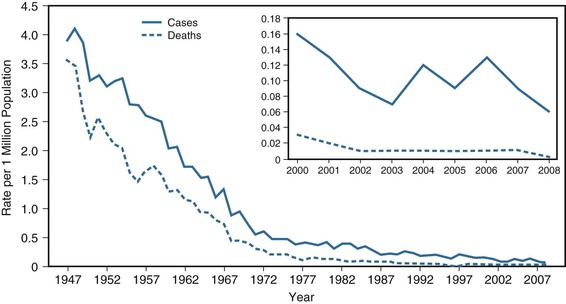
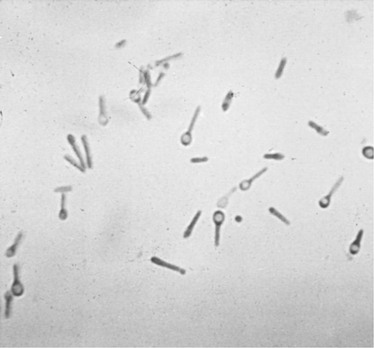
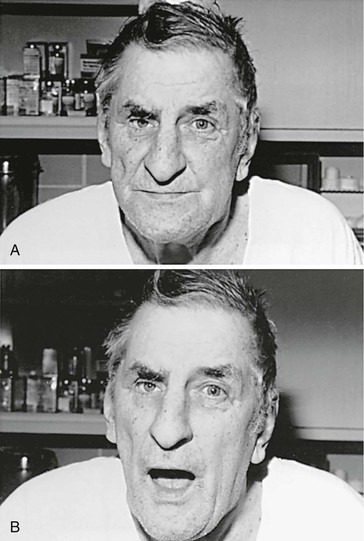
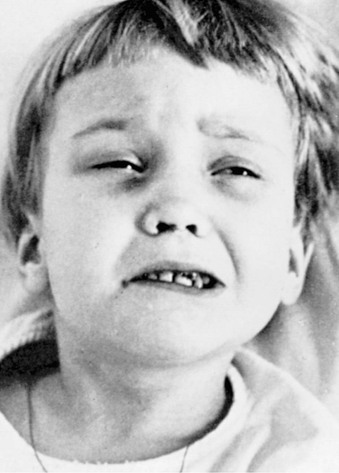
Aimee Hodowanec, Thomas P. Bleck Tetanus was well known to the ancients; descriptions by Egyptian and Greek physicians survive to the present. They recognized the frequent relationship between injuries and the subsequent development of fatal spasms. Gowers provided the quintessential description of tetanus in 1888: Tetanus is a disease of the nervous system characterized by persistent tonic spasm, with violent brief exacerbations. The spasm almost always commences in the muscles of the neck and jaw, causing closure of the jaws (trismus, lockjaw), and involves the muscles of the trunk more than those of the limbs. It is always acute in onset, and a very large proportion of those affected die.1 Nicolaier2 isolated a strychnine-like toxin from anaerobic soil bacteria in 1884. Six years later, Behring and Kitasato3 described active immunization with tetanus toxoid. This latter discovery should have reduced tetanus to a historical curiosity, but we still fail to fulfill this promise. Between 2001 and 2008 the Centers for Disease Control and Prevention (CDC) received reports of 233 tetanus cases, with an overall annual incidence of 0.10 cases per 1 million persons and an incidence of 0.23 cases per 1 million persons 65 years or older.4 Data through 2008 are summarized in Figure 246-1. Globally, 14,132 cases of tetanus were reported in 2011.5 U.S. and global statistics likely represent underreporting. Most reported cases are in patients older than 60 years,6 indicating that waning immunity is an important risk factor.7 This may be a particularly serious problem in older women.8,9 Changes in patterns of immigration may increase the number of unimmunized or inadequately immunized patients presenting for care in developed countries.10 Injection drug abuse places patients at risk for tetanus,11 as do other potentially unsterile practices that allow inoculation of spores.12 Acute injuries account for about 70% of U.S. cases, evenly divided between punctures and lacerations.13 Other identifiable conditions are noted in 23%, leaving about 7% of cases without an apparent source. Other studies cite rates of cryptogenic tetanus as high as 23%. Outbreaks of tetanus are common after natural disasters in developing countries, when people are likely to suffer from open wounds, fractures, and crush injuries.14 In developing countries, mortality rates due to tetanus are as high as 28 per 100,000. Until recently, primary tetanus immunization programs in these countries were ineffective. As a result, 800,000 to 1 million annual deaths were attributed to tetanus during the 1980s.15 Two thirds of cases worldwide occurred in sub-Saharan Africa, where more than 40% of tetanus is a result of neonatal infection15,16; nearly one third of these infants were born to mothers of a previously afflicted child, highlighting a failure to immunize.17 In 1989, a worldwide commitment to the elimination of neonatal tetanus by the World Health Assembly18,19 resulted in a decline of more than 50% in the next 10 years.20 A resurgent effort in 1999, the Maternal and Neonatal Tetanus Elimination Program,21 met with additional success. In 2010, the World Health Organization (WHO) estimated that there were 58,000 neonatal deaths due to tetanus, representing a 93% reduction in neonatal tetanus deaths compared with the 1980s.22 The Global Immunization Vision and Strategy, launched by the WHO and the United Nations Children’s Fund in 2005, continues to target tetanus as a preventable cause of neonatal death by promoting routine tetanus toxoid administration in hard-to-reach, previously underserved areas.23 As of 2011, it was estimated that globally, 83% of infants had received at least three doses of the diphtheria-tetanus-pertussis vaccine.24 Clostridium tetani is an obligately anaerobic bacillus that is gram positive in fresh cultures but may have variable staining in older cultures or tissue samples.25 The complete genome of the organism has been sequenced, and its products were recently compared with other clostridia.26 During growth, the bacilli possess abundant flagella and are sluggishly motile. Two toxins, tetanospasmin (commonly called tetanus toxin) and tetanolysin, are produced during this phase. Tetanospasmin is encoded on a plasmid that is present in all toxigenic strains.27 Tetanolysin is of uncertain importance in the pathogenesis of tetanus. Mature organisms lose their flagella, develop a terminal spore, and begin to resemble a squash racquet (Fig. 246-2).28 The spores are extremely stable in the environment, retaining the ability to germinate and cause disease indefinitely. They withstand exposure to ethanol, phenol, or formalin but can be rendered noninfectious by iodine, glutaraldehyde, hydrogen peroxide, or autoclaving at 121° C and 103 kPa (15 psi) for 15 minutes. Growth in culture is optimal at 37° C under strictly anaerobic conditions, but culture results are of no diagnostic value. Antibiotic sensitivity is discussed later. The clostridial toxins that produce both tetanus and botulism are similar in structure and function despite the almost diametrically opposed clinical manifestations of the diseases. These toxins are zinc-dependent matrix metalloproteinases, a category encompassing a diverse group of enzymes ranging from normal human cellular constituents necessary for cellular remodeling,29 through determinants of neoplastic cell function,30 to exotoxins of other microorganisms such as Bacteroides fragilis.31 Tetanospasmin is synthesized as a single 151-kDa chain that is cleaved extracellularly by a bacterial protease into a 100-kDa heavy chain and a 50-kDa light chain (fragment A), which remain connected by a disulfide bridge.32 The heavy chain can be further divided into fragments B and C by pepsin. The heavy chain appears to mediate binding to cell surface receptors and transport proteins, whereas the light chain produces the presynaptic inhibition of transmitter release that produces clinical tetanus. The nature of the receptor to which tetanospasmin binds, previously thought to be a ganglioside, remains debated.33 The toxin enters the nervous system primarily through the presynaptic terminals of lower motor neurons, where it can produce local failure of neuromuscular transmission. It then exploits the retrograde axonal transport system and is carried to the cell bodies of these neurons in the brainstem and spinal cord, where it expresses its major pathogenic action.34 Once the toxin enters the central nervous system, it diffuses to the terminals of inhibitory cells, including both local glycinergic interneurons and descending γ-aminobutyric acid-ergic (GABAergic) neurons from the brainstem. The toxin degrades synaptobrevin, a protein required for docking of neurotransmitter vesicles with their release site on the presynaptic membrane.35 By preventing transmitter release from these cells, tetanospasmin leaves the motor neurons without inhibition. This produces muscular rigidity by raising the resting firing rate of motor neurons and also generates spasms by failing to limit reflex responses to afferent stimuli. Excitatory transmitter release in the spinal cord can also be impaired, but the toxin appears to have greater affinity for the inhibitory systems. The autonomic nervous system is affected as well; this is predominantly manifested as a hypersympathetic state induced by failure to inhibit adrenal release of catecholamines. Toxin binding appears to be an irreversible event. At the neuromuscular junction, initial recovery from botulism depends on sprouting a new axon terminal; this is probably the case at other affected synapses as well. Later, the new synapses are removed when the original ones reestablish their connections.36 Tetanus is classically divided into four clinical types: generalized, localized, cephalic, and neonatal. These are valuable diagnostic and prognostic distinctions but reflect host factors and the site of inoculation rather than differences in toxin action. Terms describing the initial stages of tetanus include the incubation period (time from inoculation to the first symptom) and the period of onset (time from the first symptom to the first generalized spasm). The shorter these periods, the worse the prognosis.37 Various rating scales are available.38 Certain portals of entry (e.g., compound fractures) are associated with poorer prognoses. Tetanus may be particularly severe in narcotics addicts, for unknown reasons.39 Generalized tetanus is the most commonly recognized form and often begins with risus sardonicus (increased tone in the orbicularis oris) and trismus (“lockjaw”; masseter rigidity) (Fig. 246-3). Abdominal rigidity may also be present. The generalized spasm resembles decorticate posturing and consists of opisthotonic posturing with flexion of the arms and extension of the legs (Fig. 246-4). The patient does not lose consciousness and experiences severe pain during each spasm. The spasms are often triggered by sensory stimuli. During the spasm, the upper airway can be obstructed, or the diaphragm may participate in the general muscular contraction. Either of these compromises respiration, and even the first such spasm may be fatal. In the modern era of intensive care, however, the respiratory problems are easily managed, and autonomic dysfunction, usually occurring after several days of symptoms, has emerged as the leading cause of death.40 The illness can progress for about 2 weeks, reflecting the time required to complete the transport of toxin, which is already intra-axonal when antitoxin treatment is given. The severity of illness may be decreased by partial immunity.41 Recovery takes an additional month and is complete unless complications supervene. Lower motor neuron dysfunction may not be apparent until spasms remit, and recovery from this deficit in neuromuscular transmission may take additional weeks.42 Recurrent tetanus may occur if the patient does not receive active immunization because the amount of toxin produced is inadequate to induce immunity.43 Localized tetanus involves rigidity of the muscles associated with the site of spore inoculation. This may be mild and persistent and often resolves spontaneously. Lower motor neuron dysfunction (weakness and diminished muscle tone) is often present in the most involved muscle. This chronic form of the disease probably reflects partial immunity to tetanospasmin.44 Localized tetanus is more commonly a prodrome of generalized tetanus, however, which occurs when enough toxin gains access to the central nervous system. Cephalic tetanus is a special form of localized disease affecting the cranial nerve musculature, almost always after an apparent head wound (Fig. 246-5). Although earlier reports linked cephalic tetanus to a poor prognosis, more recent studies have revealed many milder cases. A lower motor neuron lesion, frequently producing facial nerve weakness, is often apparent.45 Extraocular muscle involvement is occasionally noted. Neonatal tetanus (Fig. 246-6) follows infection of the umbilical stump, most commonly caused by a failure of aseptic technique if mothers are inadequately immunized.46 Cultural practices may contribute.47 The condition usually presents with generalized weakness and failure to nurse; rigidity and spasms occur later. The mortality rate exceeds 90%, and developmental delays are common among survivors.48 Poor prognostic factors include age younger than 10 days, symptoms for fewer than 5 days before presentation to hospital, and presence of risus sardonicus or fever.49 Apnea is the leading cause of death among neonatal tetanus patients in the first week of life, and sepsis in the second week.50 Bacterial infection of the umbilical stump leads to sepsis in almost half of infants with neonatal tetanus, which contributes to the substantial mortality despite treatment.51
Tetanus (Clostridium tetani)
History
Epidemiology
Characteristics of Clostridium Tetani
Pathogenesis
Clinical Manifestations

Tetanus (Clostridium tetani)
246