FIGURE 5.1 CT scan demonstrating a macrocystic serous cystic neoplasm (SCN) within the body of the pancreas.

FIGURE 5.2 Arterial-phase CT scan demonstrating the characteristic exophytic appearance of a pancreatic lymphoepithelial cyst.
Premalignant and Malignant
The clinical importance of identification of premalignant/malignant pancreatic cysts cannot be overstated. Their identification represents an opportunity to intervene prior to the development of invasive pancreatic malignancy. That said, the majority of premalignant pancreatic cysts will not transform into pancreatic cancer in a given patient’s lifetime, so surveillance is often recommended. Pancreatic cysts in the premalignant/malignant category include mucinous cysts (MCN and IPMN), cystic neuroendocrine tumors, and solid pseudopapillary neoplasm (SPN).
Mucinous cystic neoplasms (MCNs) occur primarily in female patients in the fifth to sixth decade of life. These are mucin-filled lesions without any connection to the pancreatic ductal system. They are unifocal and macrocytic with histology demonstrating ovarian-type stroma. They may demonstrate calcifications. When MCN transform, they become mucinous cystadenocarcinoma, which may represent up to 10% to 20% of MCN. Early in their course, mucinous cystadenocarcinoma may represent a more indolent form of cancer when compared to pancreatic adenocarcinoma. These lesions may stain positive for human chronic gonadotropic or estrogen receptors. Intraductal papillary mucinous neoplasm (IPMN) represents a spectrum of lesions with several common features including pancreatic ductal connection, mucin-producing epithelium, and papillary histology (Fig. 5.3). These cystic lesions may be unifocal, multifocal, or multicentric and occur most commonly in older patients (sixth to seventh decade). Anatomically, IPMN may involve the main or branch pancreatic ducts or both. Invasive IPMN is the malignant endpoint in the IPMN oncologic spectrum. Malignant lesions may represent around 25% of all resected IPMN specimens and fall into two distinct histologic subtypes. The tubular subtype imitates the appearance and behavior of pancreatic ductal adenocarcinoma, whereas the colloid subtype is characterized by large pools of extracellular mucin and follows a relatively more indolent course. Cystic pancreatic neuroendocrine tumors (pNETs) are rare variants of typical pNET and may occur anywhere on the spectrum from benign to malignant behavior. These lesions occur more commonly in women and are typically sporadic, though they may exist as part of a multiple endocrine neoplasia syndrome. Solid and cystic pseudopapillary neoplasms (SPNs) are rare heterogenous solid and cystic lesions that occur almost exclusively in younger women. These lesions represent a spectrum from premalignant to malignant (about 10%), but generally have an indolent course.
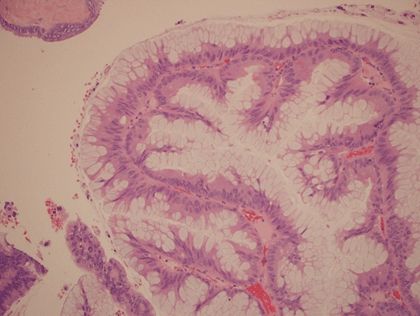
FIGURE 5.3 Hematoxylin and eosin stain histologic operative specimen demonstrating the prominent mucin-laden papillary epithelial architecture consistent with IPMN.
DIAGNOSIS
The explosion in interest surrounding cystic lesions of the pancreas is due in part to their increased recognition through improved resolution and broader use of contemporary cross-sectional imaging. In addition, there is an increased awareness of the importance of pancreatic cyst identification and characterization to promote early detection, prevention, and potential cure of pancreatic cancer. A comprehensive approach to evaluation and characterization of these lesions is critical to determine: first, the type of cystic lesion and, second, the relative oncologic risk of the lesion. Diagnosis relies on clinical, serologic, radiologic, cytopathologic, and cyst fluid (biochemical and DNA) evaluation.
Clinical
Obtaining a detailed clinical history and physical examination plays an important role in the diagnosis and differentiation of pancreatic cystic lesions. As highlighted above, the epidemiologic patterns of these cysts with regard to age and sex may aid in the development of the initial differential diagnosis (e.g., MCN occurring primarily in females). Symptoms attributable to any of these lesions may be subtle. In observational studies, the most commonly reported symptoms include epigastric pain or fullness, early satiety, and sometimes nausea. Evaluation for symptoms related to pancreatic exocrine and endocrine dysfunction is also important. Compression or occlusion of the pancreatic ductal system secondary to a cystic lesion may result in a spectrum of exocrine pancreatic dysfunction and ultimately failure. Symptoms of exocrine insufficiency may initially present as bloating and flatulence, but ultimately may progress to steatorrhea, malabsorption, and weight loss. Pancreatic duct obstruction may also precipitate pancreatitis. Derangements in insulin production may lead to new-onset or worsening diabetes mellitus in some patients. As with most pancreatobiliary malignancies, the presence of jaundice and cachexia is an ominous sign, which may indicate advanced malignancy. Physical examination will typically be somewhat low yield in these lesions. These patients rarely present with reproducible epigastric tenderness on exam, but a palpable abdominal mass may be present in the setting of larger lesions.
Serologic
The use of laboratory studies in the diagnosis and workup for cystic lesions of the pancreas may be of some adjunctive value. Assay for the development of new or worsening diabetes (serum hemoglobin A1c, fasting serum glucose) as well as pancreatic enzymes (serum amylase and lipase) to assess for pancreatitis in the setting of epigastric pain and nausea should be performed. Additionally, serum tumor markers for pancreaticobiliary malignancy, particularly cancer antigen (CA) 19-9, should be checked, as this has been shown to correlate with presence of invasive disease in the setting of IPMN. Elevation of serum alkaline phosphatase has been correlated with malignancy in pancreatic head cysts well prior to elevation of bilirubin. As of yet, there are no other viable serologic biomarkers for diagnosis or determination of malignant potential of pancreatic cystic lesions.
Radiologic
Cross-sectional imaging is the workhorse for the initial diagnosis and characterization of pancreatic cysts. Although debate exists as to their relative value, computed tomography (CT) and magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP) are the two primary noninvasive imaging modalities utilized for characterization these lesions.
Regardless of the modality utilized, certain radiologic characteristics of pancreatic cystic lesions may suggest a particular etiology. Two elements, with rare exception, that are predictive of IPMN are ductal connection and multifocality. These two features are extremely rare in other cystic lesions. A central stellate scar is a classic finding for SCN, and mural calcifications may often be present in (but are not pathognomonic of) MCN (Fig. 5.4). Finally, in the setting of malignant degeneration, cystic lesions of the pancreas on cross-sectional imaging may demonstrate features of invasion into extrapancreatic organs, vascular structures, or the biliary tree. Peritoneal and hematogenous metastases may also be detected in this setting.

FIGURE 5.4 MCN of the pancreas with the associated mural calcification seen on CT.
Dual-phase intravenous contrast-enhanced computed tomography (CT) scan is the mainstay for initial diagnosis and characterization of pancreatic cysts. Many pancreatic cysts (up to 30%) will actually be identified as incidentally detected lesions on CT scan performed for other indications. Current high-resolution CT scan technology allows for very accurate characterization of these lesions. Most cystic lesions will appear hypodense with respect to the surrounding pancreatic parenchyma on CT. It is critical to obtain thin (1 mm) cuts through the pancreas as smaller lesions are easily overlooked with less detailed imaging.
Magnetic resonance cholangiopancreatography (MRCP) is another noninvasive imaging modality that has gained wide acceptance as important adjunct in characterizing pancreatic cysts. The ability to obtain a detailed pancreatic ductogram (Fig. 5.5) may provide the clinician with information regarding ductal connection (MRI is two to three times more sensitive than CT scan alone) and may be more accurate in delineating subtle main pancreatic duct (MPD) involvement. Some authors suggest that MRCP is superior in defining IPMN type and extent and routinely employ this technique in preoperative planning and surveillance strategies.
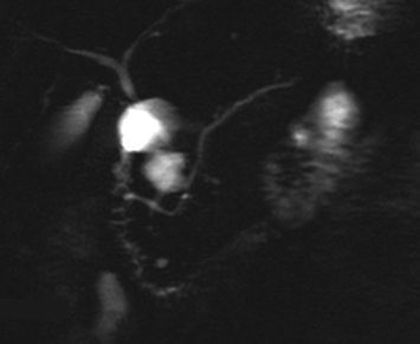
FIGURE 5.5 MRCP illustrating the grapelike morphology of a branch-type IPMN with an obvious ductal connection.
Positron emission tomography (PET) scan has been examined as an adjunctive imaging study to determine the presence of 18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree