The Thickened Skin Pattern
Thickening of the skin over the surface of the breast may occur in primary inflammatory carcinoma, other malignancies, and several benign conditions. It is important for the radiologist to be aware of ranges for normal thickness and to evaluate the skin carefully on the mammogram to detect an alteration that may be associated with an underlying disease process.
Although the normal skin thickness of the breast has been described as generally less than 1.5 mm (1), a study by Wilson et al. (2) of 150 normal patients showed the range to vary from 0.8 to 3 mm in thickness. In 92% of patients, the medial skin thickness was greater than the lateral skin thickness, and in 91% of patients, the skin was thicker inferiorly than superiorly. The mean thickness of the skin was greater in smaller breasts. In a study of skin thickness in 250 asymptomatic women, Pope et al. (3) found that the medial and inferior aspects of the breast skin were thickest and that the maximum thickness was 2.7 mm. Table 9.1 shows the ranges of skin thickness for different sizes of breasts as determined by Wilson et al. (2).
Edema of the breast is characterized by an increase in skin thickness and prominence of the interstitial or trabecular markings. A thickened skin pattern may occur with primary breast cancers, with metastatic carcinoma to the breast, or in a number of benign conditions (4) (Table 9.2) that cause the interstitium to be distended or edematous.
Malignant Causes of the Thickened Skin Pattern
Locally Advanced Breast Cancer
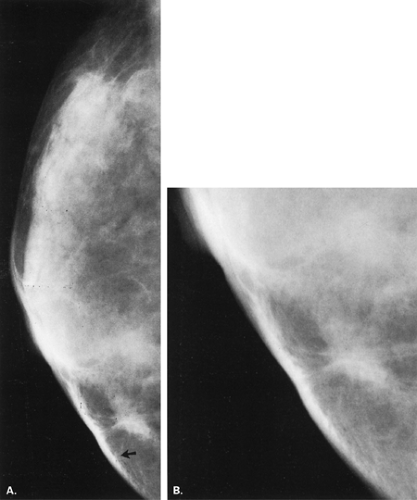
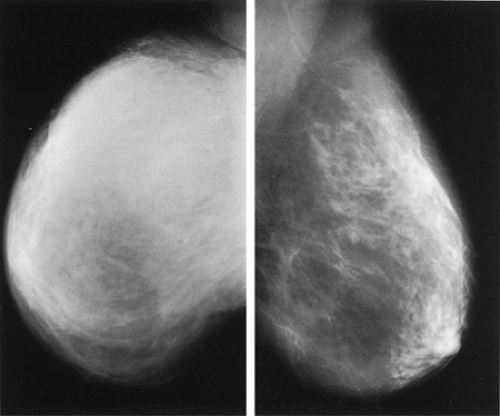
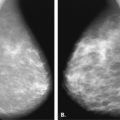
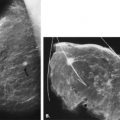
Breast cancer may extend locally into the subcutaneous fat and produce focal skin thickening and/or retraction, indicating locally advanced disease (Figs. 9.1,9.2,9.3). Dunkley et al. (5) found skin thickening on mammography in 24% of breast cancer patients; in 68% of these patients, the skin thickening seen on mammography was not evident on clinical examination. This thickening of skin is focal and is much less generalized than the skin edema associated with inflammatory carcinoma. In addition, the erythematous pitting edema of inflammatory breast cancer is not usually present in these cases.
Inflammatory breast cancer was described in Bell’s surgery text of 1816 (6,7) as “a purple color on the skin over the tumor accompanied by shooting pains.” Because of the involvement of the dermis, a diffuse edema pattern with skin thickening is seen in inflammatory carcinoma. Inflammatory cancer can account for 1% to 4% of breast cancers (8), with an average age at onset of 52 years (7). Inflammatory breast cancer is a stage IIIB, locally advanced lesion and has a poor prognosis.
In inflammatory breast cancer, the patient presents clinically with a tender, firm, heavy breast with purplish discoloration and a peau d’orange thickening of the skin. The clinical presentation is often indistinguishable from mastitis. A focal mass may be palpable, or the entire breast may be hardened. Biopsy of the skin is used to diagnose this entity; the hallmark pathologic feature is involvement of the dermal lymphatics with tumor emboli.
