The Nervous System and Diabetes
Roy Freeman
Most recognized neurologic complications associated with diabetes involve the peripheral nervous system, and it is these that will be emphasized in this chapter. The diabetic neuropathies include several distinctive clinical syndromes with differing clinical manifestations, anatomic distributions, clinical courses, and possibly underlying pathophysiologies.
Disorders of the nervous system associated with diabetes have long been recognized. Rollo is credited with having recorded this association in 1798, and until the middle of the 19th century, diabetes itself was attributed to a primary disorder of the central nervous system. It was Marchal de Calvi in 1864 who first suggested that diabetes might be the cause rather than the effect of neuropathy (1,2). Pavy’s (3) description in 1885 of neuropathic symptoms is noteworthy for its completeness.
The usual account given by these patients is that they cannot feel properly in their legs, that their feet are numb, that their legs seem too heavy—as one expressed it, “as if he had 20 pound weights on his legs, and a feeling as if his boots were a good deal too large for his feet.” Darting or “lightening” pains are often complained of. Or there may be hyperesthesia, so that a mere pinching of the skin gives rise to great pain; or, it might be, the patient is unable to bear the contact of the seam of a dress against the skin on account of the suffering it causes. Not infrequently there is deep-seated pain, located, as the pain describes it, in the marrow of the bones, which are tender on being grasped; and I have noticed that these pains are generally worse at night. With this there is the usual loss or impairment of the patellar tendon reflex.
CLASSIFICATION
There are several diabetic neuropathies. The most commonly used classification is based on the clinical presentation. Because the understanding of the etiology and pathophysiology of the diabetic peripheral neuropathies is incomplete, current classifications are based primarily on clinical manifestations. Many patients do not manifest a single type of diabetic neuropathy but rather a mixture of neuropathic features often dominated by one or another subtype.
Historical classifications begin with Leyden (4) who described hyperesthetic, paralytic, and ataxic forms of neuropathy. Jordan (5), on the basis of observations of patients treated at the Joslin Clinic, recognized three types of neuropathy: (a) a “hyperglycemic” type dominated by sensory symptoms, without neurologic signs, that was usually reversed by treatment of diabetes; (b) a chronic “circulatory-degenerative” type with advanced sensory, motor, and reflex abnormalities associated with arterial insufficiency of the legs; and (c) a “neuritic” type characterized by more-acute neuropathic symptoms and signs. In a similar classification Treusch (6) described (a) diabetes with pain in which control of diabetes improved symptoms, (b) ischemic neuropathy, (c) diabetic polyneuritis, and (d) visceral neuritis. Goodman et al. (7) listed (a) function neuropathy with uncontrolled diabetes without neurologic deficit, (b) organic neuropathy with neurologic signs and, (c) posttreatment neuropathy. These classifications all have the disadvantage of mixing clinical and uncertain pathophysiologic criteria. Locke (8) proposed a simpler anatomic classification system in which lesions of nerve roots produce radiculopathy; lesions of mixed nerves produce polyneuropathy.
More recent classifications continue to emphasize topographic body distribution (9) and are summarized by Dyck’s classification (10) into (a) symmetric distal polyneuropathy with sensory, or sensorimotor motor involvement; (b) symmetric proximal lower limb neuropathy; (c) asymmetric focal neuropathy including cranial, truncal, limb plexus, multifocal entrapment, and ischemic neuropathies; (d) asymmetric neuropathy combined with symmetric distal polyneuropathy; and (e) mixed forms.
Perhaps the simplest and most widely used classification was initially proposed by Thomas (11). This approach divides the diabetic neuropathies into diffuse, generalized, or symmetric polyneuropathies (sensory, motor, and autonomic) and focal neuropathies (mononeuropathy, mononeuropathy multiplex, plexopathy, radiculopathy, and cranial neuropathy). A modification of this classification is shown in Table 56.1.
TABLE 56.1. Classification of Diabetic Neuropathy | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
SYMMETRIC NEUROPATHIES
Generalized Polyneuropathy
EPIDEMIOLOGY
Predominately sensory or sensorimotor distal polyneuropathy is the most common of the diabetic neuropathies. Epidemiologic studies suggest that the prevalence of diabetic peripheral neuropathy ranges from 5% to 100%. This large range is in part a consequence of variations in the study population, patient selection, the diagnostic criteria for the diagnosis of diabetes, the sensitivity of methods used to detect peripheral neuropathy, and the duration of diabetes in the study cohort. Diabetic peripheral neuropathy is more prevalent in tertiary care centers and diabetes clinic populations, where patients are more likely to have complications than are patients in the community. Similarly, prevalence is typically higher if ascertainment is based on electrophysiologic measurements, autonomic testing, or quantitative sensory testing and lower if it is based on subjective symptoms and physical findings. The prevalence of neuropathy also increases with age and increasing duration of diabetes.
In a large population-based epidemiologic study, Pirart (12) followed a cohort of 4,400 patients from 1947 to 1978 and, using clinical criteria, found evidence of neuropathy in 7.5% of patients at the time of diagnosis. The prevalence of neuropathy increased to 50% after 25 years of follow-up. In a controlled, longitudinal study of 132 patients with type 2 diabetes, Partenen et al. (13) documented the progression of polyneuropathy diagnosed using clinical criteria (pain and paresthesias) and electrodiagnostic studies. The prevalence of nerve-conduction abnormalities in the legs and feet increased from 8.3% at baseline to 16.7% after 5 years and to 41.9% after 10 years. The decline in sensory and motor action potential amplitudes was more prominent than the slowing of nerve-conduction velocity. After 10 years, more than 40% of patients no longer had ankle reflexes and 20% had vibration loss.
Several cross-sectional studies have examined the prevalence of diabetic polyneuropathy. In the Rochester diabetic neuropathy cohort, the prevalence was 54% in patients with type 1 diabetes and 45% in patients with type 2 diabetes (14). In the EURODIAB IDDM Complications Study, the prevalence of peripheral neuropathy in 3,250 randomly selected patients with insulin-dependent diabetic was 28% (15). Similar prevalences were reported in the Pittsburgh Epidemiology of Diabetes Complications Study (16), the multicenter, diabetic clinic-based study on the prevalence of diabetic neuropathy in Italy (17), and in a multicenter study of diabetic patients in the United Kingdom who were attending hospital-based diabetic clinics (18).
RISK FACTORS
Hyperglycemia is now well established as a risk factor in both patients with type 1 diabetes (19,20) and patients with type 2 diabetes (13). Other correlates and associations include age, duration of diabetes, quality of metabolic control, height, the presence of background or proliferative diabetic retinopathy, cigarette smoking, high-density lipoprotein cholesterol, and the presence of cardiovascular disease (15,16,18,21).
CLINICAL FEATURES
Numbness and paresthesia begin in the toes and gradually and insidiously ascend to involve the feet and lower legs. Sensory deficit usually occurs symmetrically in the distal territory of overlapping nerves, but not infrequently, asymmetric patterns of sensory loss in root or nerve distribution may be superimposed on this distal symmetric pattern of sensory loss. Because the distal portion of longer nerves are affected first, the feet and lower legs are involved before the hands, producing the typical “stocking-and-glove” pattern of sensory deficit. In most patients, the symptoms of polyneuropathy are mild and consist of numbness or paresthesia of the toes and sensory disturbances often described as “like walking on pebbles” or “having cotton bunched up under the toes.” In some patients, “positive” symptoms are present. These include superficial burning, paresthesia, deep aching pains, dysesthesia, contact-induced discomfort, and paroxysmal jabbing pains. These symptoms are typically more severe at night. In more severe cases, distal portions of thoracic intercostal nerves are affected, producing an asymptomatic midline sensory loss in a teardrop distribution over the anterior thorax and abdomen that gradually spreads laterally (22). A similar pattern of deficits that gradually increase in size may occur on the vertex of the scalp and the central aspect of the face. This thoracic and abdominal sensory loss differs from focal thoracic truncal radiculopathy (23,24,25) in that it manifests as a painless, bilateral, symmetrical, and persistent form of neuropathy. Impaired touch and two-point discrimination in the fingertips may interfere with the reading of Braille (26). Sensory symptoms and signs are commonly accompanied by mild distal weakness and features of autonomic neuropathy.
Both lightly myelinated and unmyelinated small nerve fibers and the myelinated large nerve fibers are affected (Table 56.2). Dysfunction of small and large fibers occurs in varying combinations; however, in most cases the earliest deficits involve the small nerve fibers. Features characteristic of a small-fiber peripheral neuropathy include deficits in pain and temperature perception, paresthesias and dysesthesias, pain, deficits in the perception of visceral pain, dysautonomia, and predisposition to foot ulceration. Proprioception and deep tendon reflexes are relatively preserved. Nerve-conduction studies may be normal or minimally abnormal when small-fiber features dominate since these measurements are dependent on conduction in the surviving large, myelinated nerve fibers. This presentation, which resembles the dissociated sensory deficits that accompany as syrinx, has been described as pseudosyringomyelic. In contrast, features characteristic of large-fiber
peripheral neuropathy include loss of position and vibration perception sense and loss of deep-tendon reflexes. Nerve-conduction studies are usually abnormal. This presentation, which has features in common with the pattern of deficits that are associated with tabes dorsalis, has been termed pseudotabetic.
peripheral neuropathy include loss of position and vibration perception sense and loss of deep-tendon reflexes. Nerve-conduction studies are usually abnormal. This presentation, which has features in common with the pattern of deficits that are associated with tabes dorsalis, has been termed pseudotabetic.
TABLE 56.2. Features of Small- and Large-Fiber Neuropathy | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Marked distal muscle weakness with sparing of sensation occasionally occurs but often is due to mononeuropathy multiplex involving the peroneal or ulnar nerves. A pure or predominant motor polyneuropathy with few or no sensory symptoms or signs is rarely due to diabetes and should trigger a search for alternative causes of weakness, such as motor neuron disease, primary muscle disease, spinal cord disease, or other potentially treatable causes of peripheral neuropathy, such as chronic inflammatory demyelinating polyneuropathy (27). Once established, sensory and sensorimotor distal neuropathy is a permanent condition; although the course of painful manifestations is highly variable: It may last for months to years and may be exacerbated by intercurrent illness, infection, and depression. In one report, 36 patients with pain for at least 12 months showed no significant change in symptoms over a mean follow-up period of 4.7 years (28).
Although selected large-fiber neuropathies might be expected to cause muscle weakness, painless loss of vibration and position sense, and impaired tendon reflexes, pathologic (29,30), clinical (31), and quantitative sensory studies (32) have not demonstrated pure loss of large fibers in diabetic peripheral neuropathy (33). However, patients with disproportionate large-fiber involvement may manifest muscle weakness, atrophy of the intrinsic foot muscles, and weakness of the extensors and flexors of the toes and ankles with foot drop. When these deficits are combined with proprioceptive deficit in the toes and feet, a “pseudotabetic” gait ataxia may result. Neuropathy of this severity often coexists with diabetic retinopathy and neuropathy.
FOOT ULCERATION
Foot ulceration and neuropathic arthropathy are two of the more dreaded neurologic complications of diabetic neuropathy. Foot ulcers usually occur in patients with either small- or large-fiber neuropathy. Painless ulcers in weight-bearing areas occur on a background of insensitivity to pain, impaired pro prioception, atrophy of intrinsic foot muscles, and the consequent maldistribution of weight-bearing, disturbed sweating, impaired capillary blood flow caused by autonomic neuropathy, and noninflammatory edema. Deformity of the foot due to muscle weakness and atrophy produces a maldistribution of weight-bearing and results in callus formation (34,35,36,37). The importance of a careful neurologic examination with careful attention to foot sensation cannot be overemphasized (38). The foot that is at risk for ulceration may be determined simply using the Semmes–Weinstein monofilaments (39).
Neuropathic arthropathy (Charcot joint or diabetic osteo arthro pathy) is a rarer complication. This occurs primarily in the metatarsophalangeal and metatarsal-tarsal joints and is believed to be due to a combination of impaired deep pain, proprioceptive sensibility, and autonomic neuropathy. A good blood supply appears critical to the development of this complication (40). Trauma, even of a minor nature, or foot surgery may precipitate a Charcot joint. In addition, recurrent trauma may cause pathologic fractures of metatarsal bones with progressive external rotation and eversion deformities of the foot (35,41).
Acute Painful Neuropathy
Acute painful neuropathy (42) is a variant of sensory polyneuropathy in which severe burning pain of the extremities is combined with deep aching pain in proximal muscles, jabs of pain radiating from the feet to the legs, and striking hypersensitivity or allodynia of the extremities and trunk to touch, clothing, or bed sheets that is often likened to sunburn. Objective sensory deficit is surprisingly mild in comparison with the painful paresthesia and dysesthesia. Nerve-conduction velocities are frequently normal or minimally abnormal.
Anorexia, weight loss, and depression are often so prominent that the term “diabetic neuropathic cachexia” as coined by Ellenberg (43) to describe this syndrome. This syndrome often correlates poorly with severity of diabetes or presence of other diabetic microangiopathic complications. Prognosis may be good in some patients, with gradual recovery over a period of months (42), particularly if the onset of symptoms follows a metabolic disturbance (44). The condition appears more commonly in males (45). Recurrent episodes may occur infrequently (46).
Treatment-Induced Neuropathy
Sensory neuropathy sometimes appears for the first time coincident with treatment with insulin or oral hypoglycemic agents (47,48) and has been referred to as a treatment-induced neuropathy (49). Although the cause is unknown, it has been suggested that improved glycemic control may initiate regenerating axonal sprouts, which generate ectopic nerve impulses (49). Alternately, it has been proposed that the pain is due to changes in the epineurial vasculature, such as arterial attenuation and tortuosity, arteriovenous shunting, and neovascular proliferation (50). There is usually gradual improvement as treatment continues and glycemic control is maintained.
Hyperglycemic Neuropathy
“Hyperglycemic” neuropathy refers to widespread paresthesias of the extremities and trunk that occasionally occur in patients with newly diagnosed or poorly controlled diabetes and that rapidly improve with control of hyperglycemia. The unique reversibility of this form of neuropathy and the diffuse rather than distal distribution of paresthesias suggest a pathophysiologic basis different from that for later-appearing diabetic sensory neuropathy. In an experimental model of diabetes, acute hyperosmolar hyperglycemia was associated with reduced nerve-conduction velocity and axon shrinkage (51).
Chronic Inflammatory Demyelinating Polyneuropathy
Several investigators have drawn attention to the association between chronic inflammatory demyelinating polyneuropathy (CIDP) and diabetes. The typical presentation of patients with superimposed CIDP includes symmetric weakness with demyelination and conduction block on electromyography and demyelination on nerve biopsy. The clinical progression is characteristically more rapid than that of diabetic polyneuropathy, weakness may be more prominent and there is often a satisfactory clinical response to immune modulation (51a,51b,51c,51d).
The differentiation from patients with diabetic polyneuropathy is not easily accomplished owing to several features in common. An elevated cerebrospinal fluid protein is present in both conditions, as are demyelinating changes on nerve conduction studies. The presence of conduction block on nerve conduction studies, however, is more suggestive of CIDP. The prevalence of conduction block appears similar in CIDP patients with and without diabetes mellitus (51b).
The characteristic nerve biopsy in both CIDP and diabetic polyneuropathy shows axonal and demyelinating changes (51a,51e). While a prominent inflammatory infiltrate on nerve biopsy may indicate CIDP, inflammation is only rarely seen in CIDP, and, furthermore, inflammation may also be present on
nerve biopsies of patients with a generalized diabetic peripheral neuropathy (51f,51g).
nerve biopsies of patients with a generalized diabetic peripheral neuropathy (51f,51g).
ASYMMETRIC NEUROPATHIES
Cranial Neuropathy
Cranial neuropathies also belong to the category of mononeuropathies. The majority of diabetic cranial neuropathies affect the third and sixth cranial nerves (52,53), whereas the fourth cranial nerve is rarely affected alone (52). Onset of diplopia is followed by complete ophthalmoplegia within several days. In cases of third-nerve involvement, there may be complete ptosis but the pupil is typically spared. Weakness involves all extraocular muscles except the lateral rectus and superior oblique muscles. The pain, which is characteristically in the frontal and periorbital region, accompanies ophthalmoplegia in about 50% of cases. Unlike painful ophthalmoplegia associated with temporal arteritis (54), eye muscle weakness occurs in a specific nerve distribution rather than from ischemic muscle involvement. The suggestion that pain may be due to involvement of the first and second divisions of the trigeminal nerve in the cavernous sinus is supported by the occasional presence of sensory impairment in the distribution of the trigeminal nerve (52). However, a more likely explanation is that pain originates from ischemia or pain-sensitive terminals in the sheath of the third nerve (55). Differentiation from a neoplastic or vascular lesion in the orbital fissure, cavernous sinus, infarction at the base of the brain, or focal midbrain infarction (56) should be made with brain imaging studies such as magnetic resonance imaging (MRI). Sparing of the pupil may be a consequence of the relatively intact peripherally located pupillomotor fibers supplied by cavernous sinus blood and spared by the centrally placed nerve lesion. However, compressive lesions of the third nerve within the cavernous sinus also may spare the pupil (57) and should be excluded by brain imaging studies. Recovery without residual weakness always occurs and is usually complete within 3 months, supporting the notion that focal demyelination without axonal destruction is the responsible lesion (58).
Convincing evidence that other cranial nerve palsies occur with increased frequency in diabetes is lacking. In one uncontrolled study, impaired olfaction was reported in 35 of 58 patients with diabetes who showed no evidence of abnormalities of the nasal mucosa (59).
Optic disc edema indistinguishable in appearance from papilledema with associated hemorrhages of the nerve fiber layer and cotton-wool spots has been described in juvenile-onset diabetes (60,61). This usually is associated with only mild impairment in visual acuity and a favorable prognosis. This condition is of obscure etiology but is believed to be due to vasculopathy of the most superficial capillary layer of the disc and adjacent retina (60,61). Anterior ischemic optic neuropathy may occur in diabetes but is more closely associated with hypertension. This is an ischemic infarction of the anterior optic nerve that produces acute edema of the optic disc, profound visual loss, and subsequent development of optic atrophy. Optic atrophy and nerve deafness are associated with diabetes in Wolfram syndrome.
Facial paralysis due to seventh nerve palsy may occur with increased frequency in patients with diabetes (62), and the prognosis for recovery may be worse than in patients without diabetes (63). In view of the high frequency of this neuropathy in the general population, its designation as a diabetic mono-neuropathy remains uncertain.
Proximal Motor Neuropathy
Diabetic amyotrophy was originally described by Bruns (64) in 1890 and again by Garland and Taverner (65) in 1953 as diabetic myelopathy. Because clinical and pathologic evidence for spinal cord involvement was not forthcoming, this syndrome was subsequently designated diabetic amyotrophy (66), a deliberately noncommittal term with regard to localization of the disease process. An array of terms have subsequently been used for this syndrome, including femoral neuropathy (67,68), asymmetric motor neuropathy (69), subacute proximal diabetic neuropathy (70,71), proximal mononeuropathy multiplex (72), diabetic poly radiculopathy (73), and diabetic lumbosacral radiculoplexus neuropathy (74). Asbury (75) has recommended that the term diabetic amyotrophy be dropped because of its ambiguity and that the term proximal motor neuropathy be used instead.
This neuropathy typically occurs with a peak incidence in the fifth or sixth decade in patients with type 2 diabetes. Many patients have mild or unrecognized diabetes at the time of diagnosis. In a recent series, diabetic amyotrophy was the presenting manifestation of diabetes in one third of the subjects (76). Some authors have emphasized an association with poor glycemic control (66,77,78).
The clinical picture is one of acute or subacute pain, weakness, and atrophy of the pelvic girdle and thigh musculature. The iliopsoas and quadriceps are usually involved, producing weakness of hip flexion and knee stabilization within several weeks of onset of pain. As a result, buckling of the knee and difficulty climbing stairs are typical symptoms. In some cases, coexistent weakness of the glutei, hamstrings, thigh adductors, and, less commonly, the peroneal and tibial muscles is present, indicative of the more widespread distribution of the disorder. Symptoms may have a monophasic or stepwise progression (77,79,80,81,82,83). Symptoms begin unilaterally but extend to the opposite extremity within weeks or months (74). Most patients have weight loss, and some appear cachectic. The extent of the weight loss highlights the systemic nature of the disorder. The weight loss may be compounded by anorexia caused by reactive depression or the use of narcotic analgesics.
Despite its designation as a motor neuropathy, subtle sensory symptoms and signs are commonly present in the form of paresthesias and sensory disturbance in the anterior thigh and anteromedial aspects of the lower leg typically in the anterior femoral cutaneous and saphenous nerve distribution. The knee jerk is nearly always reduced or absent on the affected side, whereas ankle jerks may be preserved unless compromised by a coexistent distal polyneuropathy.
Deep, aching pain is prominent and is localized to the hip, buttock, and anterior thigh. Pain is unrelieved by rest, is typically worse at night than during the day, and is not increased with straight leg raising or other mechanical maneuvers. The process is typically unilateral in onset, but subsequent involvement of the opposite leg often occurs within 3 to 4 months.
Despite early reports to the contrary (66), signs of myelopathy are absent and plantar responses are usually flexor. Pain, sensory abnormalities, and weakness in thoracic root distribution occasionally occur concomitantly (25), but isolated shoulder-girdle involvement is distinctly uncommon (73) and, when present, usually occurs in patients with marked leg weakness (70,78,79).
Differentiation from compressive lumbar nerve-root disease and neoplastic infiltration of lumbosacral plexus may be difficult, and laminectomies and laparotomies have occasionally been carried out in such patients in search of a structural cause. As originally pointed out by Root and Rogers (84), and more recently discussed by Hirsh (85), the absence of mechanical signs and symptoms, lack of back pain, prominent nocturnal pain with failure to respond to bed rest, and muscular atrophy and weakness involving more than one lumbar root usually distinguishes proximal motor neuropathy from nerve-root compression.
The prognosis is usually good, with most patients showing resolution of pain followed later by gradual return of strength over a period of 6 to 18 months (73,77,78). Patients with unilateral and relatively focal pain and weakness seem to improve more rapidly and completely than patients with more widespread involvement. Because of the severe pain and disability associated with this syndrome, the ability to reassure affected patients of a favorable prognosis provides them great psychological relief.
There has been considerable debate concerning the etiology and proper classification of proximal motor neuropathy (75). Subramony and Wilbourn (86) have emphasized the heterogenicity of the syndrome, in that some patients with proximal motor neuropathy have clinical and electromyographic evidence of distal polyneuropathy whereas others appear to have a more localized process. The finding of slow nerve-conduction velocities in femoral and distal nerves (81,86,87,88,89) and of features of demyelination in nerve biopsy specimens in these patients indicates that “diabetic amyotrophy” is a form of diabetic neuropathy with a predilection for proximal nerves rather than a primary disorder of anterior horn cells of muscle. On the basis of extensive clinical electrophysiologic experiences, Bastron and Thomas (73) at the Mayo Clinic concluded that the disorder is a polyradiculopathy. Electromyography of patients with diabetic amyotrophy characteristically displays abundant fibrillations in the affected limb muscles and the paraspinal muscles. Nerve-conduction studies are unable to differentiate patients with diabetic amyotrophy from those with a generalized polyneuropathy.
Recent studies have emphasized the likelihood that this disorder has a vascular basis (90,91). A vascular etiology was first proposed for the more acute case of diabetic amyotrophy by Raff and Asbury (72,75), who documented occlusion of intrafascicular artery of the obturator nerve and numerous small-vessel infarcts in the lumbosacral plexus and proximal nerve trunks of the patient who exhibited the rapid appearance of painful proximal asymmetric leg weakness.
The possibility that this disorder has an inflammatory etiology has led to the use of immune-modulating therapies. Intravenous immunoglobulins, plasmapheresis, and corticosteroids have all been used in open-label, uncontrolled studies (71,90,92). While preliminary results suggest some clinical benefit, the need for blinded, placebo-controlled trials is highlighted by the patient of Said et al. (91), who had a spontaneous remission shortly after biopsy and prior to the initiation of corticosteroid therapy (92a).
Thoracic Radiculopathy
This entity, also known as thoracoabdominal neuropathy, did not gain attention in the English-language literature until the late 1970s (23,24). Similar to painful proximal motor neuropathies of the legs, this disorder usually occurs in middle-aged patients and often in those who have relatively mild diabetes. In many cases, patients with this syndrome have had previous or concomitant painful lumbar root syndromes in the lower extremities.
Onset of pain is usually acute, and the pain may be located in the back, chest, or abdomen. The character of the pain resembles that of herpes zoster and is usually deep and aching with some elements of superficial sharp or burning pain. Changes in pain with alterations of position or physical activity are variable. Paresthesia and cutaneous hypersensitivity are usually present but may be mild or absent, sometimes resulting in failure to recognize the neuropathic basis for pain. The pain is usually unilateral but is sometimes bilateral, may be distributed over more than one dermatomal segment, and often does not have a classic girdling radicular distribution. There may be an accompanying area of sensory loss or dysesthesia in the distribution of one or more adjacent intercostal nerves, the dorsal or ventral rami, or their branches (93). Impairment in light touch and hypersensitivity to pin stimulation, however, are often absent. In severe cases, weakness and laxity of segmental para spinal and abdominal muscles are present and abdominal hernia may even occur (94,95). Electromyography of paraspinal, intercostal, and abdominal muscles is diagnostically helpful and usually shows changes of acute denervation (24,25,96,97). As with proximal lower-extremity motor neuropathy, weight loss may be prominent, and because of the frequent absence of definite neuropathic symptoms and signs, exhaustive, unfruitful searches for an intrathoracic or intraabdominal neoplasm often are undertaken. The finding of electromyographic abnormalities usually leads to the correct diagnosis. Cases in which the distribution of symptoms and signs conforms to a single thoracic root should be evaluated with x-ray and MRI studies of the thoracic spine to exclude a compressive radiculopathy. The prognosis is usually better for the lower extremity radiculopathies, with a gradual recovery within a matter of months to a year (23).
Similar to other diabetic mononeuropathies and radiculopathies, the etiology of thoracic radiculopathy is obscure, although the acute onset and spontaneous recovery suggest a focal ischemic process. The observation that thoracic radiculopathy, proximal asymmetric motor neuropathy, and cranial mononeuropathy occur among middle-aged patients with type 2 diabetes, often appear in the same patient, improve spontaneously, and have a tendency to recur suggests a common physiologic mechanism. Although no pathologic studies of patients with thoracic radiculopathy have been published, postmortem studies of patients with diabetic polyneuropathy do show axonal and demyelinative lesions of nerve roots (81,98). Skin biopsies of patients with thoracic radiculopathy have shown a marked reduction in dermal and epidermal nerve fibers in the affected dermatome (98a).
Limb Mononeuropathy
Mononeuropathy is particularly common in persons with diabetes and may occur on the basis of focal ischemia, entrapment, compression, or trauma to superficially placed nerves (99). Any of the major peripheral nerves may be affected. Symptoms may present suddenly or gradually. When several nerves are involved simultaneously, the disorder is referred to as mononeuropathy multiplex. Many patients with diabetic polyneuropathy have electrophysiologic or clinical evidence of superimposed focal mononeuropathy at various common sites of entrapment or nerve injury, such as the median nerve at the wrist, ulnar nerve at the elbow, peroneal nerve at the fibular head, radial nerve above the elbow, and lateral cutaneous nerve of the thigh (99). This may be because nerves affected by segmental demyelination are known to be particularly sensitive to the effects of compression and anoxia. Differential diagnosis of mononeuropathy or mononeuropathy multiplex include vasculitis, paraproteinemic neuropathy, amyloidosis, acromegaly, hypothyroidism, sarcoidosis, Lyme disease, and bleeding into peripheral nerves caused by coagulation defects.
Carpal tunnel syndrome caused by median-nerve entrapment in the wrist is particularly common among persons with diabetes. A recent study report neurophysiologic evidence consistent with a carpal tunnel syndrome in 23% of patients with mild diabetic neuropathy. The carpal tunnel syndrome usually produces symptoms and signs similar to those in persons without diabetes. Occasionally, however, distal median-nerve mononeuropathy may occur in the absence of the usual pain and sensory symptoms of carpal tunnel syndrome. Although
entrapment is still possible in such cases, coexistent distal ulnar neuropathy and bilateral involvement may suggest distal polyneuropathy rather than nerve entrapment (100). Nerve-conduction studies showing prolonged distal latencies in multiple nerves rather than limited to the median nerve will serve to distinguish distal polyneuropathy from entrapment.
entrapment is still possible in such cases, coexistent distal ulnar neuropathy and bilateral involvement may suggest distal polyneuropathy rather than nerve entrapment (100). Nerve-conduction studies showing prolonged distal latencies in multiple nerves rather than limited to the median nerve will serve to distinguish distal polyneuropathy from entrapment.
Peroneal mononeuropathy typically produces sudden painless foot drop and, in addition to vascular factors, may be due to trauma because of the superficial location of the nerve at the fibular head. Ulnar mononeuropathy is probably also related to the vulnerable position of the nerve at the elbow. In this case, symptoms usually appear insidiously and may be due to chronic trauma rather than to acute injury or entrapment. Phrenic neuropathy, resulting in diaphragmatic paralysis, may occur rarely in patients with diabetes (101).
PATHOLOGY OF PERIPHERAL NEUROPATHY
Pathogenesis of Symmetric Neuropathies
The pathophysiologic basis of diabetic distal polyneuropathy remains uncertain. The two major prevailing theories relate the metabolic effects of chronic hyperglycemia and the effects of ischemia on peripheral nerves to the pathogenesis of this disorder (102,103). Alterations in neurotrophic factors and immunologic mechanisms also may play a pathogenetic role. It is likely that multiple interacting factors play a role in the pathogenesis of this disorder.
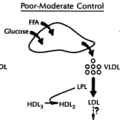
METABOLIC
The metabolic hypothesis proposes that hyperglycemia produces several metabolic derangements, including increased tissue levels of sorbitol and fructose (104,105), decreased concentrations of nerve myo-inositol and taurine (106), decreased Na+/K+ adenosine triphosphatase (ATPase) activity (104,105), nonenzymatic glycosylation of proteins, altered fatty acid metabolism, and abnormalities of axonal flow. Some or all of these factors may be responsible for functional and structural changes in nerve fibers.
Polyol Pathway Abnormalities
The polyol pathway may play a role in several of these metabolic changes. The hyperglycemic milieu results in activation of the polyol pathway and, in a reaction catalyzed by the enzymes aldose reductase and sorbitol dehydrogenase, leads to the conversion of glucose to the polyol sugars sorbitol and fructose. The accumulation of sorbitol results in reduced intracellular levels of myo-inositol and taurine, which in turn reduce Na+/K+ ATPase and contribute to the structural and functional changes (104).
Decreased levels of intracellular myo-inositol lead to reduced phosphoinositide synthesis and decreased production of diacylglycerol. This in turn impairs protein kinase C activation and may lead to decreased Na+/K+ ATPase activity. Impaired Na+/K+ ATPase activity results in abnormal decreased nodal Na+membrane potentials, increased intraaxonal Na+, and possible nodal swelling and other structural change. Activation of the polyol pathway also may promote oxidative stress by depleting NADPH, a cofactor for both aldose reductase and glutathione reductase, which leads to a decrease in reduced glutathione and increase in oxidized glutathione (104).
Endoneurial concentrations of sorbitol and fructose are increased in the alloxan and streptozotocin model of diabetes. Aldose reductase inhibition reduces endoneurial sorbitol and restores Na+/K+ ATPase activity and myo-inositol and taurine levels in somatic and autonomic nerves (106,107). Treatment with aldose reductase inhibitors also leads to improved nerve-conduction velocities in these diabetic rat models.
Myo-Inositol
myo-inositol and inositol levels are reduced within the peripheral nerve in the streptozotocin model of diabetes. Dietary supplementation with myo-inositol reverses the slowing of nerve-conduction velocity and reduction in intracellular Na+/K+ ATPase that occurs in this experimental model of diabetic peripheral neuropathy (104,110). This, however, has not been replicated in human diabetic peripheral neuropathy. As noted above, a reduction in endoneurial myo-inositol is not apparent in human diabetic nerves (108,109,111).
Taurine
Osmoregulation, in order to maintain the intracellular milieu, may also result in endoneurial metabolic changes in diabetic neuropathy. The increase in intracellular osmolality due to shunting of glucose into the polyol pathway and the consequent accumulation of sorbitol may lead to compensatory depletion of the endoneurial osmolytes taurine and myo-inositol to maintain osmotic balance (106).
Abnormal Lipid Metabolism
Diabetes also results in alterations in the metabolism of essential fatty acids and prostaglandin. Hyperglycemia leads to inhibition of δ-6-desaturase, the enzyme that converts dietary linoleic acid to γ-linolenic acid. γ-Linolenic acid is a precursor of arachidonic acid that provides the substrate for several vasoactive prostanoids, including prostacyclin. In addition, γ-linolenic acid metabolites play a role in the nerve membrane structure, nerve blood flow, and nerve conduction (112).
Oxidative Stress
Oxidative stress also is implicated in the etiology of diabetic neuropathy. There is evidence that activity of oxygen-free radicals is enhanced in diabetes. Indices of increased oxidative stress such as malondialdehyde, conjugated dienes, and lipid hydroperoxides are increased in experimental diabetic neuropathy.
Furthermore, diabetes compromises antioxidant defense mechanisms. There are documented reductions in scavengers of oxygen free radicals, such as reduced glutathione, superoxide dismutase, catalase, ascorbic acid, and α-tocopherol (116).
Antioxidant therapy with a number of agents, including probuchol (117), vitamin E (117,118), glutathione (119), carvedilol (120), butylated hydroxytoluene (121), transitional metal chelating agents (122), and α-lipoic acid (123), have improved measures of nerve function in experimental diabetic peripheral neuropathy.
Advanced Glycosylation End Products
The reducing sugars glucose, fructose, and galactose react with the free amino groups of proteins to form early reversible Schiff bases and Amadori products. These in turn undergo a chemical rearrangement to form advanced glycosylation end products. In the setting of prolonged hyperglycemia, nonenzymatic glycosylation of proteins occurs, which results in structural changes to the components of the extracellular matrix (124,125).
These structural changes may lead to functional neural and vascular abnormalities. Advanced glycosylated end products also may quench nitric oxide, thereby attenuating endothelium-mediated vasodilatation (126). Aminoguanidine may inhibit the formation of advanced glycosylated end products and improve nerve and vascular function (124,125,126,127,128). There have been no reports of human trials with this agent.
These structural changes may lead to functional neural and vascular abnormalities. Advanced glycosylated end products also may quench nitric oxide, thereby attenuating endothelium-mediated vasodilatation (126). Aminoguanidine may inhibit the formation of advanced glycosylated end products and improve nerve and vascular function (124,125,126,127,128). There have been no reports of human trials with this agent.
Protein Kinase C Activation
Hyperglycemia leads to increased synthesis of diacylglycerol, which leads to activation of protein kinase C. Protein kinase C may also be activated by oxidative stress and advanced glycosylated end products. Protein kinase C activation causes increased vascular permeability, impaired nitric oxide synthesis, and changes in blood flow (129).
There is some evidence that impaired protein kinase C activity may contribute to reduced Na+/K+ ATPase activity. Recently data have emerged suggesting that there is increased protein kinase C activity in the retina, kidney, and the vasculature of nerve tissue.
Protein kinase C elevations compromise nerve regeneration in experimental models of diabetic peripheral neuropathy (130,131). In experimental models of diabetes, treatment with nonspecific (132) and β-specific protein kinase C inhibitors normalized the observed neurophysiologic abnormalities (132a).
Poly (ADP-Ribose) Polymerase
There is increasing evidence that poly (ADP-ribose) polymerase (PARP) plays a critical role in mediating several pathways of hyperglycemia-induced damage (activation of PKC isoforms, hexosamine pathway flux, and AGE formation). This most likely occurs by inhibiting GAPDH activity. DNA strand breaks due to oxidative stress are a major cause of PARP activation (132b,132c). In streptozotocin-induced diabetic rats, the PARP inhibitors, 3-aminobenzamide and 1,5-isoquinolinediol, reversed deficits in nerve blood flow and conduction (132c).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree