TREATMENT OF ADULT MALE HYPOGONADISM
TESTOSTERONE FORMULATIONS
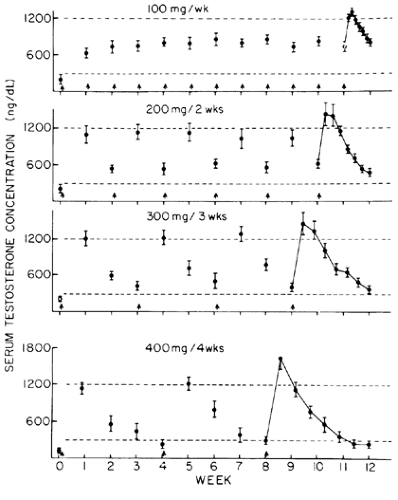
The long-acting 17β-hydroxyl esters of testosterone, testosterone enanthate and testosterone cypionate, are the most practical, effective, and safe, and least expensive preparations available for androgen replacement therapy for hypogonadal men. The intramuscular administration of 200 mg of testosterone enanthate induces peak serum testosterone levels at or just above the upper limits of the normal adult male range within 1 to 2 days of administration (Fig. 119-1).35 Testosterone levels usually remain within the normal range for 2 weeks. By increasing the dose of testosterone enanthate to 300 mg, eugonadal levels of testosterone in blood are maintained for 3 weeks (see Fig. 119-1). However, the administration of 400 mg of testosterone enanthate does not maintain normal serum testosterone levels for >3 weeks (see Fig. 119-1). No formal evaluations of the optimal dosage of testosterone cypionate have been reported. Because the kinetics of serum testosterone levels after a single intramuscular injection of testosterone cypionate are similar to those after a single injection of testosterone enanthate, however, the two preparations are thought to be therapeutically equivalent in terms of duration of action and potency.
In adults, androgen replacement therapy is usually instituted with testosterone enanthate or testosterone cypionate at a dosage of 200 mg, intramuscularly, every 2 weeks. Patients can usually be taught to self-administer intramuscular injections, or a family member or friend may be trained to give them. The assessment of therapeutic efficacy is accomplished by careful monitoring of the clinical response. Ideally, serum testosterone concentrations should be in the midnormal range 1 week after a testosterone ester injection and above the lower limit of the normal range immediately before the next injection. In some hypogonadal men, the large fluctuations in serum testosterone concentrations between intramuscular injections of testosterone enanthate or testosterone cypionate given every 2 to 3 weeks produce disturbing fluctuations in sexual function, energy, and mood.56 Patients may complain of reduced libido, erectile dysfunction, and diminished energy a few days before their next testosterone injection. The documentation of low serum testosterone levels at that time may be useful to justify an adjustment of the dosage interval (e.g., from every 2 weeks to every 10 days).
In elderly hypogonadal patients with symptoms of bladder outlet obstruction or enlarged prostate glands, the prudent approach is to begin testosterone therapy gradually and at a reduced dosage (e.g., testosterone enanthate or cypionate 50– 100 mg intramuscularly every 2–4 weeks). Alternatively, a short-acting testosterone ester may be used, such as testosterone propionate, 25 to 50 mg given intramuscularly three times weekly. The shorter duration of action permits rapid withdrawal if androgen-induced prostatic growth, urinary obstruction, or a prostatic nodule develops, but the need for frequent injections limit the practicality and acceptability of this approach.
Transdermal testosterone gel or patches (see earlier) provide alternatives to testosterone ester injections for androgen replacement in adult hypogonadal men who refuse or cannot tolerate intramuscular injections every 2 to 3 weeks; cannot administer injections to themselves or logistically arrange for injections to be given; have a bleeding diathesis; or have a personal preference.
A transdermal testosterone gel formulation (AndroGel) is a useful alternative to testosterone ester injections for androgen replacement therapy in hypogonadal men. Daily application of 50, 75, or 100 mg of testosterone in a 1% hydroalcoholic gel for 180 days in men with androgen deficiency produced relatively constant serum testosterone levels in the middle to upper physiologic range throughout the entire day (Fig. 119-2). By comparison, nightly application of a permeation-enhanced nonscrotal patch (Androderm) produced testosterone levels that exhibited a normal circadian variation in the lower normal range. AndroGel treatment increased energy and a sense of well being; improved libido and sexual function; increased lean body mass, muscle mass and strength, bone turnover markers, bone mineral density, and hematocrit; and decreased fat mass in a dose-dependent fashion, generally to a greater extent than did the testosterone patch. Compared to Androderm, AndroGel caused relatively little skin irritation and was associated with better compliance. However, AndroGel caused a disproportionate elevation in serum DHT levels, probably because of the large surface area of skin (containing 5 α-reductase) on which it is applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree