THYROID GLAND AND PREGNANCY
Numerous changes occur in the thyroid gland and in the levels of thyroid hormones during pregnancy.42 When iodine intake is marginal, increased renal clearance results in iodine deficiency, and minimal enlargement of the thyroid may ensue.43 The iodine in iodized salt and in prenatal vitamins usually prevents this deficiency and the resultant thyroid enlargement. These small amounts of iodine (6–40 mg daily) cause only a transient, mild fall in fetal free T4 levels, and the fetus soon escapes this inhibition, as does the mother.44 Excessive iodine ingestion should be avoided, however, because iodine crosses the placenta and may cause neonatal goiter (see later).
The belief is widespread that a goiter commonly develops during pregnancy. This belief is based on uncontrolled observations in the early literature made in iodine-deficient areas.45 In
iodine-replete regions, no increase is seen in the frequency of goiters during pregnancy.45,46 Of 309 pregnant adolescents in one study, 19 had goiters,46 2 had Graves disease and hyperthy-roidism, 3 had Hashimoto thyroiditis (1 with hyperthyroidism), 4 had subacute thyroiditis (1 with hyperthyroidism), and 9 had simple nontoxic goiters. Thus, the presence of a palpable goiter in iodine-replete areas indicates significant disease in ˜50% of patients and always requires evaluation.
iodine-replete regions, no increase is seen in the frequency of goiters during pregnancy.45,46 Of 309 pregnant adolescents in one study, 19 had goiters,46 2 had Graves disease and hyperthy-roidism, 3 had Hashimoto thyroiditis (1 with hyperthyroidism), 4 had subacute thyroiditis (1 with hyperthyroidism), and 9 had simple nontoxic goiters. Thus, the presence of a palpable goiter in iodine-replete areas indicates significant disease in ˜50% of patients and always requires evaluation.
The fetal thyroid and the fetal hypothalamic–pituitary–thyroid axis develop independently of the maternal thyroid status. The components of this axis are functioning after 10 weeks of gestation. By 11 to 12 weeks of gestation, the fetal thyroid begins to concentrate iodine, and T4 and TSH are present in the fetal circulation.47 The placenta is permeable to iodine and to medications used to treat hyperthyroidism, such as propylthiouracil (PTU), methimazole, and propranolol. Triiodothyronine (T3) and TSH cross the placenta only minimally.42,48 When fetal thyroid disease is suspected, the assessment for a goiter can be performed using ultrasonography48; percutaneous cord blood sampling can be carried out to evaluate fetal thyroid hormone status,47 and therapy can be initiated to forestall problems. T4 crosses the placenta in somewhat larger amounts than T3, and its administration to mothers late in gestation leads to amelioration of the effects of hypothyroidism in infants with congenital hypothyroidism resulting from enzyme defects or agenesis of the thyroid.49
Thyroid-stimulating activity as measured by serum bioassay is increased in the first trimester because of the intrinsic thyroid-stimulating activity of hCG.42,43,50 The hCG may cause increased T4 and T3 levels, as well as a transient hyperthyroidism associated with hyperemesis gravidarum (see later). Markedly elevated levels of hCG secreted by trophoblastic neoplasms also may cause hyperthyroidism.50 In addition, a human chorionic thyrotropin may be made by the placenta, but it has little thyroid-stimulating activity and probably plays no physiologic role.51
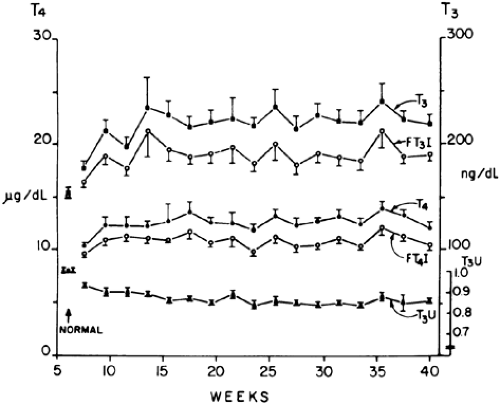
The increased estrogens produced by the fetal-placental unit raise thyroid hormone–binding globulin levels in the mother by stimulating its hepatic production, as well as by decreasing its degradation through altered glycosylation.42,51 The increased thyroid hormone–binding globulin levels result in higher levels of bound T4, beginning by 4 to 6 weeks of gestation51 (Fig. 110-2). Free T4 levels have been reported to be unchanged, increased, or decreased during pregnancy, although they remain within the normal range in most patients.42,43,51 These differences may relate to relative iodine deficiencies in the populations studied43 and to the stage of pregnancy being assessed. The slightly elevated free T4 levels seen in some persons may result from the stimulating activity of the high levels of hCG.43,50,51 T3 is bound to thyroid hormone–binding globulin with somewhat less affinity than T4, but increases in total T3 levels similar to those of T4 are observed during pregnancy.51 TSH levels are decreased minimally during pregnancy, possibly because of the increased free T4 levels.51
HYPERTHYROIDISM
Hyperthyroidism occurs in ˜2 of every 1000 pregnancies.42,52 Approximately 95% of these cases are caused by Graves disease (see Chap. 42). Preexisting Graves disease often ameliorates during pregnancy, as do other autoimmune disorders, perhaps due to the gestationally mediated alterations in immune mechanisms.42,52 Clinical improvement is most likely to occur in the second half of pregnancy, paralleling the fall in circulating levels of the stimulatory immunoglobulins.52 However, Graves disease also may present initially or may relapse during pregnancy.42,52 Hyperthyroidism may be exacerbated postpartum, possibly because the pregnancy had an ameliorating effect on the disease that was lost with delivery.
Untreated hyperthyroidism clearly has an adverse consequence on fetal outcome. Among 57 patients with uncontrolled hyperthyroidism, 25 had low-birth-weight infants (a nine-fold increase in relative risk), 19 had premature deliveries (a 16.5-fold increase in relative risk), and 8 developed preeclampsia (a 4.74-fold increase in relative risk); however, no perinatal deaths occurred.53 In patients who were hyperthyroid but whose condition was brought under control during the pregnancy, these numbers were considerably improved but still not normal. Patients whose hyperthyroidism was under control throughout the pregnancy had no increased risk of these complications.53
DIAGNOSIS OF HYPERTHYROIDISM DURING PREGNANCY
The hyperdynamic state of pregnancy may make the clinical diagnosis of hyperthyroidism more difficult; tachycardia, warm skin, systolic flow murmurs, and heat intolerance are common to both. Even the presence of a goiter may not be specific. However, weight loss, marked tachycardia, eye signs, and a bruit over the thyroid are more suggestive of hyperthyroidism.42,52
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree