SMA, superior mesenteric artery; SMV, superior mesenteric vein; PV, portal vein; SMV–PV, superior mesenteric–portal vein confluence
PANCREATICODUODENECTOMY
Pancreaticoduodenectomy involves resection of the pancreatic head, duodenum, gallbladder, and bile duct with or without removal of the gastric antrum. Our recommended technique includes a brief staging laparoscopy to exclude liver and peritoneal metastases followed by a midline upper abdominal incision.
The surgical resection is divided into the following steps:
1.Isolation of the infrapancreatic SMV and separation of the colon and its mesentery from the duodenum and pancreatic head: The lesser sac is entered by mobilizing the greater omentum up off of the transverse colon. The loose attachments of the posterior gastric wall to the anterior surface of the pancreas are divided. The hepatic flexure of the colon is freed from its retroperitoneal attachments, exposing the pancreatic head and duodenum. The visceral peritoneum along the inferior border of the pancreas is incised starting from the left of the middle colic vessels toward the patient’s right and inferiorly to expose the junction of the middle colic vein and SMV. The retroperitoneal attachments of the small bowel and right colon mesentery are taken down to a much greater extent in patients with uncinate tumors extending into the small bowel mesentery. When necessary, the small bowel mesentery can be mobilized by incising the visceral peritoneum all the way up to the ligament of Treitz (Cattell-Braasch maneuver).
2.The Kocher maneuver is begun at the third part of the duodenum by identifying the inferior vena cava. All tissue medial to the right gonadal vein and anterior to the inferior vena cava is elevated along with the pancreatic head and duodenum. This dissection is continued to the left lateral edge of the aorta, with exposure of the anterior surface of the left renal vein. A complete Kocher maneuver is necessary for the subsequent dissection of the pancreatic head from the SMA (step 6). Particularly important is the division of the leaf of peritoneum that extends from the retroperitoneum to the root of mesentery; incision of this portion of peritoneum is perhaps the most important part of the Kocher maneuver.
3.The portal dissection is commenced by exposing the CHA proximal and distal to the right gastric artery and the gastroduodenal artery (GDA). Both the right gastric and the GDA are then ligated and divided. Division of the GDA allows mobilization of the hepatic (common-proper) artery off the underlying PV. Cholecystectomy is then performed, and the common hepatic duct is transected at or above its junction with the cystic duct. Following transection of the bile duct, bile cultures are sent and indwelling endobiliary stents are removed. A bulldog clamp is placed on the transected hepatic duct to prevent bile from soiling the right upper quadrant until biliary reconstruction is completed. Note, the PV should always be exposed and the location of the right hepatic artery noted prior to dividing the common hepatic duct.
The PV should be identified but not extensively mobilized until step 6, at which time the stomach and pancreas have been divided. Care must be taken to avoid injury to the superior pancreaticoduodenal vein draining the pancreatic head at the superolateral aspect of the PV, or significant bleeding may occur when one does not yet have adequate exposure and vascular control.
4.The terminal branches of the left gastric artery are ligated and divided along the lesser curvature of the stomach prior to gastric transection. The stomach is then transected with a linear gastrointestinal (GIA) stapler at the level of the third or fourth transverse vein on the lesser curvature and at the confluence of the gastroepiploic veins on the greater curvature to complete a standard antrectomy (Fig. 7.1). The omentum is then divided at the level of the greater curvature transection. In the pylorus-preserving variant, the duodenum is divided just distal to the pylorus.
5.The loose attachments of the ligament of Treitz are taken down with care to avoid injury to the inferior mesenteric vein (IMV) situated immediately to the patient’s left running caudal to cranial. The jejunum is then transected with a linear GIA stapler approximately 8 to 10 cm distal to the ligament of Treitz and its mesentery sequentially ligated and divided with an energy device such as the LigaSure. This dissection is continued proximally to involve the fourth and third portions of the duodenum. The duodenal mesentery is divided to approximately the level of the aorta, allowing the devascularized segment of duodenum and jejunum to be reflected beneath the mesenteric vessels into the right upper quadrant.
6.This step is oncologically the most important and difficult part of the operation. Traction sutures are placed on the superior and inferior borders of the pancreas, and the pancreas is then transected with electrocautery at the level of the PV. There is usually a small artery that runs along the inferior border of the pancreas that is secured with the traction sutures. If there is evidence of tumor adherence to the PV or SMV, the pancreas is divided more upstream (to the tail) in the preparation for segmental venous resection. The specimen is separated from the SMV by ligation and division of the small venous tributaries to the uncinate process and pancreatic head (Fig. 7.2). Complete removal of the uncinate process from the SMV is required for full mobilization of the SMV–PV confluence and subsequent identification of the SMA. Failure to fully mobilize the SMV–PV confluence risks injury to the SMA and may result in a positive SMA margin. In addition, without complete mobilization of the SMV, it is difficult to expose the SMA. The inferior pancreaticoduodenal arteries (IPDAs) arising from the SMA must be identified and directly ligated. Mass ligation of the IPDAs with mesenteric soft tissue is a common cause of postoperative hemorrhage as the vessels may retract with the usual changes in blood pressure after extubation.
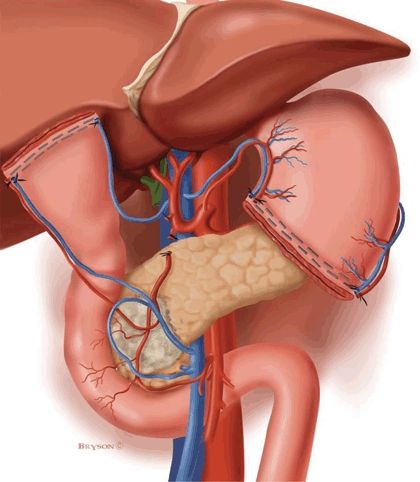
FIGURE 7.1 Illustration demonstrating completion of step 3 and step 4. The porta hepatis has been dissected, with ligation of the gastroduodenal and right gastric arteries. The gallbladder has been removed and the common hepatic duct transected (step 3). The antrum of the stomach has been divided at the level of the third or fourth transverse vein on the lesser curvature (step 4).
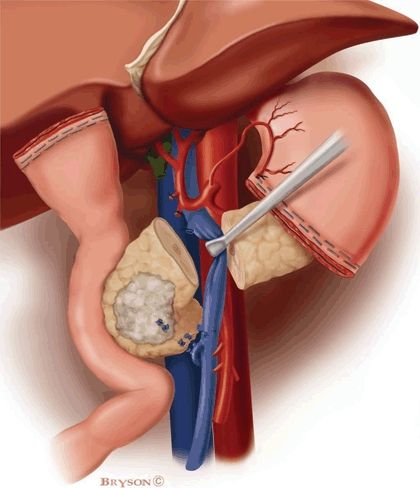
FIGURE 7.2 Illustration of step 6. The pancreatic head and uncinate process are being separated from the SMV–PV confluence. The pancreas has already been transected at the level of the PV. Small venous tributaries from the PV and SMV are ligated and divided including delicate branches from the uncinate to the first jejunal branch of the SMV.
Proper mobilization of the SMV involves identification of its first jejunal branch. This branch originates from the right posterolateral aspect of the SMV (at the level of the uncinate process), travels posterior to the SMA, and enters the medial (proximal) aspect of the jejunal mesentery. The jejunal branch may course anterior to the SMA in up to 20% of cases, a situation that makes this dissection somewhat simpler. If tumor involvement of the SMV (at the level of the jejunal branch) prevents dissection of the uncinate process from the SMV, the jejunal branch should be divided proximal to the site of tumor encasement and again at its junction with the main trunk of the SMV. Once the uncinate is separated from the distal SMV, medial retraction of the SMV–PV confluence allows exposure of the SMA. The specimen is then separated from the right lateral wall of the SMA, which is dissected to its origin at the aorta; the plane of dissection should be directly on the adventitia of this vessel (Fig. 7.3).
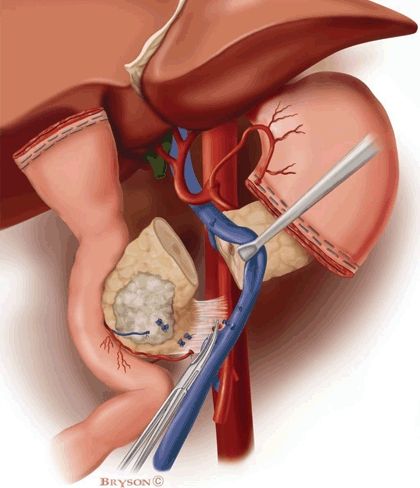
FIGURE 7.3 Illustration demonstrating sharp dissection of the SMA margin, the most critical component of step 6. Medial retraction of the SMV–PV confluence facilitates dissection of the soft tissues adjacent to the lateral wall of the proximal SMA. The IPDA (or arteries) is identified at its origin from the SMA, ligated, and divided.
The pancreatic and common hepatic duct transection margins are submitted for frozen-section evaluation. Positive resection margins demonstrating invasive carcinoma on the biliary or pancreatic duct mandate further resection until clear margins are achieved. Specimens should be oriented for the pathologist. The SMA margin must be identified and inked for the pathologist, as it cannot be accurately assessed in a retrospective fashion.
Pancreatic, Biliary, and Gastrointestinal Reconstruction
Reconstruction after pancreaticoduodenectomy begins with the pancreatic anastomosis.
1.The pancreatic remnant is mobilized from the retroperitoneum and distal splenic vein for a distance of 2 to 2.5 cm to allow accurate suture placement for the pancreaticojejunal anastomosis. The transected jejunum is brought retrocolic through a generous incision in the transverse mesocolon to the left (rather than the right) of the middle colic vessels. This minimizes tension on the anastomosis and provides a more direct route for the small bowel mesentery to approximate the pancreatic remnant than is afforded using a right-sided mesenteric window. A two-layer, end-to-side, duct-to-mucosa pancreaticojejunostomy is performed. Occasionally, we use a one-layer anastomosis if the pancreas is small, is firm, and contains a dilated duct. Additionally, a small silastic stent may be used if the pancreatic duct is small. If the duct is too small to allow passage of the stent, an invaginating technique dunking the pancreatic remnant into the jejunal limb may rarely be required. The anastomosis between the pancreatic duct and the small bowel mucosa is completed with 5-0 monofilament absorbable sutures. Each stitch incorporates a generous bite of the pancreatic duct and a full-thickness bite of the jejunum. The posterior knots are tied on the inside and the lateral and anterior knots on the outside. When a stent is used, this is placed into the pancreatic duct and small bowel for a distance of approximately 2 to 3 cm prior to tying the anterior sutures.
2.A single-layer biliary anastomosis is performed using interrupted 4-0 or 5-0 absorbable monofilament sutures at a distance from the pancreaticojejunal anastomosis chosen to eliminate any tension. An interrupted technique is utilized to avoid purse stringing of the anastomosis. A stent is rarely ever used, even when the bile duct is of normal caliber.
3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree