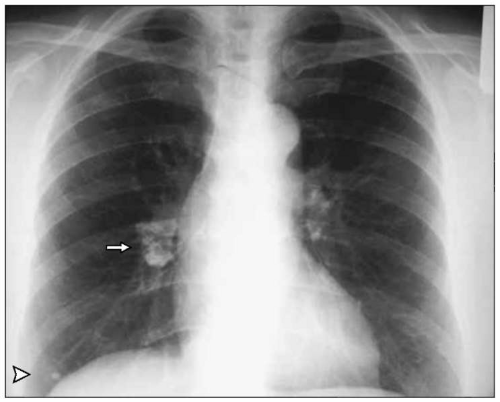
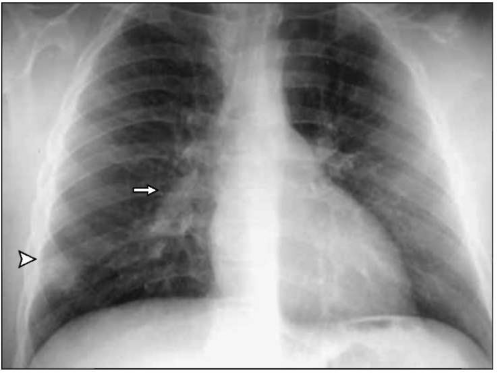
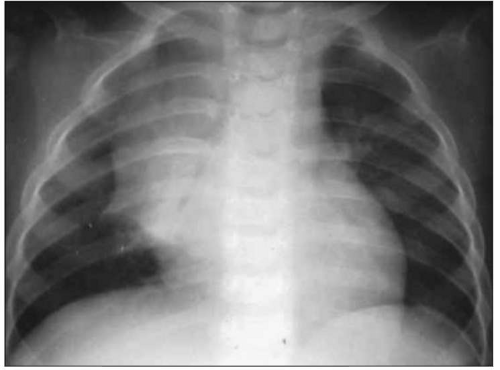
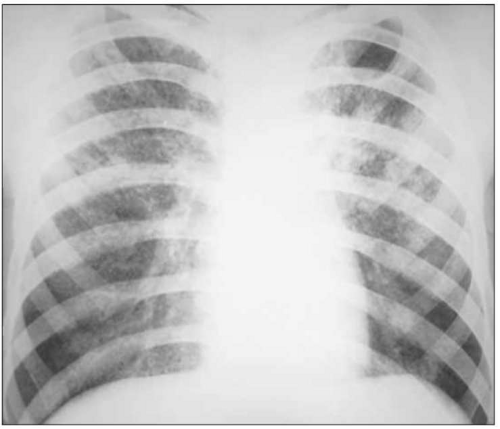
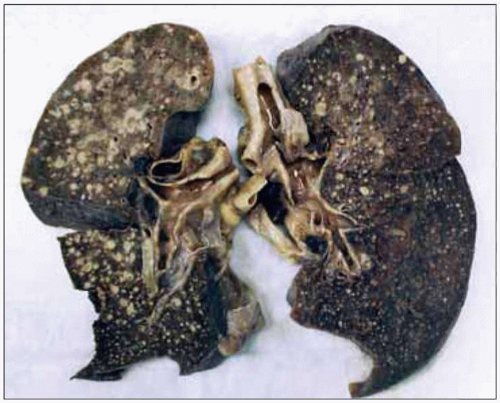
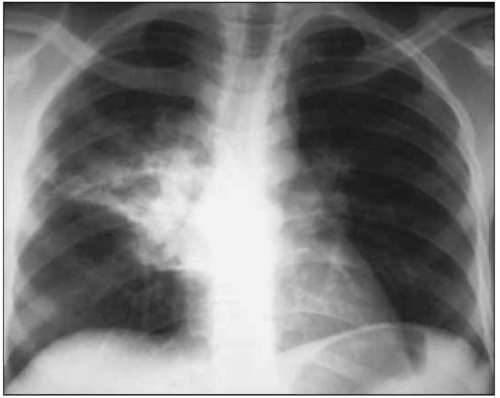
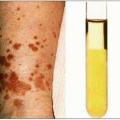
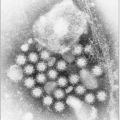
Patients starting on antituberculous chemotherapy may develop acute worsening of their symptoms or existing tuberculous lesions or new lesions; these are termed paradoxical or immune reconstitution inflammatory syndrome (
IRIS) reactions.
IRIS reactions occur more frequently in HIV-infected patients with
TB (7-36% of patients) and are more common when highly active antiretroviral therapy (
HAART) and anti-TB treatment are started at the same time. The cause of
IRIS reactions is unclear, but they may be due to reconstitution of the host immune response and an increased inflammatory response to mycobacterial antigens after beginning
HIV and anti-TB therapy. Most occur within 4-12 weeks after starting
HAART.
IRIS reactions are more common in patients with extrapulmonary
TB or low CD4+ lymphocyte counts. New or worsening adenopathy, fever, and new pulmonary infiltrates or pleural effusion are the most common presentations. After excluding other opportunistic infections, non-adherence with
TB treatment, and drug resistant
TB, management is by treatment of symptoms. Adjunctive corticosteroids may be helpful in severe cases.
HAART therapy can usually be continued. Illustrative cases are shown in
Figs. 4.19, 4.20 and 4.21.