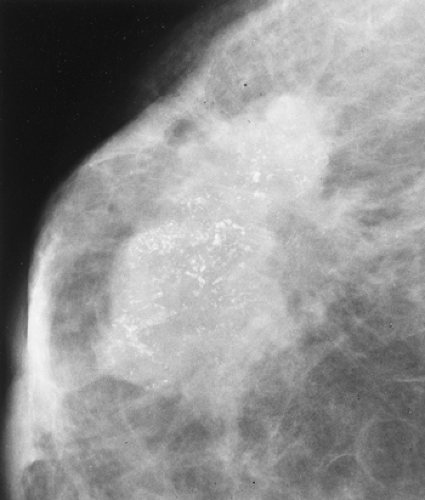
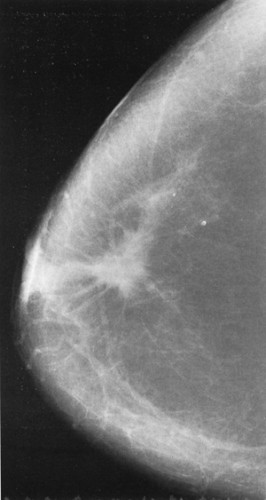
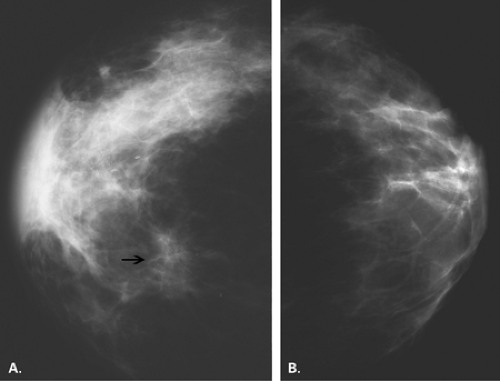
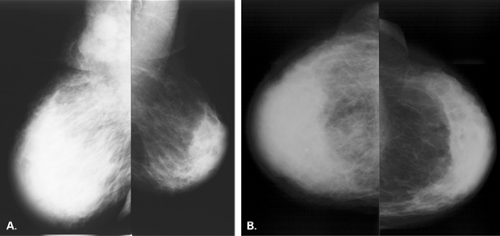
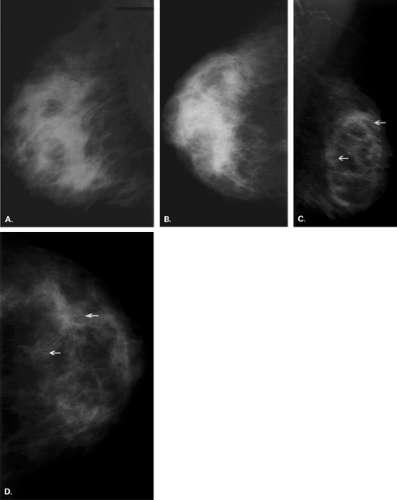
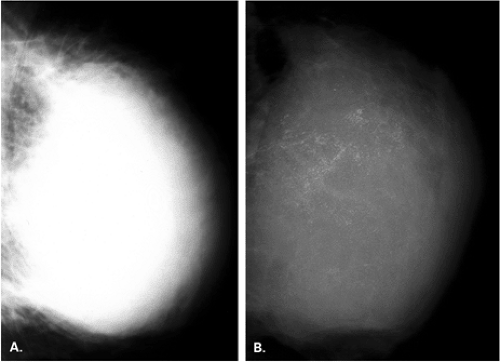
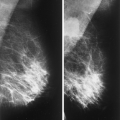
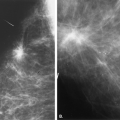
Mammographically, skin thickening and a marked increase in the density of the breast are seen (Figs. 9.4,9.5,9.6,9.7,9.8). Much of this density is caused by edematous changes in the trabeculae or interstitium of the breast. The breast affected by inflammatory carcinoma is less compressible on positioning for mammography, and the overall size of the breast on the mammogram may appear to be less than the normal breast because of its hardness and lack of compressibility. The underlying tumor mass may be evident on mammography, or the density may be so great because of the edema and the decreased compression of the thickened breast that evaluation of the underlying parenchyma is unsatisfactory.
In a review of 142 cases of pathology-proven inflammatory breast cancer, Günhan-Bilgen et al. (10) found the following manifestations on mammography: skin thickening in 84%, trabecular thickening in 81%, a mass in 16%, an asymmetric focal density in 61%, and microcalcification
in 56%. Sonography showed skin thickening in 96% and a solid mass in 80%. Ultrasound was helpful in the depiction of masses that were obscured by the edema pattern as well as in the demonstration of skin and pectoral muscle invasion and axillary involvement. In another series, Kushwala et al. (11) found that mammographic findings of skin and trabecular thickening were common (92% and 62%, respectively) and that masses and microcalcifications were uncommon manifestations of inflammatory breast cancer. Dershaw et al. (12), however, found that a vast majority of patients with inflammatory breast cancer had an edema pattern as well as an associated mass or malignant microcalcifications on mammography.
in 56%. Sonography showed skin thickening in 96% and a solid mass in 80%. Ultrasound was helpful in the depiction of masses that were obscured by the edema pattern as well as in the demonstration of skin and pectoral muscle invasion and axillary involvement. In another series, Kushwala et al. (11) found that mammographic findings of skin and trabecular thickening were common (92% and 62%, respectively) and that masses and microcalcifications were uncommon manifestations of inflammatory breast cancer. Dershaw et al. (12), however, found that a vast majority of patients with inflammatory breast cancer had an edema pattern as well as an associated mass or malignant microcalcifications on mammography.
TABLE 9.1 Range of Normal Skin Thickness | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||
TABLE 9.2 Causes of Skin Thickening | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
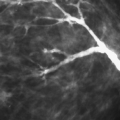
Sonography is often more helpful than mammography in identifying malignant masses in patients with inflammatory breast cancer. Sonography is also useful in defining the extent of inflammatory carcinoma, including the involvement of lymph nodes in the axillary and supraclavicular areas (13). The skin thickness can be measured on sonography, and a decrease in skin thickening can be used to quantify the response to chemotherapy (Figs. 9.9 and 9.10).
The mammographic finding of diffuse skin thickening and increase in density of the breast may be present several weeks before the clinically inflammatory signs appear (14). Keller and Herman (15) found that patients with inflammatory cancers had an average skin thickness of 6 mm and diffuse increase in density on mammography, compared with a skin thickness of 9 mm and a prominent reticular pattern in patients with a benign cause of a breast edema pattern. Patients with locally advanced breast cancer and secondary inflammatory changes may have a similar clinical presentation to those patients with inflammatory breast cancer (7)—namely, edema of the breast.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree