- The majority of people with diabetes without complications or co-morbidities can be well managed within the community; however, people with more complicated disease warrant referral to specialists.
- How to design a system to allow most patients to remain in the community, but be referred for specialist treatment at an optimum time, is one of the most important questions in organizing diabetes care. Moreover, to rationalize diabetes care, there are many areas that will need decision-making regarding who is to do what, and at which level. There is no single correct answer as the local situation will influence the decision.
- On a worldwide basis, community care of diabetes by primary care providers is likely to provide the backbone of diabetes treatment. How to improve and support care at this level, and to what extent, is an important strategic question. If it is improved to a specialist level then its cost advantages would be minimized.
- In many areas of the world, specialist care is provided by a hospital, often characterized by a large inpatient unit supported by outpatient clinics. Provision of continuity of care for a chronic disease such as diabetes within hospitals and clinics is a task warranting a great deal of attention.
- Diabetes educators or specialist nurses can complement and enhance what doctors provide. Non-medical staff can be trained to make clinical decisions about the management of diabetes, including the management of glycemic control, hypertension and dyslipidemia, provide self-management education and coordinate team services to meet the patient’s health needs, thereby taking the load from the medical staff to allow them to concentrate on more complex cases.
- In some areas of the world, diabetes education centers have been developed to support large diabetes clinics. Staff within these centers have core clinical knowledge of diabetes, as well as understanding teaching and learning principles and behavioral and psychologic strategies to help patients manage their diabetes.
- Some diabetes centers provide integrated specialist diabetes care. Clinical activities undertaken by these centers often include initiation of insulin therapy and stabilization of diabetes without need for hospitalization, screening and management of diabetes complications, management of diabetic foot disease, diabetes in pregnancy, neuropathic pain and insulin pump therapy. This “Rolls Royce” model is expensive and cannot care for every person with diabetes. It must concentrate its role in complementing, not duplicating, what the community doctors can provide. It also has a role in educating community doctors and health care professionals while demonstrating what needs to be done and can be achieved.
- Timely communication is crucial in promoting a seamless interface between community and specialist levels of care. This is most important in improving the skills of primary care health providers, and it involves more than just providing factual information on the level of HbA1c and insulin dosage.
Introduction
The World Health Organization’s Declaration of Alma Ata, adopted in 1978, expressed the need to protect and promote the health of all peoples of the world. The Declaration highlighted the inequity between developed and low and middle income countries. Despite the number of decades that has passed since this Declaration, providing appropriate care for all people with diabetes remains problematic. Conclusive evidence now exists that the devastating complications of diabetes can be minimized by timely and effective treatment; however, even in developed countries, with universally funded health services, large proportions of people with diabetes are not routinely monitored either for diabetes or its complications [1]. This is especially so for people living in rural areas [2–5], or for those who are socially disadvantaged [6]. This means that the opportunity to commence early treatment is missed. Today it is estimated that only 5% of people living with diabetes around the world receive optimal care [7]. While clinicians endeavor to provide the best possible treatment, there are often serious limitations stemming from resource availability and/or inadequate models of care.
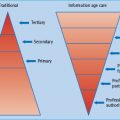
Globally, the spectrum of diabetes services varies from a single health care provider working in an isolated community setting, to small groups of primary care doctors and nurses working in health centers or district hospitals, through to highly sophisticated tertiary units in major urban areas with access to a range of specialists, nurses and other diabetes team members. In this chapter we explore how diabetes care may be best delivered at these various levels, taking into consideration political, cultural and economic environments. Not every case of diabetes can be looked after at the community level. Likewise, not every case of diabetes can be managed at the specialist level. How to support and to balance these two extremes is one of the most important questions in organizing diabetes care.
Primary care for diabetes
Primary care in the community forms an integral part of health care in most countries and is the first level of contact for most people with diabetes. The sheer number of people with diabetes would dictate this to be a necessity. How we improve diabetes care at this level is therefore a matter of great importance. What is considered primary care may vary a great deal between countries, or within regions of the same country. Likewise, improving primary care for diabetes may take on different meanings in different settings.
On a world basis, primary care is usually provided by a doctor, acting alone and almost invariably also treating many other diseases. In many ways, diabetes is just a condition that the patient “happens to have,” and its management can be surreptitiously relegated to a lesser role than the problem of the day. Various attempts have been made to overcome these issues, and it is beyond the scope of this chapter to outline them all, but some examples are mentioned here.
In many countries, primary care is delivered through a system of health centers or clinics which are scattered throughout urban and rural areas. Appropriately supported, these centers can provide routine diabetes management to most people with diabetes within a local area, but require the ability to refer more complicated cases, such as patients with newly diagnosed type 1 diabetes mellitus (T1DM) or those with an active foot problem.
The success of this approach was exemplified by a randomized cluster trial conducted in the Torres Strait, which is located between Australia and Papua New Guinea, and inhabited by indigenous Australians scattered over a wide area in small communities [8]. The study aimed to implement a sustainable system of care by providing basic training in clinical diabetes care to local indigenous health workers employed in randomly selected health centers. The study team also assisted local staff within these centers to establish diabetes registers and recall systems, and to develop diabetes care plans. Diabetes specialist outreach services were established concurrently for all health centers within the Torres Strait, and were designed to facilitate referral and provide care for individuals with more complicated disease. It also provided a secondary benefit for local staff to learn up-to-date diabetes management principles through working alongside the diabetes specialist during visits to the health centers. It was found that diabetes care processes improved in all health centers and the intervention sites showed greatest progress, with significant improvements in weight, blood pressure and glycemic control measures. Moreover, people with diabetes managed by the intervention clinics were 40% less likely to be admitted to hospital for a diabetes-related condition. Over time, local service providers have assumed increasing responsibility for routine diabetes care, thus ensuring sustainability of the service.
The ability of organizational change to improve diabetes care processes and clinical outcomes at the primary care level has been further emphasized by the recently reported TRANSLATE trial [9]. The multicomponent organization intervention adopted within this trial, which included implementation of an electronic diabetes registry, visit reminders and patient-specific physician alerts, resulted in a significant increase in the proportion of patients achieving recommended clinical outcomes.
Tanzania provides a further example of implementing a well-organized system of care at the community level. Prior to 2004, for a general population of 39 million, specialized diabetes care was available in just five referral hospitals nationally, and was provided by a handful of consultant physicians and diabetes educators. Access to diagnosis and treatment, particularly in rural areas, was extremely limited. With support of the Ministry of Health and the Tanzanian Diabetes Association, teams of health care workers from all regional hospitals, comprising a doctor, two nurses and a laboratory technician, were offered comprehensive diabetes training programs. After training, each team was given a starter kit containing diagnostic and educational tools in order to help establish services. By 2006, 29 diabetes clinics had been established, providing accessible and affordable treatment and education services to more than 100 000 people [5]. This model of care is consistent with the World Health Organization’s aim of sustainable interventions by helping countries develop their own infrastructure and professional expertise in health care. It will enable Tanzania to continue to progress independently towards providing sustainable and accessible diabetes care in the long term, and can serve as a model for other low and middle income countries.
Since 1993, general practitioners (GPs) in the UK have been encouraged to develop services for diabetes, with a specific payment for doctors offering structured diabetes care. As a result, the proportion of people with diabetes reviewed annually in primary care has increased. Interestingly, Norway also report improvements in processes of diabetes care over a similar time period, without additional incentives for GPs to follow national guidelines. In the case of Norway, the improvement was attributed to ongoing medical education [10]. In Germany, a diabetes management program was introduced in 2003, the core content of which was defined by a national expert panel. Program initiatives included the use evidence-based guidelines and the development of a basic data set, establishment of quality indicators, as well as recall of patients. Fulfilment of program recommendations is compulsory for contracts between health insurers and service providers. By mid-2007, approximately 50% of the estimated population with diabetes, and approximately 65% of family practices, had enrolled in the program. A recently reported survey showed that patients being managed under the program perceived improved care [11].
In Australia, the government funds a chronic disease management program in general practice. Under this program it has been made easier financially for GPs to employ a practice nurse to help with various tasks of managing patients, including but not exclusive to diabetes. Many doctors use these practice nurses to complete the annual cycle of diabetes care, which includes periodic examination of the feet, and ensuring other diabetes complications and metabolic variables are regularly assessed. In recognition of the fact that GPs often encounter difficulties in securing the services of allied health professionals for their patients, the Australian government has also begun a subsidy, through the universal health insurance system, for five allied health visits a year, and made such referrals the prerogative of GPs only. These initiatives are obviously in the right direction from the individual doctor’s and patient’s point of view. Conceptually, they are elevating primary care for a particular disease to a level close to specialist care. Whether this is true primary care or just specialist care in another guise is debatable. The irony for the health care planner is that if primary care for diabetes becomes progressively better, it may become progressively more like specialist care and thus lose its cost–benefit advantage. Whether this move would translate into better clinical endpoints and provide overall cost–benefits for the treatment of diabetes for the entire community needs to be evaluated.
Traditional specialist care
Hospital clinic
In many areas around the world most diabetes care is provided by a hospital, often characterized by a large inpatient unit supported by outpatient clinics. While some hospitals have diabetes-specific outpatient services, many people with diabetes are seen within the context of a large general medical clinic. Although specialists are often nominally in charge in this setting, and the clinic is considered a specialized diabetes clinic, much of the time the duty of actually seeing people with diabetes is delegated to junior and rotating medical staff. Typically, nursing staff undertake process tasks such as preparing medical records, measuring the patient ‘s height and weight, and testing blood glucose levels. Many of these clinics are not formatted to cope with caring for people with a chronic disease, and entrenched but unsuitable systems, often as a result of hospital regulations, such as only providing patients with a few weeks’ supply of medications, mean that clinics are overwhelmed by people attending to have a prescription written. This ultimately leads to shorter consultation times to cope with increased throughput of clinic attendees. As a consequence, care tends not to be patient-focused nor up-to -date, resulting in poor clinical outcomes.
Simple policy changes can improve diabetes care without imposing too much of a cost penalty. For example, if the rationale for writing monthly (or even shorter) prescriptions is because of cost or supply chain issues, doctors can write a prescription valid for several months that can be dispensed monthly by the hospital pharmacist. This will free up the clinic considerably. Another example that can improve continuity of care is to link the rotating junior doctors’ clinics with someone more permanent. At least patients will see someone familiar, and if they have a particularly difficult diabetic problem (be it medical, such as insulin allergy, or psychosocial, such as poor family support), at least the junior rotating doctor could be told beforehand about it by the senior consultant who is next door.
A further step that can improve diabetes care within the traditional system is to allocate nurses to the specialized position of diabetes educator or diabetes specialist nurse, so they can complement and enhance what the doctors provide. For this to be successful, it is important their roles are separate to the clinic nurse, and not just be seen as “an additional pair of hands” to help with routine clinic or ward duties. Rather, they should be employed to provide education regarding self-management principles to either inpatients or outpatients, or a combination of both. In some cases their role may be fully dedicated to educating patients; however, with further training, the specialist nurse can well provide many areas of diabetes management [12–16]. These staff can be trained to make clinical decisions about the management of diabetes, including management of glycemic control, hypertension and dyslipidemia, provide self-management education, and coordinate team services to meet the patient’s health needs. Utilizing nursing staff to provide many of the routine clinical services is less expensive than using medical staff, and takes the load from the medical staff so they can concentrate on more complex cases. Indeed, studies comparing clinical outcomes from protocol driven, nurse-l ed clinics with traditional physician-l ed clinics have shown care is no worse in a nurse or allied health driven system [13–16]; however, the success of this approach may lie in the careful selection of staff. Recognizing the advanced skills of the diabetes specialist nurse, both through a career structure and improved financial incentives, is important to ensure continuity of staff. There is also a need to convince nursing and hospital administrators of the importance of the specialist nurse role so that trained staff are permanently maintained within their specialist area.
Traditional diabetes clinics have often been considered to be antiquated. However, they can be made to work, and realistically they are likely to remain the backbone of specialist diabetes care worldwide. However, for them to be effective, there are organizational and system issues to which the senior doctor in the clinic must pay attention, rather than limiting his/her role to a medical one only.
Private specialist diabetes care
In many areas around the world, a system of private specialist diabetes care exists to offer choice and to reduce some of the burden on public funded services. Subsidy or insurance of private health services is often available, but patients may be faced with a co-payment if their diabetes practitioner charges above the subsidized fee. These costs are a major barrier to many patients receiving the level and type of care they require [17], particularly when multiple specialists are involved. In the majority of cases, private services are run by solo practitioners, and access to support services provided by allied health professionals is also costly. In many ways, similar to their primary care counterparts, the private specialists face the same difficulty of providing multi-disciplinary care required by some patients with diabetes.
Integrated specialist care
Specialist diabetes care can also be provided in a more integrated and multidisciplinary manner, addressing not only glucose control, but also complications and co-morbidities of diabetes, involving doctors as well as allied health professionals. The health and cost benefits of such integrated specialist care have been reported by the Steno Hospital [18–26], although it is difficult to evaluate the magnitude of benefits by controlled clinical trials. It is also not clear how much of the reported benefit was brought about by multidisciplinary involvement, and how much by multifaceted treatment.
Such integrated care is often conveniently provided at a diabetes center, an entity that is distinct from the diabetes clinic. To appreciate the full potential of a diabetes center, it is worthwhile noting its heterogeneous nature. Although many facilities may function under the same generic name, they can differ quite considerably. Initially, the role of diabetes centers was to provide diabetes education. For many this remains their primary function, and diabetes education center is perhaps a more appropriate name. These education centers have generally been developed to support large diabetes clinics, and are usually located separately from where medical consultations are made. In this model, clinical care is provided by physicians and patient self-management education is conducted by other diabetes team members. These team members need to have core clinical knowledge of diabetes, understand teaching and learning principles, as well as behavioral and psychologic strategies to help patients to manage their diabetes. It is a system of care repeated in many countries around the world, and can be highly successful in meeting the clinical, educational and psychologic needs of the person with diabetes and their family.
Toward the other end of the spectrum, a diabetes center can incorporate clinical activities. In this manner the duties of doctors and other health professionals become more integrated, co-located and co-dependent. This is the model we have relied on extensively at Royal Prince Alfred Hospital in Sydney for the last two to three decades. Initially, a prime motive of such initiatives was initiation of insulin therapy and stabilization of diabetes without the need for hospitalization, duties largely provided by diabetes nurses, but with the backing of doctors. Over the years more specialized clinical services, such as screening and management of diabetes complications, diabetic foot disease, diabetes in pregnancy, neuropathic pain and use of insulin pump treatment have been progressively added to the services provided by our diabetes center. In many of these activities, nursing and allied health professionals have such a specialized role that the doctor’s function can become a supporting as well as a supervisory one. We have found nursing and allied health professionals to be better in these roles than rotating doctors, if for nothing else because patients appreciate more continuity. Conceptually, there is no reason why one good doctor cannot provide all these services to their patients, and we have indeed witnessed some who were able to do so, but in our experience it is logistically difficult. In many ways, in our system there are many specialists that make up the team, but not all of them are doctors. This concept, for example, of a nurse being more “specialized” in a clinical area of diabetes management than a doctor, is sometime difficult for the traditionalist to understand, or with which to feel comfortable.
To provide such specialized services, diabetes center staff members require ongoing training which is at one time more specialized, and yet also broader in scope, philosophically identical to that required by their medical counterparts undergoing specialist training. For example, in addition to understanding general diabetes and dietary principles, dietitians working in a clinical diabetes center need to be expert in insulin adjustment and hypoglycemic unawareness in order to be able to help a patient who is learning carbohydrate counting. Another example is the nurse who is helping the patient to adjust insulin dosage. Such nurses must be familiar with the findings of recent clinical trials such as the ACCORD Study [27] to individualize the level of glycemic control required by that individual.
By its very “Rolls Royce” nature, this type of integrated specialist diabetes care is more resource hungry. By creating such “super centers” there will be constant ambivalence between balancing state of the art services and providing day-to-day diabetes care to a large number of people. Because of resource constraints, this will always be a problem, and it is even worse for a unit that is dependent on throughput for its funding. This dilemma will necessitate a rational debate of who needs specialist care and what this entails.
Sharing the burden of diabetes between community care and specialist care
Many aspects of diabetes management can be very capably provided at the community level [28,29]. It therefore makes sense for the majority of patients without complications or co-morbidities of diabetes to be managed within the community; however, patients with more complicated disease warrant referral to specialists, depending on their individual need. For containment of cost, not surprisingly, virtually all governments embrace this position.
While conceptually sound and obvious, a seamless delivery for such a division of labor is not easy to achieve. It is relatively easy for primary care doctors to notice poor glycemic control. By contrast, patients with complications or risk factors of complications, but who are unaware of their existence, do not readily identify themselves. Various guidelines from learned bodies therefore promote the concept of regular screening for diabetes complications. In Australia, the government rewards primary care doctors with additional remuneration if a patient with diabetes has completed a cycle of care, including assessment for glycemic control and diabetes complications, within a certain timeframe. This push towards primary care, coupled with the natural expectation of a better standard of care, would increase the use of specialized services such as ophthalmology and podiatry, amongst others. Ironically, much of the cost saving of seeing a primary care doctor rather than a specialist may be lost in this manner.
Improving synergism between primary and specialist care
A possible solution is the system we have used at the diabetes center of the Royal Prince Alfred Hospital in Sydney. We rely on a shared care system to partition responsibilities between primary care doctors and specialists, and have established a complication assessment service to underpin such a sharing arrangement [29]. In one visit, patients referred by primary care doctors have examination of the fundi, testing of foot sensation and reflexes, quantitation of albuminuria, assessment of lipid profile and other cardiac risk factors, as well as examination of pedal and carotid pulses. This allows the primary care doctors to provide routine diabetes management for the majority of patients, and to make appropriate referrals to specialists when necessary.
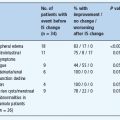
A recent study comparing outcomes of patients managed by our model with those of patients attending traditional specialist services found that the adherence to management guidelines in our shared care model was superior to traditional specialist care. Moreover, a significantly higher proportion of patients managed under the shared care model, achieved an HbA1c within 1% (11 mmol/mol) of normal range, and/or a blood pressure at target [30]. This would suggest that the majority of people with diabetes do not need to see a specialist service in the traditional 3–4 monthly cycle to receive similar quality of care. Apart from achieving good endpoints of glycemic control and complication detection, this system is more cost effective because specialists services such as ophthalmologists and nephrologists are generally only sought when recommended by a diabetes specialist.
It is worthwhile to note particular issues that can make such a system maximally effective. The specialist team that examines the patients and reports to the primary care doctor must have good clinical skills and judgment in managing the various complications of diabetes. This will allow diabetes specialists to provide more precise recommendations about the timing of referrals to other specialists, or indeed to provide appropriate treatment of some complications themselves. For example, the ability of the diabetes specialist to recognize not only retinopathy in a particular patient, but also be confident that it is not vision-threatening for the foreseeable future, may appropriately delay the referral to an ophthalmologist until later. It also offers a cost advantage. During 2008, our center screened over 2400 patients, 237 of whom were found to have retinopathy. The cost to the health system for the screen-negative patients to have been seen by an ophthalmologist would have been close to $AUD150 000. A further example is the ability to identify the occasional patient with non-diabetes-related neuropathic pain; this may save many other patients with typical diabetes neuropathic pain from unnecessary referral to neurologists.
To maximize the effectiveness of this system further, the diabetes center team must also know what a particular primary care doctor is capable of, or willing to do, in the management of diabetes. This will help to decide how much of the care of a patient should be returned to the primary care level. This differential approach to shared care cannot be easily written in a guideline, and can only be established through years of contact with primary care doctors in the community.
There are many other approaches to facilitate complementary primary and specialist diabetes care. For example, telemedicine has been shown to be a useful tool in linking community health services with specialist services. At our center, telemedicine is used in the management of diabetic foot disease, and facilitates routine and urgent consultations between our urban diabetes center and rural sites. Routine consultations are organized by prior arrangement without the patient needing to be present. The process includes the advanced emailing of standardized digital images of the patient’s foot for the center’s foot team to review before phone linkup. The images are displayed on computer monitors at both sites during the phone linkup and a patient management plan developed, which is then implemented locally. Urgent consultations are booked on demand, and at least one person from the diabetes center foot team is available for immediate advice until further review can be arranged. This system minimizes unnecessary patient travel, facilitates routine clinical care, and allows for urgent consultations, as well as providing ongoing training for community health professionals regarding diabetic foot disease. Such a system has the potential for use in countries where diabetic foot services are limited [31]. Another example is the development of mobile diabetes buses in India [32]. Retinal photographs taken in rural locations are beamed by satellite to specialist diabetes services for their opinion regarding the need for laser therapy. This service is financially supported by local charities and donations from other international organizations, and involves partnerships with government satellite organizations and private medical centers.
Rethinking diabetes care
To rationalize diabetes care, decisions will need to be made in many areas regarding who is to do what, and at which level. There is no single correct answer, since the local situation influences the decision; nevertheless some pertinent examples and relevant points can be raised. For example, emotion would often dictate that the management of gestational diabetes should be at the specialist level; however, the large numbers of women with this diagnosis has the potential to overwhelm diabetes pregnancy clinics. This places increased pressure on staff, and means that women with pre-existing T1DM and type 2 diabetes mellitus (T2DM) may not receive the level of care they need. The morbidity of gestational diabetes is relatively low in comparison with T1DM and T2DM. A better use of resources would be to provide the care for women with gestational diabetes in the community, with appropriate protocols and guidelines to ensure referral to specialist services as required.
Treatment of diabetic foot disease is another example of how care between the community and the specialist services needs to be carefully partitioned, depending on the individual’s degree of risk. Guidelines often suggest that all those with diabetes should have their feet assessed and managed by podiatrists. This will place great stress on the availability of podiatrists when their service is better directed to high risk individuals, especially those with active foot lesions. It is better to assign the level of care depending on whether a patient has risk factors for foot ulceration, such as impaired sensation or peripheral circulation, and whether there are active foot lesions. This would allow patients with foot ulceration, severe foot infection and Charcot arthropathy to receive the specialized attention they need.
The care of people with T1DM is challenging. They need more multidisciplinary care, such as dietary counseling of carbohydrate counting or intensive teaching in the use of insulin infusion pumps. These skills are not readily available in the community. The lower prevalence of T1DM also means that most primary care doctors do not have enough exposure to this group of patients to gain experience. Therefore, this group of individuals is probably better managed at the specialist level.
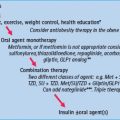
There is also the broader (and economically the most important) question of who should look after the glycemic control for the majority of people with T2DM. There is a great deal of uncertainty about the optimal line of division between primary care and specialist care, both from medical and economic points of view. A reflection of this uncertainty is the ongoing debate on how guidelines on the treatment of T2DM should be framed. There are some who believe that an HbA1c target of <7% (<53mmol/ mol) should be adopted because, amongst other reasons, this is what can reasonably be expected at the primary care level. Others believe that this approach is not individualized enough, and could potentially discourage specialists and patients from aiming for even better glycemic control, even when it is appropriate.
Communication between primary and specialist care
Timely communication is crucial in promoting a seamless interface between primary and specialist care. In our system, we have relied for many years on a report that is a hybrid of a computer report, containing numerical and factual data, supplemented by three free text messages addressing issues related to, respectively:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree